How trauma affects health and fitness: Is it the reason your client can’t make progress?
We first envisioned an article about trauma a few years ago.
Over and over, we’d seen clients who checked out when they ate. Or shut down during workouts.
Or who raged when we made a relatively innocuous nutritional suggestion. (Like, “Consider eating slowly today.”)
Or who panicked. Disappeared. Became distressed. Got paralyzed.
Or seemed unable to cope with overwhelming urges to eat, restrict, purge, binge drink, or do a variety of other unhelpful behaviors.
As their coaches, we looked for individual explanations.
And we found them.
Painful childhoods with abusive or absent adults. Sexual assault. Emotional neglect. Substance abuse. Military service. Displacement. Miscarriages. Natural disasters. Grief and loss.
But today more than ever, it’s apparent that trauma of all kinds can negatively affect client progress.
Racism, homophobia, poverty, sexism, ableism, transphobia, fatphobia.
Unsafe neighborhoods and communities. Lack of power and resources.
Violence, abuse, and bullying from the people who are supposed to protect them—partners, police, workplaces, health systems, schools, the government.
Economic uncertainty. A global pandemic.
No wonder many of us are having a hard time managing our eating, exercise, and self-care.
Yet remarkably: We still have the capacity to change and thrive.
To that end, this article aims to help—by providing insights and tools that you, as a nutrition, fitness, or health coach, can use to appropriately support clients who are struggling with trauma.
+++
This article is about eating and exercise. But it’s also much bigger than that.
As humans, we’re called on to help make the world a better place. And to stand as advocates for all people harmed by suffering, injustice, and abuse.
At Precision Nutrition, we support not just the “physical health” of our clients, but their deep health: nurturing all the things that make a complete human.

That’s because each domain of deep health—physical, emotional, mental, environmental, relational, and existential—affects all other domains.
And trauma? It can have negative and long-lasting effects on any of these domains, making it difficult for clients to experience meaningful progress in their health and fitness.
That’s where you come in.
As a nutrition, fitness, or health coach, it’s outside your scope of practice to ask clients directly about trauma.
But sometimes clients will tell you about traumatic experiences. Or they might do or say things that just don’t seem to add up.
Understanding how trauma manifests can help explain why clients often do puzzling or apparently unhelpful things, such as overeat when they’re also desperate to lose weight or be healthier.
Or neglect their own health and wellbeing even if they take great care of everyone else.
You should know how to respond and support these clients, because—unfortunately—trauma can happen to anyone, and it’s more common than many people realize.
Growth can happen for these clients, even in the face of overwhelming suffering. Humans are astonishingly resilient.
Being a trauma-aware coach can help you:
- understand people and their challenges, which will lead to more effective, productive coaching relationships
- understand why some clients behave “irrationally” or struggle with their eating and exercise habits
- identify strategies that can help clients get unstuck
- avoid re-traumatizing people, which is part of being a good person (and is probably smart for your business, too)
- recognize when a client needs additional support—such as a referral to a therapist—to work through trauma
++++
What is trauma?
Trauma is anything that overwhelms our existing resources and ability to cope.
How is trauma different from stress?
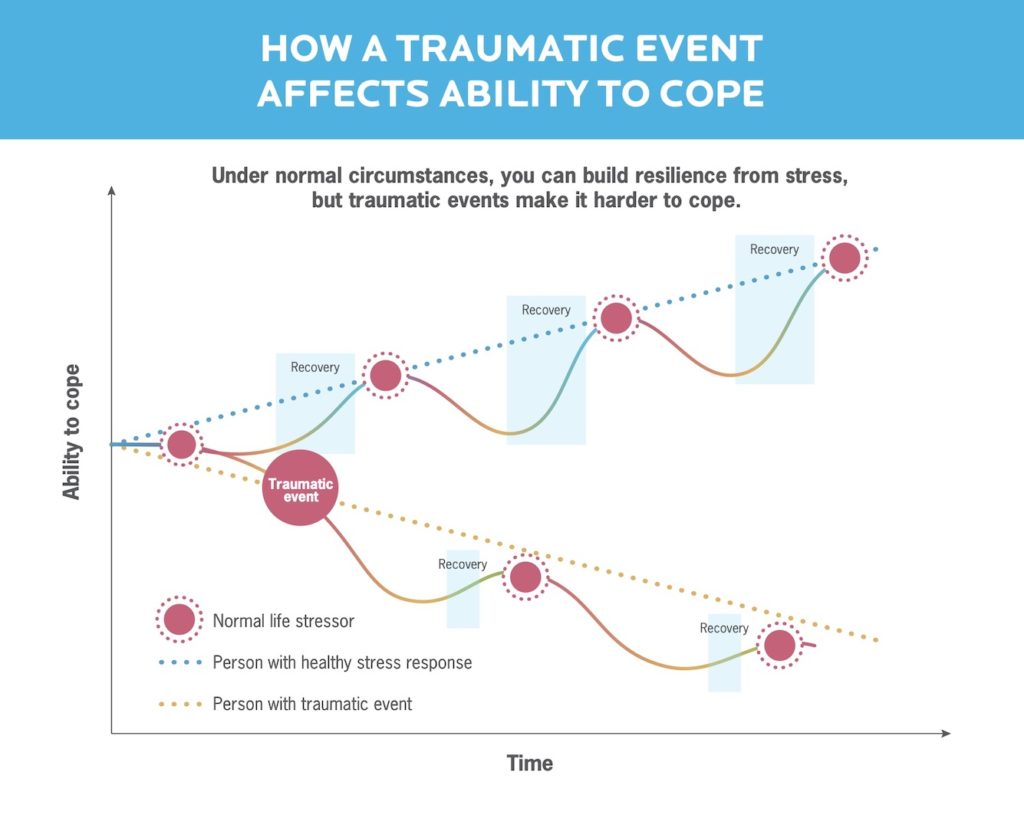
When we experience stress of any type, the body enters an alarm phase. In a normal situation, we eventually recover and get back to our baseline, or maybe even come away stronger and more resilient.
