If you’ve heard of billionaire Bryan Johnson, you’ve likely encountered the phrase “bio age testing.”
Johnson, the subject of the Netflix documentary Don’t Die, says he’s on a quest to achieve the lowest possible “biological age” (also known as bio age).
He reportedly spends millions each year on anti-aging treatments—dozens of daily supplements, weekly acid peels for his skin, injections to boost collagen production, hyperbaric oxygen therapy, and plasma infusions extracted from his 17-year-old son’s body.
To determine what’s working, Johnson has undergone numerous tests to assess his bio age. Johnson says these tests show his age is now 5.1 years younger than when he embarked on his anti-aging quest.
Apparently, he’s aging in reverse.
Granted, not everyone’s buying it. A New York Times exposé, for example, claims Johnson’s biological age, in reality, has increased by 10 years.1
Still, Johnson’s “don’t die” crusade is gaining traction.
Bio age tests are a frequent topic on popular podcasts by Peter Attia, Joe Rogan, and Andrew Huberman. Google “bio age testing” and you’ll see dozens of ads for mail-order blood or urine testing kits that claim to reveal your biological age, pace of aging, and more. With prices tumbling into affordability, it’s natural to wonder…
Should you or your client sign up for bio age testing?
If so, which test is best? Just as importantly, what should you do with the information?
In this story, you’ll learn:
- Five FREE ways to assess your overall health and pace of aging—from the comfort of your own home
- Doctor-approved bio age tests you may have already done without realizing it
- The research behind commercial bio age tests, and whether they’re worth your money
- The two biggest mistakes people make when chasing health and longevity
What is your bio age?
Your biological age (bio age) refers to how your cells function. It’s not necessarily the same as your chronological age, which refers to the number of candles on your birthday cake.
For example, let’s say Chang, a 50-year-old man, works at a desk, spends his free time in front of the TV, lives in the most polluted city in the world, eats a candy bar for lunch, and smokes. On the other hand, Jabari, a different 50-year-old man, hits the gym several times a week, lives in the mountains, doesn’t smoke, relishes his five servings of veggies a day, meditates, and spends most evenings in his garden.
Genetics aside, you’d be wise to wager that Jabari’s bio age is younger than Chang’s.
How do these tests measure bio age?
Bio age testing kits measure one or more biological markers of aging, also known as biomarkers.
For example, some tests focus on the size of your telomeres, the protective caps at the ends of chromosomes. Others measure DNA methylation, a physiological process that chemically alters DNA.
Once a company isolates and measures these markers from your blood or urine, it plugs the bio data into a formula that calculates your bio age.
However, if you see a doctor with any regularity, you’re likely already tracking some biomarkers of aging. For example, biomarkers such as blood pressure, cholesterol levels, and blood glucose can help predict your risk of future cardiovascular disease, a leading cause of premature death.
What’s the point of biomarker testing?
Biomarker testing can help you monitor your wellness proactively rather than waiting for disease symptoms to appear.
For some, it also serves as a motivator. If you learn you have the bones of someone 20 years older, this may give you the nudge you need to start strength training consistently.
In addition, biomarkers provide objective data, allowing you to track and evaluate various health-related actions quantitatively. By monitoring your blood pressure, you might learn that consistent exercise helps, but your late-afternoon energy drink does the opposite.
5 FREE biomarker tests
You don’t have to be a billionaire (or even a millionaire) to track biomarkers of aging.
In this section, we’ll cover several massively underappreciated, scientifically validated tests you can use to gain insight into your bio age—for FREE.
Before scientists developed high-tech blood-based bio age tests, researchers used these free tests to calculate the pace of aging in the people they studied.
FREE biomarker test #1: Get off the floor
People who are fitter and stronger tend to live longer.2
That’s because muscles do more than just move us around. They also secrete anti-inflammatory substances, help to regulate blood sugar, slow cellular aging, protect the lining of the arteries, and more. All this helps reduce the risk of age-related diseases, such as type 2 diabetes, high blood pressure, and heart disease, a phenomenon we explore in our article, The New Science of Muscle.
Related to strength, your ability to balance is also key. If you’re middle-aged or older and can’t stand on one foot for at least 10 seconds, your risk of dying in the next seven years is double that of someone who can stand for longer, according to a study of 1,700 people.3
The Sitting-Rising Test (SRT) is one way to assess both strength and balance at the same time.
People with low scores on this test have a higher risk of dying from cardiovascular disease, according to a 12-year study of 4,200 adults between the ages of 46 and 75.4
 How to measure it
How to measure it
Lower yourself to the floor with your legs in a crisscross position. Then, with your legs in the same position, stand back up. As you stand, notice if you must use a part of your body—hand, shin, knee—as leverage.
To score yourself, start with 10 points. Then, for each body part you used to stand, deduct a point. Subtract a half point if you became unsteady or lost your balance.
Keep in mind that this (and other tests) serve as a proxy for your fitness. A low score indicates that your balance and coordination, muscle strength and power, and mobility may all require some attention.
FREE biomarker test #2: Squeeze a ball
Like the SRT test, your grip strength provides insight into your overall fitness. If the muscles in your hands are weak, the muscles throughout your body are more likely to be weak, too.
Poor grip strength can also predict future muscle weakness. In one study, people with a weak grip were more likely to walk slowly and be unable to rise from a chair, complete rigorous housework, or climb a flight of steps 25 years later.5
Low grip strength has also been associated with:6
- Low bone mineral density
- Increased risk of falls
- Poor nutritional status
- Depression
- Poor sleep, cognitive function, and/or quality of life
- Increased risk of heart disease, cancer, and premature mortality
According to one study, grip strength was a better indicator of longevity (or lack thereof) than blood pressure.7
 How to measure it
How to measure it
Grab a standard tennis ball, and squeeze as hard as you can, for as long as you can.
If you can manage 15 to 30 seconds before your grip fatigues, you’re doing fine. Ninety seconds puts you well above average—anything over 90 ranks you solidly in the upper-third percentile.
If you’re below 15, keep in mind that this test is also just one indicator of your overall strength. (And squeezing balls to improve grip strength without training the rest of your body is unlikely to make significant improvements in your overall health and fitness.)
A hand-held dynamometer—available for use at most occupational therapists’ and some gyms—can also test grip strength. (If you’re willing to shell out some cash, you can buy your own for somewhere between $100 and $500.)