But with trauma, we experience the stressor so intensely that we’re unable to go through all the steps we need to recover. We end up worse off than where we started.
Trauma-inducing stressors can come from many different areas of our lives.
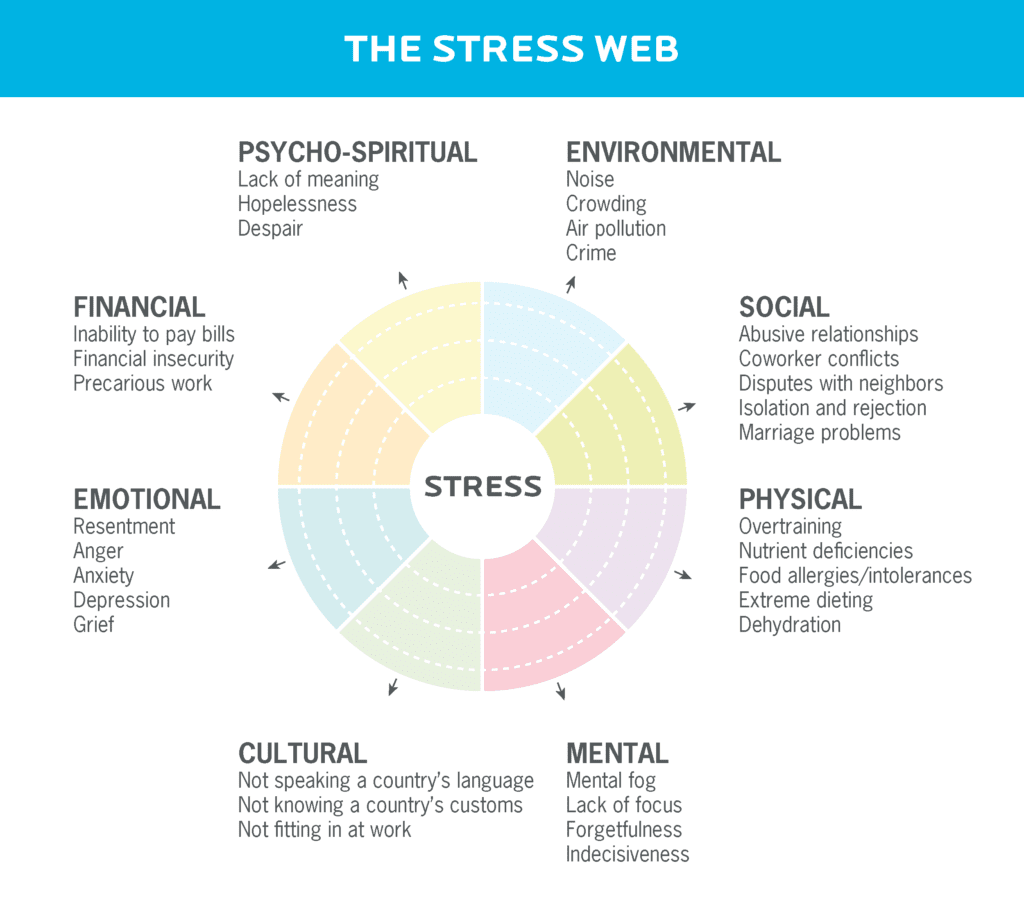
There are several types of trauma with varying degrees of severity, but they all can affect our health, wellbeing, and ability to care for ourselves.
Big-T trauma
Most people associate the word “trauma” with events like sexual assault, living or serving in a war zone, physical violence, or being in a car crash.
Because such experiences are extremely damaging and objectively terrible, psychologists refer to these as big-T trauma.
Usually, people know if they’ve experienced this type of trauma, although they may not be aware of its far-reaching effects.
Little-t trauma
Other times, traumatic events may seem like “no big deal” objectively, but they still leave a strong and lasting impression.
Little-t trauma refers to the more prevalent indignities, insecurities, injuries, and paper cuts of life.
- The experience may be something “minor” that hits in a vulnerable moment, like a parent who was largely absent during your teen years.
- Or it might be something deeply unfair or angering that happens over and over, like systemic racism or homophobia.
Little-t trauma can have lasting effects too. Many people experience it without ever recognizing it as “trauma.”
Collective trauma
We can also experience trauma as a group.
Collective trauma is a psychological effect that destabilizes the foundation of a society or group.1
Bombings, natural disasters, wars, famines, and pandemics are all obvious examples of events that can result in collective trauma.
Collective trauma can also come from violence, abuse, and indignities perpetrated against a specific group. This can happen cumulatively over time.
For example, the imposition of colonialism and residential schools on indigenous people in many countries such as Canada, the US, and Australia has had lasting generational effects.
People living through the collapse of a political regime, or in a general state of heightened awareness of violence—for instance, in a military state where they see guns on a daily basis—also suffer collective trauma.
(People may experience this type of trauma somewhat differently from individual trauma. Although it may feel less personal, trauma is trauma.)
Importantly, we don’t have to experience trauma directly in order to be affected.
For example:
- Parents may feel traumatized after a school shooting, even if their child doesn’t go to the school where the shooting happened.
- People who are alive in 2020 may have not experienced slavery directly, but the social scars of it are still “alive.”
This type of trauma can last for generations in our collective memories, and the meaning we find in these memories often goes on to shape society.
Intergenerational trauma
Trauma can be passed down through families in many ways.
First, if a person has experienced trauma, their behavior towards their child may change.
A parent or caregiver may repeat the traumatizing behavior they experienced, perpetuating the cycle.
Or, they may be so deep in their own coping mechanisms—such as abusing alcohol—they’re unable to provide for their child materially and/or emotionally.
Clients dealing with intergenerational trauma may tell you that their first issues with food appeared early in life when they felt scared, alone, small, angry, or otherwise distressed by what was happening in their families.
Second, the effects of trauma can be passed down via what’s known as transgenerational epigenetics.
Trauma can actually change how our DNA is packaged, and thus how our genes are expressed.
So traumatized people may give birth to babies who are epigenetically (i.e., biologically) predisposed towards mental or physical health challenges, increased inflammation, and/or more chronic disease.2,3,4,5,6,7,8
The most famous example is from research on the descendants of Holocaust survivors, which showed changes to genes in both parents and children.9,10 Other research has correlated a legacy of slavery with elevated stroke risk in African-American populations living in the southeastern United States.11
Similar effects have been observed in other marginalized populations (and in animal research), but this is considered an emerging area of science.12
Trauma isn’t “fact-based,” but perception-based and response-based.
A person’s subjective experience of an event or situation determines whether it was traumatic, regardless of how major or minor it seems.
Let’s say Fatima and Sonal both burned themselves on hot stoves when they were kids.
Neither of them remembers it that well, but they had similar experiences: Mom freaked out. They had to go to the hospital to treat the burn.
For Fatima, the experience wasn’t traumatic. She was upset and scared in the moment, but in the days that followed, she recovered. It didn’t leave any more of an imprint than skinning her knee on the playground.
For Sonal, the experience was traumatic. She already felt vulnerable because her dad wasn’t around, and her mom was always super stressed and working overtime to make ends meet. Though she hardly thinks about it now, the burn left a mental mark.
Now, as an adult, Sonal is wary of cooking. She doesn’t really know why.
She has stories to explain why she doesn’t cook. She’s busy. The stove just kind of seems… complicated. Or something.
But what made the experience traumatic was the context—not the burn itself.
Trauma is probably more prevalent than data indicates.
But here’s what we know: About 60 percent of men and 50 percent of women experience at least one significant trauma in their lives.13
Women are more likely to experience sexual assault and child abuse, while men are more likely to experience physical assault, combat, accidents, and disasters.14 Men are also more likely to witness death or injury.
Privilege and power are protective.
People from marginalized groups—such as people from racialized minority groups, immigrants and refugees, LGBTQI* people, people experiencing poverty, and so on—are much more likely to experience trauma.
But many people who’ve had big-T trauma don’t report it. And certainly most people who’ve suffered little-t trauma don’t.
What would they say?
- “I’d like to report my coworker being a racist or sexist a-hole?”
- “I’d like to report my mother being emotionally unavailable to me during a crucial point in my development?”
- “I’d like to report I only go out when it’s daylight so I won’t get harassed?”
- “I’d like to report a hot, corrosive rush of shame from something someone said, even though they weren’t even talking to or about me?”
For many folks, these types of events are just “how things are.” As famous feminist Gloria Steinem said about sexual harassment and assault in the 1960s and 70s, “We didn’t even have a word for it. We called it ‘life.’”
Many Precision Nutrition Coaching clients—and very likely many of yours, if you’re a coach—are dealing with the effects of trauma.
This can affect their eating and exercise behaviors, their self-care choices, and their ability to regulate their emotions.
Trauma affects how we eat, move, and live.
Although trauma manifests differently in different people, we tend to see common patterns.
Trauma changes our brains.
Often, trauma affects how a person behaves, defines themselves, and communicates with others.
Here’s what that might look like in interactions with clients:
They struggle to identify emotions, needs, and/or physical sensations. For instance, when you ask, “How do you know when you’re hungry?” or “Does that hurt?”, or “How are you feeling?”, they might say they’re not sure.15
They don’t seem to have the best memory. If you ask, “What was food like when you were little?”, or “What time did you eat dinner as a kid?”, they might not remember. They “forget things” like their daily coaching practices.