FREE biomarker test #3: Stand on one foot
An ability to balance on one foot for an extended period can help reduce your risk of falls, one of the leading causes of injury-related death among older adults.
In addition, many different bodily systems—the eyes, inner ear, skeletal muscles, and brain—must work together to help you stay upright.
Conditions like diabetes, heart disease, and cancer can all affect balance. As a result, an inability to stand on one foot can serve as a warning sign for eroding health and fitness.8
 How to measure it
How to measure it
Stand near a wall or chair for safety. Keep your eyes open and hands on your hips. Then, lift your dominant leg and start timing yourself. Once you put your foot down, stop the clock. Repeat the test with your non-dominant leg.
Once you have your times, compare them to the following averages, from a study out of Duke University, to see how you did compared to your age-matched peers.9
| Age | Seconds on one leg (males) | Seconds on one leg (females) |
|---|---|---|
| 30-39 | 59 | 56 |
| 40-49 | 56 | 55 |
| 50-59 | 42 | 48 |
| 60-69 | 40 | 38 |
| 70-79 | 27 | 25 |
| 80+ | 13 | 11 |
FREE biomarker test #4: How you feel
Sometimes you know why you’re tired, such as the morning after binge-watching the last few episodes of a thriller. Once you catch up on your sleep, the weariness lifts.
That’s not the same thing as fatigue, which describes persistent exhaustion that worsens over time and interferes with life. In addition to feeling physically tired, someone who’s fatigued feels mentally dull and emotionally exhausted.
Think of fatigue as an early sign that something’s off, especially if you don’t know the cause.
Let’s say you’ve already ruled out the usual suspects like too much caffeine, dehydration, too much alcohol, medication side effects, chronic stress, or too much or too little exercise. What’s left is likely a sleep disorder or a developing health problem such as anemia, obesity, depression, cancer, or diabetes, to name a few.
If you’re 60 or older, fatiguability—or how worn out you feel after an activity—can also predict longevity.
According to research out of the University of Pittsburgh Medical Center, the higher someone scores in fatiguability, the higher their risk of death in the future.10 Other research has linked high fatiguability with declines in gait speed, walking ability, and other tests of fitness.11
 How to measure it
How to measure it
To measure fatigability, use a tool called the Pittsburgh Fatigability Scale. Using a 0 (no fatigue) to 5 (extreme fatigue) scale, rate how fatigued you think you would feel after completing the following activities:
| Activity | Duration | Score (0 to 5) |
|---|---|---|
| Leisurely walking | 30 minutes | |
| Brisk or fast walking | 1 hour | |
| Light household activity | 1 hour | |
| Heavy gardening or yard work | 1 hour | |
| Watching television | 2 hours | |
| Sitting quietly | 1 hour | |
| Moderate-to-high intensity strength training | 30 minutes | |
| Participating in a social activity | 1 hour | |
| Hosting a social event for 60 minutes | 1 hour | |
| High intensity activity | 30 minutes | |
| Add all scores: | ||
If you score less than 15, you’re doing well. Scores between 15 and 24 are a warning sign. Anything 25 and above is regarded as severe, and worth mentioning to your healthcare professional.12
FREE biomarker test #5: Body composition
Despite popular belief, both too little and too much body fat can influence health for the worse, as we explore in our infographic, Is body fat good or bad for you?
| Too much fat raises the risk for: | Too little muscle raises risk for: |
|---|---|
| Heart disease | Heart disease |
| High blood pressure | High blood pressure |
| Cancer | Cancer |
| Fatty liver disease | Stroke |
| Insulin resistance | Insulin resistance |
| Type 2 diabetes | Faster cellular aging |
| Inflammation | Inflammation |
| Joint distress | Depression and anxiety |
| Sleep apnea | Falls and loss of balance |
Your muscle mass also plays a role, which is why someone’s body composition matters more than their weight.
The gold standard methods that estimate body composition—underwater weighing, air displacement (Bod Pod), and dual-energy X-ray absorptiometry (DEXA)—certainly aren’t free.
However, a recent study determined that a good old-fashioned (and cheap) tape measure can provide a comparably accurate estimate of body composition.13
 How to measure it
How to measure it
To use a tape measure to keep track of your body fat percentage, measure:
- The widest part of your neck
- The narrowest part of your waist (For some people, this will be at the navel. For others, it might be slightly above the navel)
- The widest part of your hips
Ensure the tape is snug but not so tight that it cuts into the skin. Once you have your measurements, plug those numbers—along with your age, sex, height, and weight—into our FREE Body Fat Calculator, which will take it from there.
Doctor-approved biomarker tests
Depending on where you live in the world, the following tests may not be free. However, as part of routine preventative care, your insurance might cover them.
Doctor-approved test #1: Blood panel
If your primary care doctor recommends yearly blood work, it’s for good reason.
By keeping tabs on several blood markers, you can see if your health is trending toward type 2 diabetes or heart disease, both leading causes of premature mortality.
Many blood markers can also be influenced relatively quickly (within 6 to 12 weeks) through lifestyle changes, supplement protocols, or medications. This makes them practical tools for monitoring whether various lifestyle or medical modifications are working.
 How to measure it
How to measure it
If you’re not already doing so, consider having the following blood markers tested annually. Then, talk to your health care professional about what your numbers mean. They might use the following numbers, along with your blood pressure, to calculate a cardiovascular disease risk score.
| Blood marker | Optimal range |
|---|---|
| Total cholesterol | < 200 mg/dL* |
| LDL | < 100 mg/dL for those without heart disease < 70 mg/dL for those with a history of heart attack or stroke |
| HDL | > 60 mg/dL |
| Triglycerides | < 150 mg/dL |
| Alipoprotein B (Apo B) | < 133 mg/dL (males) < 117 mg/dL (females) |
| Lipoprotein (a) | < 30 mg/dL |
| C-reactive protein | < 2.0 mg/L** |
| Fasting glucose | < 100 mg/dL |
| Hemoglobin A1C | < 5.7% |
*Milligrams per deciliter of blood
**Milligrams per liter
Doctor-approved test #2: Bone density
When researchers study healthy super-agers aged 90 and older, strong bones are one of their defining features.14
That may be because, like muscles, bones are live organs that secrete substances that may be beneficial to overall health and longevity.15
For example, bones secrete osteocalcin, a hormone that plays a role in bone remodeling. When osteocalcin circulates in the body, it’s thought to play a role in everything from helping muscles to produce ATP to regulating brain neurotransmitters.