They often get stuck or paralyzed. The “freeze response” immobilizes us. Clients may say they feel unable to act, they avoid things, and/or they feel powerless. “I don’t know what happened, I just found myself eating… ”
Their story of themselves is deeply negative. “I hate myself. I’m a failure. I’m doomed. I can’t do anything right.” It’s hard for them to imagine that anything could be different or better.
They have a bigger reaction than expected. Seemingly mundane exchanges trigger fight/flight/freeze. Let’s say you suggest that your client try adding protein to their breakfast. They, in turn:
- Get super angry (fight)
- Walk away from the conversation (flight)
- Become very quiet or even completely disengage (freeze)
You might be shocked at what appears to be an over-reaction, but this is a deeply ingrained human response to fear and danger.
They always want to please you. This client might agree to literally every nutrition strategy you suggest. Eventually, it becomes clear they’re not implementing them. It just feels safer to go along with your ideas than to explain why it won’t work for them.
This is called fawning behavior. It’s often learned and employed by victims of abuse: By making themselves as invisible and agreeable as possible, they’re trying to protect themselves from further trauma.
Post-Traumatic Stress Disorder: A deeper look
Sometimes, traumatic events result in Post-Traumatic Stress Disorder, or PTSD. We don’t know exactly why, but PTSD is most likely to occur in women16, military veterans17, and people who already have one or more traumas in their past.18
PTSD manifests in a couple of ways:
1. It can disorganize our sense of time, place, and space.
This affects how we remember a traumatic experience—often making it seem like the event is happening right now—and setting off a series of psychological and physiological responses such as dissociation, panic, and fight/flight/freeze.19
2. It affects how well we can reintegrate the traumatic event.
When something terrible happens, we may dis-integrate, or fall apart. To heal, we need to “re-integrate” the experience into our life and make meaning from it.
With PTSD, that reintegration never happens. Victims are left with persistent, long-standing cognitive, neurological, psycho-emotional disorganization, that we cannot, without treatment, resolve.
Trauma changes our physical health.
People with trauma may struggle with physical issues including:
● Hormonal problems, like an overactivated hypothalamic-pituitary-adrenal (HPA) axis, a hormonal feedback loop that’s exquisitely sensitive to things like energy availability and stress.
When the HPA axis is hyperactivated, sex hormones, cortisol, and even brain neurotransmitters can get out of whack. The body may sound an alarm or simply shut the factory down.20
● Elevated inflammation, seen in biomarkers such as C-reactive protein and inflammatory cytokines, perhaps due to an overactivated HPA axis.21,22
This may be a reason childhood trauma is associated with a higher risk of health issues like heart disease, cancer, liver disease, and more.23
People with trauma may also have more chronic illnesses, particularly autoimmune disorders such as rheumatoid arthritis, psoriasis, chronic fatigue, inflammatory bowel disease (IBD), and allergies.24
● Unexplained pain, like long-standing, nagging pain or tightness that doesn’t seem to have a cause.
Maybe your client’s been X-rayed, MRI’d, CAT-scanned, and seen by every specialist. There’s no sign of injury. But the pain, restriction, and physical limitation persists.
Interestingly, the cumulative effect of stress, HPA axis/hormone dysfunction, and inflammation can actually increase pain perception.25,26 You know how things just hurt more when you’re stressed out? This is part of the reason why.
Stressed and hurting: The Bohr effect and pain
When we’re physically stressed—such as during an intense workout—we tend to inhale quickly and forcefully. Our exhales also get faster.
When we do this, it strips carbon dioxide (CO2) from the bloodstream.
This is an important bodily response. It helps the body dispose of the waste products generated by exercise, and enables us to deliver fresh oxygen to our muscles.
This dynamic relationship between blood CO2 and blood oxygen concentration is known as the Bohr effect.27
But if you’re sitting still and something stressful happens, you may experience the same shift in your breathing—deep inhales, short exhales. (Imagine a person hyperventilating during a panic attack.)
Except because you’re sitting still, there’s no increased oxygen demand in your muscles. If this happens frequently over time the following sequence of events can occur:
- You’ll have reduced CO2 in your bloodstream.
- Reduced CO2 in your blood ultimately reduces the amount of oxygen in your muscles.
- This alters the way you produce adenosine triphosphate (ATP), which is what muscles use for energy.
- Changes to ATP production alter how muscles contract and relax, increasing baseline tension.
- Because your muscles can’t fully relax, you may experience chronic tightness.
This tightness is particularly common in postural muscles, such as the ones found in the lower back, neck, and shoulders. So in addition to increased pain perception, people dealing with trauma may also experience pain due to chronic muscle tightness.
The good news?
The tightness caused by dysfunctional breathing patterns can be alleviated, in part, by learning to breathe more efficiently.
In particular, practicing longer exhales can be very helpful in delivering more oxygen to the muscles, which helps them relax.
To learn more about breathing drills and why they work, jump down to helping clients learn self-regulation.
Trauma can change our nutrition, exercise, and health habits.
When people struggle with their behavior around food and fitness for years or decades, particularly with obesity or patterns of disordered eating, there’s a pretty good chance that something happened to them. And it doesn’t even have to be something “big.”
Clients with a trauma history may:
- Overeat and/or binge.28 Losing themselves in a binge can shut out the world for a while.
- Compensate after they feel they’ve overeaten. They may purge, or over-exercise, or fast.29 The endorphins released in a punishing workout, or from bingeing and purging, may provide a temporary high.
- Control and restrict their eating. In fact, they may alternate between this and losing control.30
- Come up with strict “rules” with harsh consequences. Like “I must work out two hours a day or else I’m a lazy walrus.”
- Do things that seem confusing or contradictory. Like going on a diet in the morning and binge eating in the evening. Or keeping trigger foods around to “test themselves,” even though they often “fail.”
- “Check out” or get “brain fog” around food. Like “I don’t know what happened, I sort of woke up and the bag of chips was empty.” Or, “I get paralyzed when I try to decide what to do. It’s just overwhelming.” Or, “I guess I’m just not motivated.”
The more intense the trauma in a person’s life, and/or the more frequent it’s been, the more likely they are to have physical symptoms and/or maladaptive behaviors, thoughts, and beliefs.
One study tracked the relationship of BMI over time, correlating it to trauma history. The graph tells an interesting story.
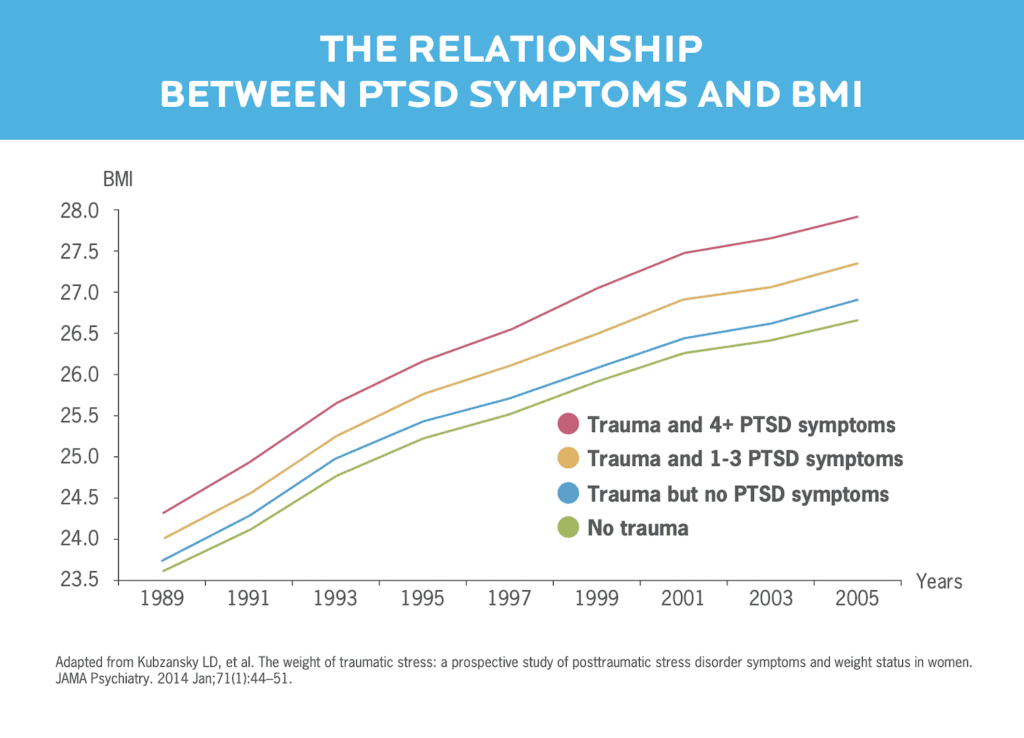
The more PTSD-type symptoms a person had, the more likely they were to gain weight over time.
Another study looked at the relationship between exercise tolerance and childhood abuse.
Researchers found that women who’d been abused were more likely to avoid exercise because the higher heart rate and feeling “amped up” evoked the same feelings of anxiety and fear they’d experienced earlier in their lives.32
Trauma can also change us for the better.
As human beings, we can feel about 50 different things at once and not have them be inconsistent. We’re complex.
We can feel horrible because of post-traumatic stress but still be growing.
A person might lose everything but then have that “screw it” moment where they reevaluate their life and decide to dump some crap and clutter overboard. That’s one type of post-traumatic growth.
Post-traumatic growth is when we change and evolve in good and healthy ways as a result of trauma.
It often involves finding meaning in our pain. For instance, we may vow to help others in similar situations.
It can help to think of post-traumatic growth like kintsugi, a type of Japanese pottery made from broken ceramics. Artists use precious metals to put the pieces back together, and the repaired version is considered more beautiful and desirable than the original item—especially because the process takes quite a bit of time.
If you know how to recognize trauma in your clients, you might just be able to help them take steps towards making repairs. They may find meaning in what they’ve been through. Or even discover the beauty in rebuilding.