Because of these varied roles, it’s thought that, as bones wear away, osteocalcin levels drop, contributing to many age-related health problems, including diabetes, low muscle mass, and cognitive issues.16 17 (At least, that’s the theory. Most of this research has been done on mice.)
Osteocalcin aside, loss of bone density can, of course, lead to fractures, which can increase your risk of death for up to 10 years after a break.18
It’s especially important to keep tabs on bone health if you’re in any of these high-risk categories:
- You’re female and went through menopause before age 45.
- You’ve been sedentary most of your adult life.
- You take medications such as diuretics or stomach-acid blockers, which are linked with an increased risk of osteoporosis.
- You have a history of nicotine use or excessive alcohol consumption.
- You have a medical condition, such as diabetes or thyroid disease, that raises your risk.
- You have a family history of osteoporosis.
 How to measure it
How to measure it
Dual-energy X-ray absorptiometry (DEXA) scans are a type of X-ray that measures the amount of bone mineral content packed into a square centimeter of bone.
Insurance often won’t cover these scans for people younger than 65 unless there’s a documented risk of developing osteoporosis. Out of pocket, the average cost is about $300.
When you receive your DEXA results, you’ll see a T-score that represents how your bone density compares to the average bone density of a young adult with peak bone mass. A T-score of +1.0 to -1.0 means you have normal bone mineral density for someone your age. Anything below -1.0 means you might have osteopenia (low bone mineral density) or osteoporosis (porous bones that are prone to fracture).
Commercial bio age tests
If you have some money to burn, you can learn an awful lot about your body.
Here, you’ll find a quick run-down on some of the more high-tech tests you can get and what they can tell you.
However, before we get into the details, we want to point out a few caveats:
 Biological age can vary over time, and by organ. Someone may go through a period of accelerated aging—saying, during a period of intense stress—then their rate of aging may slow as they focus more on recovery. Additionally, organs can age at different rates. For example, someone with heart disease may have a relatively older heart than their kidneys. (Not all tests measure individual organ age, but it’s becoming more common.)
Biological age can vary over time, and by organ. Someone may go through a period of accelerated aging—saying, during a period of intense stress—then their rate of aging may slow as they focus more on recovery. Additionally, organs can age at different rates. For example, someone with heart disease may have a relatively older heart than their kidneys. (Not all tests measure individual organ age, but it’s becoming more common.)
 Commercial tests won’t always accurately reflect the changes you’re making. Until more research supports the reliability of these tests, evaluate your behaviors over isolated test results. If you’re eating more fruits and veggies, exercising more consistently, managing stress, and otherwise slaying the healthy lifestyle department, don’t sweat your results. Focus on doing the things we know improve health.
Commercial tests won’t always accurately reflect the changes you’re making. Until more research supports the reliability of these tests, evaluate your behaviors over isolated test results. If you’re eating more fruits and veggies, exercising more consistently, managing stress, and otherwise slaying the healthy lifestyle department, don’t sweat your results. Focus on doing the things we know improve health.
 If a company pairs your test results with a hard sell for a proprietary and expensive supplement protocol, be wary. It’s better to share and discuss your results with a trusted health professional than take health advice from a profit-seeking stranger over the internet.
If a company pairs your test results with a hard sell for a proprietary and expensive supplement protocol, be wary. It’s better to share and discuss your results with a trusted health professional than take health advice from a profit-seeking stranger over the internet.
Commercial test #1: DNA methylation
DNA methylation is a biological process that chemically alters DNA. Because the rate of methylation accelerates with aging, it can be used to estimate someone’s biological age and life expectancy, finds research.19 20 21
The Horvath Clock and DunedinPACE both measure specific biomarkers that can be used to better understand someone’s methylation rate. Scientists developed these tests to help other scientists study how various lifestyle factors, environmental exposures, and medicines affect aging. They didn’t develop the tests as a way for the average person to pinpoint their biological age. (Which hasn’t stopped companies from selling DNA methylation testing kits to the public.) They cost about $300.
If you decide to get one of these tests, keep in mind your results won’t give you a complete picture of your health and longevity. Aging typically occurs at varying rates throughout the body. Your liver might age faster than your heart or brain, for example. So if you measure DNA methylation in your blood, that’s all you know about. Put another way, a DNA methylation test isn’t a substitute for your annual wellness checkup or blood work.
Commercial test #2: Telomere analysis
Telomeres—the protective caps on the ends of chromosomes—wear away with age. The length of a telomere can predict how many times a specific cell can divide before dying.
Abnormally short telomeres are associated with several genetic diseases. For this reason, when physicians suspect someone might have inherited a genetic disease, they’ll order a specific type of telomere test—the flow-FISH test—to measure the telomere length in all the cells in a blood sample.22 23
It’s more debatable whether telomere tests can predict aging in healthy people.
Just as importantly, the telomere test marketed to the public, known as the qPCR telomere test, isn’t used in research or medicine. These $100 tests are fine if you’re merely curious—just don’t base health and fitness decisions on your results.
Commercial test #3: VO2 Max
For years, only elite athletes cared about VO2 max, which describes the maximum amount of oxygen that your body can use during exercise.
More recently, however, some experts have suggested that VO2 max can serve as a measure for athletes and non-athletes alike to track the rate at which their bodies are aging.
People with high VO2 max tend not only to be more physically fit but also less likely to develop heart disease, diabetes, cancer, or stroke.24 25 26 27
In an observational study that followed the health outcomes of 5,107 Danish men over 46 years, men with above-average V02 max during middle age lived an average of five years longer than men with below-average V02 max. Each unit increase in VO2 max was associated with a 45-day increase in longevity. The researchers suggested VO2 max may more accurately predict all-cause mortality than high cholesterol, obesity, high blood pressure, and insulin resistance.28
You might think of V02 max as a canary and your aging body as a coal mine.
As you age, your chest wall becomes more rigid, the muscles that surround the lungs weaker, and the oxygen-carrying blood vessels calcified and less elastic. The heart also squeezes with less force, max heart rate drops, muscle mass and strength decline, the mitochondria in cells and muscles lose their effectiveness, among other differences.
In addition to raising your risk for many different diseases, these changes can also affect VO2 max, which tends to decline 10 percent per decade starting around age 30.29 30
In the past, the only way to reliably measure VO2 max was in a fitness lab.
You would wear a metabolic mask and a heart monitor while you ran or cycled to exhaustion. The mask collected your expired carbon dioxide and monitored how much oxygen you sucked into your lungs. This lab-based testing is still the most accurate way to measure V02 max as well as other key fitness metrics such as:
- Max heart rate, or the highest number of times your heart can beat per minute during exercise
- Ventilatory threshold 1, or the point during exercise when the body switches from mainly using fat for fuel to using a combination of fat and glucose or glycogen (stored glucose) for fuel.
- Ventilatory threshold 2, or the point where your body moves away from aerobic metabolism (which uses oxygen) to anaerobic metabolism (which doesn’t use oxygen).
- Tidal volume is the amount of air inhaled or exhaled during each breath
Depending on where you live, you might be able to get your VO2 max tested for around $150.
However, if you don’t have access to a VO2 max clinic, three somewhat less accurate options exist.
 The 1-mile walk test
The 1-mile walk test
Wear a heart rate monitor as you walk one mile on a flat surface, such as a treadmill or running track. As soon as you complete the mile, record your heart rate and walk time. Then, plug it into the following formula to calculate your VO2 max:
132.853 — (0.0769 × Weight) — (0.3877 × Age) + (6.315 × Sex) — (3.2649 × Time) — (0.1565 × Heart rate)
If that feels like too much math, you can also use a free online tool.
 The smartwatch test
The smartwatch test
Many smartwatches will estimate your VO2 Max for you based on information the watch gathers from your workouts, sex, and age. Compared to in-office testing, smart watches can over- or underestimate V02 max, especially in people who are very out of shape or extremely fit.31
Because of this, you don’t necessarily want to use your smart watch measurement to determine your current state of health. However, it can help you to see trends. For example, does your VO2 estimate drop after a few weeks of skipping your usual spin class? If so, that’s good information to have.
 The PR test
The PR test
Fitness performance correlates with longevity. If you’re getting faster at running a certain distance or can go a longer distance than before, you’re getting fitter and increasing your chances of living a long, healthy life.
One way to test this: the 12-minute run test, also known as the Cooper test. (This is a validated way to estimate VO2 max—and shows about a 90 percent correlation with lab-based measurements.)
Here’s how it works:
Run as fast as you can on a flat surface, such as a treadmill set at a 1 percent incline or running track, for 12 minutes. After 12 minutes, record your distance. Then, plug it into one of the following formulas to calculate your VO2 max.
| Distance in Miles | Distance in Kilometers | |
|---|---|---|
| VO2 Max = | (35.97 x distance in miles) – 11.29 | (22.351 x distance in kilometers) – 11.288 |
In lieu of doing math, you can also use a free online calculator.
How to change your biological age
Try to think of the information you gather about your body as just that—information.
It’s not a moral judgment of who you are as a person.
Just as importantly, it’s not a permanent situation.
- If you’re weaker than other people your age, you can grow stronger.
- If your cholesterol or blood glucose levels are high, you can take steps to lower them.
- If your body is aging faster than your birthdays, consider exploring key lifestyle changes that may help turn the situation around.
You have options. However, most people make two big mistakes when it comes to longevity-related lifestyle changes.
Mistake #1: Ignoring evergreen, big-impact strategies
It’s the simple, boring, “I’ve heard this a million times before” health practices that, when done consistently, add up to a long, healthy life.
We’re talking about things like…
- Eating more minimally processed foods and fewer ultra-processed foods
- Consuming more brightly colored fruits and veggies
- Moving your body regularly
- Getting enough rest and sleep
- Enjoying community, time in nature, and other activities that make life meaningful
- Keeping alcohol intake moderate
- Not using tobacco
- Wearing sunscreen
- Flossing
And that’s just a partial list.
According to thousands of studies, people who practice these and other high-impact strategies not only live longer, but also live better. They’re stronger, happier, and less likely to spend their later years disabled or in pain.
(If you’d like to see where you stand when it comes to big impact health and longevity strategies, check out our FREE Longevity Assessment.)
However, when it comes to health, fitness, and longevity, many people pursue options with minimal impact (at best). They reach for the latest, trendy supplement rather than taking steps to quit smoking, as just one example.
Here’s the thing: Big rock strategies require changes in behavior. If daily physical activity were as easy as popping a pill, walkers and cyclists would clog up the streets in your neighborhood.
(It’s precisely this reason why so many people need the support of a certified health coach who has undergone training in the science of behavior change.)
Mistake #2: Not turning data into action
The data gathered from biomarker aging tests can give you a sense of control.
However…
Data, in isolation, doesn’t lead to a longer life.
Gathering data without changing your behavior is like checking your reflection in the mirror, seeing spinach wedged between your incisors, and leaving it there.
You need to remove the spinach for the mirror check to be worthwhile.
Biomarker testing is the same.
If you don’t use your bio data to inform behavior change, you’re wasting your money and time.
Consider your biomarker data as a baseline or starting point.
Then, use it to assess whether various lifestyle changes or medical interventions are moving you closer to your goal of living a longer, healthier life.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Grind K. How Bryan Johnson, Who Wants to Live Forever, Sought Control via Confidentiality Agreements. The New York Times [Internet]. 2025 Mar 21 [cited 2025 Jul 15]; Available from: https://www.nytimes.com/2025/03/21/technology/bryan-johnson-blueprint-confidentiality-agreements.html
2. Strasser B, Volaklis K, Fuchs D, Burtscher M. Role of dietary protein and muscular fitness on longevity and aging. Aging Dis. 2018 Feb 1;9(1):119–32.
3. Araujo CG, de Souza E Silva CG, Laukkanen JA, Fiatarone Singh M, Kunutsor SK, Myers J, et al. Successful 10-second one-legged stance performance predicts survival in middle-aged and older individuals. Br J Sports Med. 2022 Sep 1;56(17):975–80.
4. Araújo CGS, de Souza e Silva CG, Myers J, Laukkanen JA, Ramos PS, Ricardo DR. Sitting–rising test scores predict natural and cardiovascular causes of deaths in middle-aged and older men and women. Eur J Prev Cardiol. 2025 Jun 18;zwaf325.