7 ways to help your clients break the cycle.
#1: Familiarize yourself with the signs of trauma.
Good news: You’ve already accomplished this by reading this article!
Importantly, the reasoning behind understanding the signs of trauma isn’t so you can diagnose your clients. As noted earlier, that’d be a job for a qualified therapist. So unless you happen to be one of those, it’s important to stay within your scope of practice as a coach.
But knowing what trauma looks like helps you:
- support your clients and avoid retraumatizing them
- avoid feeling frustrated when client behavior doesn’t seem to make sense
- know when it’s time to refer out to a mental health practitioner
Educate yourself and be prepared to handle difficult material sensitively.
If you want to dig into some further reading, consider these resources:
- The Body Keeps the Score by Bessel van der Kolk, MD
- Post Traumatic Slave Syndrome by Joy DeGruy, PhD
- When The Body Says No and In The Realm of Hungry Ghosts, both by Gabor Mate, MD
- The Body Remembers: The Psychophysiology of Trauma and Trauma Treatment by Babette Rothschild, MSW
#2: Affirm the validity of people’s feelings.
Don’t say “It’s no big deal.” It obviously is to them.
Don’t say “I understand completely.” You don’t.
Don’t say “Get over it.” They can’t, not without help.
Don’t avoid the topic and say nothing because it’s too icky or you don’t know what to say.
Instead, say: “I’m sorry for what you’re going through. Thank you for trusting me with this. I am here to listen and support you.”
#3: Maintain and respect boundaries.
Care about your clients but don’t become a caregiver for them. Know where you can help, and where you can’t.
Here at Precision Nutrition, we’ve come up with a code of ethics for coaches, as well as best practices for maintaining healthy boundaries with clients.
Familiarize yourself with these concepts. They’re important for all clients, but they can help establish a sense of safety with traumatized clients.
You should pay special attention to:
- Using open, non-confrontational body language to give off friendly, non-threatening vibes.
- Using a warm yet professional tone of voice.
- Establishing consent early and often if your coaching methods require physical touch.
That last point is key.
It may feel awkward to bring it up, which is why a lot of coaches skip it. Don’t be one of those people.
The guidelines here are simple:
- Any time you want to touch a client, ask: “Is it okay if I touch you here, like this?” Use hand gestures to indicate what you mean.
- Before you remove your hand(s) from a supportive position (such as helping to position their rib cage during a pushup), ask: “Is it okay if I remove my hands now?”
It might sound strange to ask about removing your hands, but doing so without asking can make a person with body-related trauma feel especially vulnerable.
Asking these questions gives a client ownership over what happens to their body. They can control who touches them, how, and when. And that’s how it should always be.
#4: If your client is open, explain the trauma response.
If you have a client who has disclosed trauma, it can help to share what happens during the trauma response with them.
Why? People are often really confused about what’s happening to them.
It’s a lightbulb moment to learn that what they’re experiencing is a physiological response to something that happened in their past.
It’s well worth taking the time to explain that their brain and body have learned a pattern of responding, and so what’s happening to them and their health struggles are not their fault.
When your client blanks out in front of the fridge, it’s not because they don’t have enough willpower or they bought the “wrong” groceries.
This realization can make a huge difference for the client and how they define themselves. They realize they’re not a bad person or lazy or that they can’t control themselves. They’re just repeating a pattern they learned long ago.
#5: Help clients learn to calm themselves.
This is a powerful skill that anyone can learn or teach. Here are three approaches to try.
Balloon breathing
“There’s a physical relationship between how you breathe and what your brain is telling your body to do,” says Craig Weller, CPT, PN Master Coach and resident exercise specialist. Exhaling triggers parasympathetic input from the brain, slightly slowing the heart rate.
By extending your exhale, you spend a little bit more time in the parasympathetic, calm-down state.
Try a longer, slower out-breath, like blowing up a balloon:
- Breathe out slowly for several seconds. You can count 1-2-3-4-5 if you like.
- Pause for a few seconds. Again, feel free to count.
- Then, consciously relax, and let the in-breath happen naturally.
- Repeat.
Core-engaged breathing
Putting your spine in different positions has differing effects on your nervous system via physical pressure receptors called ganglia.
Extending your spine (think upward dog in yoga) activates sympathetic receptors, turning on “fight or flight” mode.
Conversely, flexing your spine (think fetal position, or a puppy taking a nice nap), takes pressure off the spinal ganglia, producing a calming effect. Long exhales with your ribs and core in this position relieves the pressure even more.
Two versions of core-engaged breathing to consider: fetal position breathing and ribs-down breathing.
Grounding exercises.
These can help a client who struggles with “checking out” by drawing their attention to concrete physical sensations.
Examples of grounding exercises:
- Focus on the sensation of your feet on the floor
- Feeling the barbell in your hands
- Smell the rubber of the medicine ball you’re holding
#6: Have a referral network at the ready.
There may be times when you can’t (and shouldn’t) address all your clients’ needs on your own.