5. Dodds RM, Kuh D, Sayer AA, Cooper R. Can measures of physical performance in mid-life improve the clinical prediction of disability in early old age? Findings from a British birth cohort study. Exp Gerontol. 2018 Sep;110:118–24.
6. Bohannon RW. Grip strength: An indispensable biomarker for older adults. Clin Interv Aging. 2019 Oct 1;14:1681–91.
7. Leong DP, Teo KK, Rangarajan S, Lopez-Jaramillo P, Avezum A Jr, Orlandini A, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015 Jul 18;386(9990):266–73.
8. Rezaei A, Bhat SG, Cheng C-H, Pignolo RJ, Lu L, Kaufman KR. Age-related changes in gait, balance, and strength parameters: A cross-sectional study. PLoS One. 2024 Oct 23;19(10):e0310764.
9. Hall KS, Cohen HJ, Pieper CF, Fillenbaum GG, Kraus WE, Huffman KM, et al. Physical performance across the adult life span: Correlates with age and physical activity. J Gerontol A Biol Sci Med Sci. 2017 Apr 1;72(4):572–8.
10. Glynn NW, Gmelin T, Renner SW, Qiao YS, Boudreau RM, Feitosa MF, et al. Perceived physical fatigability predicts all-cause mortality in older adults. J Gerontol A Biol Sci Med Sci. 2022 Apr 1;77(4):837–41.
11. Simonsick EM, Schrack JA, Santanasto AJ, Studenski SA, Ferrucci L, Glynn NW. Pittsburgh Fatigability Scale: One-page predictor of mobility decline in mobility-intact older adults. J Am Geriatr Soc. 2018 Nov 1;66(11):2092–6.
12. Vercelli S, Zampogna E, Negrini F, Pietraroia C, D’Antona G, Papa S, et al. Cross-cultural translation, validation, and responsiveness of the Pittsburgh Fatigability Scale – Italian version (PFS-I) in a mixed-sample of older adults. BMC Geriatr. 2024 Dec 19;24(1):1016.
13. Combest TM, Khan J, Tufano JJ, Lane M, Watson NL, Altom KR, et al. Comparison of four body composition methods: Circumference measurements, eight-point bioelectrical impedance analysis up to 500 and 1000 kHz to dual-energy X-ray absorptiometry to measure body fat percentage. Mil Med [Internet]. 2024 Sep 18 [cited 2025 Jan 11]
14. Dayer SR, Mears SC, Pangle AK, Mendiratta P, Wei JY, Azhar G. Does superior bone health promote a longer lifespan? Geriatr Orthop Surg Rehabil. 2021 Aug 3;12:21514593211036231.
15. Mera P, Laue K, Wei J, Berger JM, Karsenty G. Osteocalcin is necessary and sufficient to maintain muscle mass in older mice. Mol Metab. 2016 Oct 1;5(10):1042–7.
16. Weivoda MM, Chew CK, Monroe DG, Farr JN, Atkinson EJ, Geske JR, et al. Identification of osteoclast-osteoblast coupling factors in humans reveals links between bone and energy metabolism. Nat Commun. 2020 Jan 7;11(1):87.
17. Lee NK, Sowa H, Hinoi E, Ferron M, Ahn JD, Confavreux C, et al. Endocrine regulation of energy metabolism by the skeleton. Cell. 2007 Aug 10;130(3):456–69.
18. Tran T, Bliuc D, Hansen L, Abrahamsen B, van den Bergh J, Eisman JA, et al. Persistence of excess mortality following individual nonhip fractures: A relative survival analysis. J Clin Endocrinol Metab. 2018 Sep 1;103(9):3205–14.
19. Chen BH, Marioni RE, Colicino E, Peters MJ, Ward-Caviness CK, Tsai P-C, et al. DNA methylation-based measures of biological age: meta-analysis predicting time to death. Aging (Albany NY). 2016 Sep 28;8(9):1844–65.
20. Lu AT, Quach A, Wilson JG, Reiner AP, Aviv A, Raj K, et al. DNA methylation GrimAge strongly predicts lifespan and healthspan. Aging (Albany NY). 2019 Jan 21;11(2):303–27.
21. Belsky DW, Caspi A, Corcoran DL, Sugden K, Poulton R, Arseneault L, et al. DunedinPACE, a DNA methylation biomarker of the pace of aging. Elife. 2022 Jan 14;11:e73420
22. Alder JK, Hanumanthu VS, Strong MA, DeZern AE, Stanley SE, Takemoto CM, et al. Diagnostic utility of telomere length testing in a hospital-based setting. Proc Natl Acad Sci U S A. 2018 Mar 6;115(10):E2358–65.
23. Vaiserman A, Krasnienkov D. Telomere length as a marker of biological age: State-of-the-art, open issues, and future perspectives. Front Genet. 2020;11:630186.
24. Imboden MT, Harber MP, Whaley MH, Finch WH, Bishop DL, Kaminsky LA. Cardiorespiratory fitness and mortality in healthy men and women. J Am Coll Cardiol. 2018 Nov 6;72(19):2283–92.
25. Cai L, Gonzales T, Wheeler E, Kerrison ND, Day FR, Langenberg C, et al. Causal associations between cardiorespiratory fitness and type 2 diabetes. Nat Commun. 2023 Jul 3;14(1):3904.
26. Aker A, Saliba W, Bahouth F, Naoum I, Zafrir B. Cardiorespiratory fitness and risk of cardiovascular events and mortality in middle age patients without known cardiovascular disease. J Clin Med. 2023 Nov 9;12(22):7011.
27. Prestgaard E, Mariampillai J, Engeseth K, Erikssen J, Bodegård J, Liestøl K, et al. Change in cardiorespiratory fitness and risk of stroke and death: Long-term follow-up of healthy middle-aged men: Long-term follow-up of healthy middle-aged men. Stroke. 2019 Jan;50(1):155–61.
28. Clausen JSR, Marott JL, Holtermann A, Gyntelberg F, Jensen MT. Midlife cardiorespiratory fitness and the long-term risk of mortality: 46 years of follow-up. J Am Coll Cardiol. 2018 Aug 28;72(9):987–95.
29. Kim C-H, Wheatley CM, Behnia M, Johnson BD. The effect of aging on relationships between lean body mass and VO2max in rowers. PLoS One. 2016 Aug 1;11(8):e0160275.
30. Strasser B, Burtscher M. Survival of the fittest: VO2max, a key predictor of longevity? Front Biosci (Landmark Ed). 2018 Mar 1;23(8):1505–16.
31. Caserman P, Yum S, Göbel S, Reif A, Matura S. Assessing the accuracy of smartwatch-based estimation of maximum oxygen uptake using the Apple Watch Series 7: Validation study. JMIR Biomed Eng. 2024 Jul 31;9(1):e59459.
If you’re a health and fitness pro…
When your clients are stressed and exhausted, everything else becomes a
struggle: going to the gym, choosing healthy foods, and managing cravings.
But with the right tools, you can help your clients overcome
obstacles like chronic stress and poor sleep—leading them toward the
lasting health transformations they’ve always wanted.
PN’s Level 1 Sleep, Stress Management, and Recovery (SSR) Coaching
Certification
will give you these tools. And it’ll give you confidence and credibility as a
specialized coach who can
solve the biggest problems blocking any clients’ progress. (You can
join the SSR Early Access List for our biggest discount + exclusive perks.)
The post Biological age tests: Should you get one? appeared first on Precision Nutrition.
Source: Health1
Many people with IBS would trade 10 to 15 years of life expectancy for an instant cure for their condition.
This is according to the results of a study of nearly 2,000 people with irritable bowel syndrome (IBS).1
In other research, people with IBS said they would take a medicine that carried a one percent risk of sudden death if it would cure their symptoms2—which can include urgent bouts of diarrhea, gas, or persistent constipation.
Some people with IBS experience bouts of abdominal pain they describe as worse than childbirth. These flare-ups can siphon concentration, interrupt sleep, and destroy work productivity.3
As a result, many people with IBS plan their lives around the availability of private, clean bathrooms. Fear of a sudden flare-up leads some to avoid restaurants, get-togethers, even exercising in public.
This pervading worry has a name—gastrointestinal-specific anxiety—and it can affect everything from social relationships to overall well-being. It’s also the main reason people with IBS report worse quality of life than people with other chronic conditions, including heart disease, diabetes, and end-stage kidney disease.4
If you or a client has IBS, there are ways to manage it.
PN Super Coach Sarah Maughan, certified through Monash University—a global leader in understanding the link between food sensitivities and IBS—has witnessed how lifestyle changes can prevent flare-ups, calm GI anxiety, and allow people with IBS to live the lives they want.
“My hope is for everyone with IBS to know they have options, whether that’s turning to a physician for medication and/or a health coach to learn about lifestyle changes and how to put them into action,” says Maughan.
In this article, we’ll hear more from Maughan. You’ll also learn:
- What IBS is, including why it happens and the different ways it can manifest
- What your poo can tell you about the health of your digestive tract
- Five evidence-based lifestyle changes that can improve IBS symptoms
- The best way to determine which foods trigger your or your client’s IBS symptoms (and which foods are usually “safe” to eat)
Plus, if you’re a health coach, you’ll learn how to support clients with IBS while safely staying within your scope of practice.
So, what is IBS?
Sometimes referred to as “spastic colon,” IBS is the most commonly diagnosed digestive disorder in the world, affecting about 14 percent percent of adults.5
Unlike Crohn’s and other inflammatory bowel diseases (IBD), IBS doesn’t alter the architecture of the gut. When healthcare professionals use diagnostic imaging, they find no infections, inflammation, damage to the bowel wall, or other evidence of disease.
Years ago, this lack of visible disease led many healthcare professionals to assume that IBS was purely psychological. More recently, however, this thinking has shifted.
Experts now view IBS as a functional neuro-gastrointestinal disorder.
That means the nerves between the GI tract and the brain don’t function optimally, causing the brain to deliver unnecessary pain signals and interfere with typical bowel function.
What are the symptoms of IBS?
IBS symptoms can come and go, with some people experiencing months or years of relief only to suffer a severe flare-up that can last hours to weeks.
In addition, not everyone with IBS experiences the same set of symptoms, which can make the condition challenging to diagnose.
The below illustration shows the range of IBS symptoms.

What causes IBS?
Researchers are still trying to understand why the gut functions differently in people with IBS. However, they do have a few theories.
According to one hypothesis, the nerve endings in the GI tract may be overly sensitive in people with IBS. This can lead to two different sets of symptoms.
 Hypersensitive nerves communicate pain signals to the brain, causing people with IBS to notice digestive processes that other people wouldn’t feel. Tiny gas bubbles may be severely uncomfortable for someone with IBS, for example, but not bother someone without the disorder.
Hypersensitive nerves communicate pain signals to the brain, causing people with IBS to notice digestive processes that other people wouldn’t feel. Tiny gas bubbles may be severely uncomfortable for someone with IBS, for example, but not bother someone without the disorder.
 Overreactive nerves can trigger GI muscles to contract with too much force, leading to gas, bloating, and diarrhea. If they underreact, the same muscles don’t contract forcefully enough, which slows the passage of food through the intestine and leads to constipation.
Overreactive nerves can trigger GI muscles to contract with too much force, leading to gas, bloating, and diarrhea. If they underreact, the same muscles don’t contract forcefully enough, which slows the passage of food through the intestine and leads to constipation.
Another theory blames disturbances on the gut microbiome, which helps to explain why some people develop IBS symptoms after first having a severe GI illness like the Norovirus.
How is IBS diagnosed?
If you or your client suspect IBS, see a credentialed health professional.
The symptoms of IBS overlap with several other gastrointestinal diseases and health conditions that can require medication, surgery, or medically-supervised lifestyle changes. These include infections, inflammatory bowel diseases, celiac disease, cancer, and food allergies, among others.
It’s especially important to see a medical professional if you or your client notice any of the following:
- Rapid, unintentional weight loss
- Rectal bleeding, blood in stools, or vomiting blood
- Bouts of diarrhea that disturb sleep
- Diarrhea with fever
- Continuous abdominal pain
- A sudden onset of GI symptoms after age 50
IBS Types
In addition to ruling out other GI conditions, a healthcare professional will also ask detailed questions about you or your client’s symptoms. This information allows them to pinpoint which IBS “type” you or your client might have:
- IBS-D, which means someone predominantly has diarrhea
- IBS-C, which is characterized by constipation
- IBS-M, which means someone has alternating periods of diarrhea and constipation
- IBS-U, which means someone’s symptoms don’t neatly fall into any of the above categories
You or your client’s IBS type will inform what your healthcare professional recommends.