Keep some recommendations for mental health practitioners handy. These can be people you know in your community, or ones you’ve identified through research. If you’re not sure where to start, here are some ideas:
- If you live in the United States or Canada, check out Psychology Today’s Find A Therapist directory.
- In Europe, try the European Association for Body Psychotherapy or the European Association for Psychotherapy.
- In Australia, try Australia Counselling.
- Or Google your location with keywords like “trauma therapy.”
Make a list, and keep it handy. Try our referral worksheet.
Remember, referring out doesn’t mean you stop seeing your client. You can continue to support them in their health habits while they get specialized support in another area.
#7: Serve, but preserve.
There’s no getting around it. This is heavy stuff.
You may yourself have experienced trauma and be dealing with very similar issues as your client.
A lot of people choose to go to a coach over a therapist, for a variety of reasons—from not having health insurance to stigma around mental health.
While you should maintain your boundaries with clients and stay within your scope of practice, there are going to be times when you’re the only person a client can confide in.
But therapists have something coaches don’t always have in place: supervision and advisors. They regularly get together with other therapists to discuss cases, share advice, and get support.
As a coach, you can do something similar by talking with like-minded coaches regularly. Get that support.
Difficult subject matter can be draining. So make sure to harge your own battery.
Because your health is important, too.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Hirschberger G. Collective Trauma and the Social Construction of Meaning. Front Psychol. 2018 Aug 10;9:1441.
2. St-Hilaire A, Steiger H, Liu A, Laplante DP, Thaler L, Magill T, et al. A prospective study of effects of prenatal maternal stress on later eating-disorder manifestations in affected offspring: preliminary indications based on the Project Ice Storm cohort. Int J Eat Disord. 2015 Jul;48(5):512–6.
3. Fuller-Rowell TE, Homandberg LK, Curtis DS, Tsenkova VK, Williams DR, Ryff CD. Disparities in insulin resistance between black and white adults in the United States: The role of lifespan stress exposure. Psychoneuroendocrinology. 2019 Sep 1;107:1-8.
4. Allen AM, Thomas MD, Michaels EK, Reeves AN, Okoye U, Price MM, Hasson RE, Syme SL, Chae DH. Racial discrimination, educational attainment, and biological dysregulation among midlife African American women. Psychoneuroendocrinology. 2019 Jan 1;99:225-35.
5. Conway-Phillips R, Dagadu H, Motley D, Shawahin L, Janusek LW, Klonowski S, Saban KL. Qualitative evidence for Resilience, Stress, and Ethnicity (RiSE): A program to address race-based stress among Black women at risk for cardiovascular disease. Complementary Therapies in Medicine. 2020 Jan 1;48:102277.
6. Farmer HR, Wray LA, Haas SA. Race, gender, and socioeconomic variations in C-reactive protein using the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci [Internet]. 2020 Feb 17; Available from: http://dx.doi.org/10.1093/geronb/gbaa027
7. Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: Patterns and prospects. Health Psychology. 2016 Apr;35(4):407.
8. Hidayat K, Du X, Shi B-M, Qin L-Q. Foetal and childhood exposure to famine and the risks of cardiometabolic conditions in adulthood: A systematic review and meta-analysis of observational studies. Obes Rev. 2020 May;21(5):e12981.
9. Yehuda R, Daskalakis NP, Bierer LM, Bader HN, Klengel T, Holsboer F, et al. Holocaust Exposure Induced Intergenerational Effects on FKBP5 Methylation. Biol Psychiatry. 2016 Sep 1;80(5):372–80.
10. Jawaid A, Roszkowski M, Mansuy IM. Transgenerational Epigenetics of Traumatic Stress. Prog Mol Biol Transl Sci. 2018 Jun 11;158:273–98.
11. Esenwa C, Ilunga Tshiswaka D, Gebregziabher M, Ovbiagele B. Historical slavery and modern-day stroke mortality in the United States Stroke Belt. Stroke. 2018 Feb;49(2):465-9.
12. Jawaid A, Mansuy IM. Inter- and transgenerational inheritance of behavioral phenotypes. Current Opinion in Behavioral Sciences. 2019 Feb 1;25:96–101.
13. VA.gov | Veterans Affairs [Internet]. [cited 2020 May 27]. Available from: https://www.ptsd.va.gov/understand/common/common_adults.asp
14. Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006 Nov;132(6):959–92.
15. Franzoni E, Gualandi S, Caretti V, Schimmenti A, Di Pietro E, Pellegrini G, et al. The relationship between alexithymia, shame, trauma, and body image disorders: investigation over a large clinical sample. Neuropsychiatr Dis Treat. 2013 Feb 18;9:185–93.
16. Kimerling R, Weitlauf JC, Iverson KM, Karpenko JA, Jain S. Gender issues in PTSD. Handbook of PTSD: Science and practice, 2nd ed. 2014;2:313–30.
17. Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War veterans: a population-based survey of 30,000 veterans. Am J Epidemiol. 2003 Jan 15;157(2):141–8.
18. Neuner F, Schauer M, Karunakara U, Klaschik C, Robert C, Elbert T. Psychological trauma and evidence for enhanced vulnerability for posttraumatic stress disorder through previous trauma among West Nile refugees. BMC Psychiatry. 2004 Oct 25;4:34.