A healthcare provider might suggest a short course of antibiotics and antidiarrheal medicine for IBS-D. On the other hand, for IBS-C, they might recommend a fiber supplement, non-habit-forming laxative, laxative-like medication, or other medicine that reduces the perception of pain and regulates bowel movements.
How to prepare for a medical appointment: Your pre-appointment checklist
In order to get the most out of the visit, you can help your client (or yourself) prepare for a healthcare appointment.
A healthcare professional will likely ask the following questions, so consider the responses beforehand:
- How long have you experienced these symptoms?
- Did anything change around the time your symptoms began? (Stress levels? Dietary habits? Recent travels?)
- Did you recently have food poisoning or gastroenteritis?
- How much fiber do you consume?
- How is your sleep quality? How many hours do you usually sleep at night?
- How often do you exercise?
Another way to prepare for your first appointment?
Well, you might not like it, but it’s a good idea to…
Look at your poo
Consider keeping a poo diary for a couple of weeks before your appointment.
In the diary, track the frequency of bowel movements and other symptoms. Use the Bristol Stool Chart (below) to take note of the quality of your poo. This information can help your healthcare professional assess whether you have IBS and which type.

(To learn more about the clues your poos can hide, read: 6 reasons you should care about your poop health)
How to help IBS: 5 strategies to support bowel health and function
In recent years, the U.S. Food and Drug Administration approved several new prescription medicines for IBS, along with a medical device that stimulates the cranial nerves behind the ear.
In addition, thousands of research papers have looked at the interaction between IBS and various lifestyle habits, with many promising findings.
Here are five evidence-based ways to reduce the symptoms of IBS (and bonus, many of them are great for enhancing overall health too).
IBS relief strategy #1: Add exercise
People with IBS who exercise regularly tend to experience fewer symptoms and flare-ups than people who don’t exercise.
When researchers asked people with IBS to walk moderately for an hour three times a week, study participants experienced significant relief from bloating and abdominal pain within 12 weeks.6
How exercise soothes IBS isn’t fully understood, though.
According to other research, exercise may reduce stress and improve mental health, which, in turn, may help improve communication between the gut and the brain.7 8
Another theory argues that exercise helps encourage the growth of health-promoting gut bacteria, which may help to break down food more efficiently and decrease inflammation.9
IBS relief strategy #2: Work on stress management
Anxiety, stress, and depression all activate stress hormones like norepinephrine (noradrenaline) and cortisol, which can:
- Amplify gut-based pain signals
- Alter the balance of bacteria in the gut (known as the gut microbiome)
- Increase intestinal permeability—potentially allowing harmful substances into the bloodstream10 11 12
Of course, stress doesn’t come with an on/off switch.
Simply telling yourself, “Stop getting so stressed out!” won’t likely help—and may even paradoxically lead to more stress.
That’s why Precision Nutrition-certified coaches like Maughan help clients learn to focus on what’s within their control—such as practicing self-compassion, or experimenting with nervous system regulators like yoga, breathing exercises, and gentle walking.
As the image below illustrates, clients can control how they perceive, respond to, and anticipate stressors—but not always the stressors themselves.
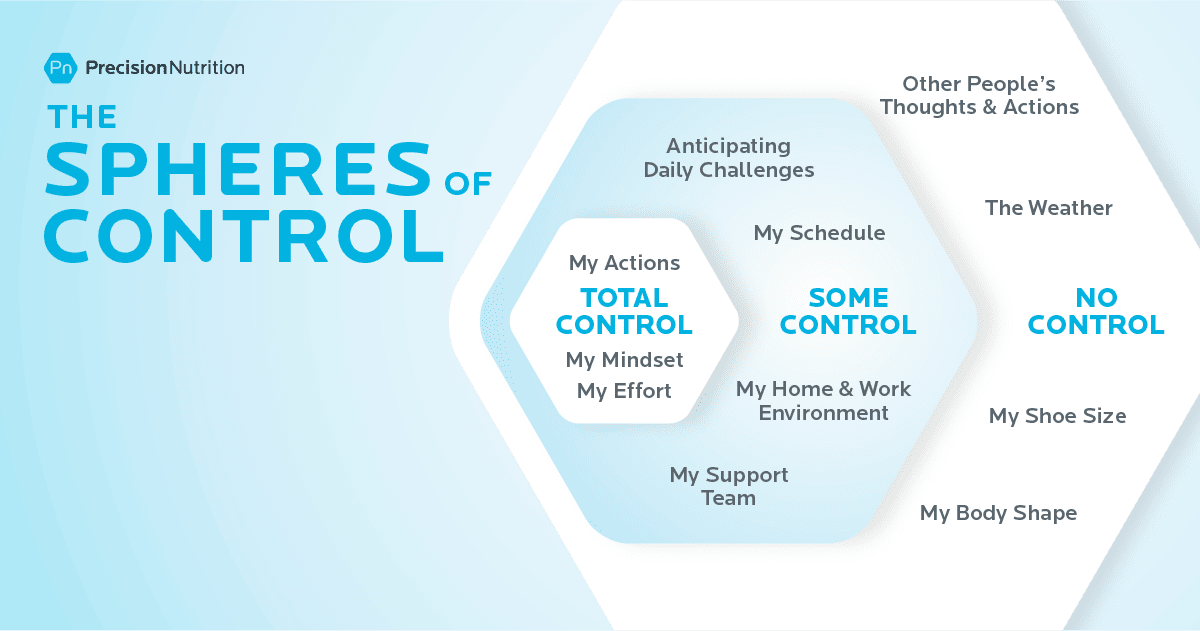
Either way, when clients focus more on what they can control and less on what they can’t, they often feel calmer and more capable.
(If you want to help a client figure out just what’s within their control—and what’s not—try out our free worksheet: Sphere of Control Worksheet)
(Assess your current stress load by taking our free quiz: Do you have a Stress Bod?)
IBS relief strategy #3: Slow your eating pace
PN coaches have long appreciated and advocated slower, more relaxed eating.