19. Center for Substance Abuse Treatment (US). Exhibit 1.3-4, DSM-5 Diagnostic Criteria for PTSD. Substance Abuse and Mental Health Services Administration (US); 2014.
20. Monteleone, Alessio Maria, et al. Childhood trauma and cortisol awakening response in symptomatic patients with anorexia nervosa and bulimia nervosa. International Journal of Eating Disorders Volume 48, Issue 6, pages 615–621, September 2015.
21. Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016 May;21(5):642–9.
22. Baldwin JR, Arseneault L, Caspi A, Fisher HL, Moffitt TE, Odgers CL, et al. Childhood victimization and inflammation in young adulthood: A genetically sensitive cohort study. Brain Behav Immun. 2018 Jan;67:211–7.
23. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998 May;14(4):245–58.
24. Song H, Fang F, Tomasson G, Arnberg FK, Mataix-Cols D, Fernández de la Cruz L, et al. Association of Stress-Related Disorders With Subsequent Autoimmune Disease. JAMA. 2018 Jun 19;319(23):2388–400.
25. Hannibal KE, Bishop MD. Chronic stress, cortisol dysfunction, and pain: a psychoneuroendocrine rationale for stress management in pain rehabilitation. Phys Ther. 2014 Dec;94(12):1816–25.
26. Blackburn-Munro G, Blackburn-Munro RE. Chronic pain, chronic stress and depression: coincidence or consequence? J Neuroendocrinol. 2001 Dec;13(12):1009–23.
27. Grossman P. Respiration, stress, and cardiovascular function. Psychophysiology. 1983 May;20(3):284–300.
28. Backholm K, Isomaa R, Birgegård A. The prevalence and impact of trauma history in eating disorder patients. European Journal of Psychotraumatology. 2013;4:10.3402/ejpt.v4i0.22482. doi:10.3402/ejpt.v4i0.22482.
29. Brewerton TD, Dansky BS, O’Neil PM, Kilpatrick DG. The number of divergent purging behaviors is associated with histories of trauma, PTSD, and comorbidity in a national sample of women. Eat Disord. 2015 Feb 26;23(5):422–9.
30. Madowitz J, Matheson BE, Liang J. The relationship between eating disorders and sexual trauma. Eat Weight Disord. 2015 Sep;20(3):281–93.
31. Kubzansky LD, Bordelois P, Jun HJ, Roberts AL, Cerda M, Bluestone N, et al. The weight of traumatic stress: a prospective study of posttraumatic stress disorder symptoms and weight status in women. JAMA Psychiatry. 2014 Jan;71(1):44–51.
32. Dale, Lourdes P., et al. Abuse History is related to Autonomic Regulation to Mild Exercise and Psychological Wellbeing. Appl Psychophysiol Biofeedback (2009) 34:299–308. DOI 10.1007/s10484-009-9111-4
If you’re a coach, or you want to be…
Learning how to coach clients, patients, friends, or family members through healthy eating and lifestyle changes—in a way that supports the deep health of the whole person—is both an art and a science.
If you’d like to learn more about both, consider the Precision Nutrition Level 1 Certification. The next group kicks off shortly.
What’s it all about?
The Precision Nutrition Level 1 Certification is the world’s most respected nutrition education program. It gives you the knowledge, systems, and tools you need to really understand how food influences a person’s health and fitness. Plus the ability to turn that knowledge into a thriving coaching practice.
Developed over 15 years, and proven with over 100,000 clients and patients, the Level 1 curriculum stands alone as the authority on the science of nutrition and the art of coaching.
Whether you’re already mid-career, or just starting out, the Level 1 Certification is your springboard to a deeper understanding of nutrition, the authority to coach it, and the ability to turn what you know into results.
[Of course, if you’re already a student or graduate of the Level 1 Certification, check out our Level 2 Certification Master Class. It’s an exclusive, year-long mentorship designed for elite professionals looking to master the art of coaching and be part of the top 1% of health and fitness coaches in the world.]
Interested? Add your name to the presale list. You’ll save up to 30% and secure your spot 24 hours before everyone else.
We’ll be opening up spots in our next Precision Nutrition Level 1 Certification on Wednesday, October 7th, 2020.
If you want to find out more, we’ve set up the following presale list, which gives you two advantages.
- Pay less than everyone else. We like to reward people who are eager to boost their credentials and are ready to commit to getting the education they need. So we’re offering a discount of up to 30% off the general price when you sign up for the presale list.
- Sign up 24 hours before the general public and increase your chances of getting a spot. We only open the certification program twice per year. Due to high demand, spots in the program are limited and have historically sold out in a matter of hours. But when you sign up for the presale list, we’ll give you the opportunity to register a full 24 hours before anyone else.
If you’re ready for a deeper understanding of nutrition, the authority to coach it, and the ability to turn what you know into results… this is your chance to see what the world’s top professional nutrition coaching system can do for you.
The post How trauma affects health and fitness: Is it the reason your client can’t make progress? appeared first on Precision Nutrition.
Source: Health1