Yes, slow eating helps people fill up on fewer calories—but it also tends to help clients reduce or even eliminate GI woes like acid reflux, bloating, and pain.
For one, slower eating often translates to more chewing. In addition to mechanically mashing food into a pulp, increased chewing also allows the mouth’s digestive enzymes to pre-digest food. As a result, the stomach and intestines have to work less hard.
Plus, eating in a relaxed setting often lowers stress hormones like norepinephrine and cortisol, making it less likely that they will intensify GI pain signals.
According to Maughan, this can be especially important for young parents, as it’s not always easy to eat undistracted and peacefully when tending to little ones.
(Sounds simple, but slow eating is more challenging than people think—and a lot more impactful. Learn more: Try the slow-eating 30-day challenge.)
IBS relief strategy #4: Troubleshoot sleep problems
According to research, people with IBS experience more shallow, less restorative, and more interrupted sleep.13
Because of poor sleep quality, many people with IBS sleep more hours overall than people without IBS—yet feel less rested.
Fatigue can then set off a vicious cycle. When people don’t sleep restfully, stress hormone levels tend to be higher, which can exacerbate gut pain.14
Unrested people also tend to feel hungrier during the day. Cravings for fats and sweets also intensify, driving people to reach for the very foods more likely to trigger IBS symptoms—and wolf them down too quickly.
Stopping this cycle can be challenging.
As with stress, you can’t simply will yourself to sleep more restfully.
However, the first three strategies—exercise, stress management, and slower eating—can all help.
Some PN clients have found that consuming a smaller dinner earlier in the evening gives their bodies more time to digest before bed. Other clients tell us that a relaxing pre-bedtime routine—a few minutes of foam rolling, a guided meditation, a bath, or some journalling—tends to help.
(Find out the best practices for getting better sleep by checking out our infographic: The power of sleep)
IBS relief strategy #5: Investigate your diet
While there’s no one-size-fits-all IBS diet, experts have identified several food categories that are more likely to be problematic for many people. These include:
 Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAPs), which are a family of carbohydrate-rich foods that are poorly absorbed in the small intestine. Even in people without IBS, these foods tend to slow digestion and attract water. When gut bacteria ferment them, they produce gas, which can stretch the intestinal wall. For most, this slowed digestion and gas isn’t especially noticeable; In people with IBS, it can lead to intense pain. High-FODMAP foods include wheat, rye, barley, onions, garlic, beans, dairy, honey, cashews, some processed meats, and many fruits and vegetables. (More about FODMAPs in the next section.)
Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAPs), which are a family of carbohydrate-rich foods that are poorly absorbed in the small intestine. Even in people without IBS, these foods tend to slow digestion and attract water. When gut bacteria ferment them, they produce gas, which can stretch the intestinal wall. For most, this slowed digestion and gas isn’t especially noticeable; In people with IBS, it can lead to intense pain. High-FODMAP foods include wheat, rye, barley, onions, garlic, beans, dairy, honey, cashews, some processed meats, and many fruits and vegetables. (More about FODMAPs in the next section.)
 Caffeinated beverages and foods, especially coffee, which trigger the release of stress hormones, stimulate the production of stomach acid, increase muscle contractions in the colon, and irritate the lining of the intestine.15
Caffeinated beverages and foods, especially coffee, which trigger the release of stress hormones, stimulate the production of stomach acid, increase muscle contractions in the colon, and irritate the lining of the intestine.15
 Alcohol and spicy foods that irritate the gut.16 17
Alcohol and spicy foods that irritate the gut.16 17
 High fructose corn syrup and sugar alcohols such sorbitol and mannitol, which have been linked to gas, bloating, and diarrhea in susceptible people.18 19
High fructose corn syrup and sugar alcohols such sorbitol and mannitol, which have been linked to gas, bloating, and diarrhea in susceptible people.18 19
 Fatty, greasy foods, which can slow digestion and attract water, leading to loose stools, bloating, and gas.20 21
Fatty, greasy foods, which can slow digestion and attract water, leading to loose stools, bloating, and gas.20 21
If the idea of giving up all the foods and beverages on the above list has you in a cold sweat, know this…
Not everyone with IBS is sensitive to the same foods and beverages.
“Everyone can have different triggers,” says Maughan. “That’s why it’s so important to figure out what makes your body feel good and what doesn’t.”
Some people struggle with apples but are okay with berries. Others can drink green tea but not black. One person might be able to consume five to eight ounces of beer but not 12. A gluten-free diet may work great for some but not others.
Similarly, many people find relief by avoiding certain high-FODMAP foods. However, you may only be sensitive to some FODMAPs and not others. If so, eliminating all FODMAPs would be unnecessarily restrictive and difficult to follow consistently.
For this reason, it can be helpful to try an elimination diet to see which foods and beverages are problematic—along with the quantities you can safely tolerate, says Maughan. You’ll learn more about elimination diets in the next section.
(Want someone to walk you through exactly how to do an elimination diet? Read: How and why to do an elimination diet.)
Scope of Practice: How to coach someone with IBS
In our online coaching communities, we often see people asking some version of the following question:
“My client just told me that she has IBS. Am I allowed to continue to coach this person?”
The answer: Yes, you certainly can.
As we mentioned, Maughan specializes in helping people with digestive problems. Coaching someone with IBS is no different than coaching a client with any other nutritional goal, she says.
“Because IBS is often largely associated with what someone eats, it’s within a coach’s wheelhouse—with some caveats,” says Maughan. “You can’t diagnose your client with the condition, and you should make it clear that you’re not prescribing a diet for them. In addition, you should encourage clients to seek care from a medical professional, especially if you suspect something other than IBS is going on.”
To stay within your scope of practice, follow these do’s and don’ts.
| DO | DON’T |
|---|---|
| Encourage clients with digestive issues to visit a healthcare professional so they can get a definitive diagnosis. | Tell clients, “It sounds like you might have IBS.” |
| Share information about potential lifestyle changes, including elimination diets. Help clients run experiments that allow them to gain insight about the connection between their lifestyle, diet, and their body. | Pitch a rigid and restrictive diet as a treatment that will cure all of the client’s digestive problems. |
| Offer to work with a client’s medical team. Help the client adopt and remain consistent with the lifestyle changes their team recommends. | Contradict medical professionals by telling clients that the medical establishment always gets IBS wrong. |
| Support clients with optional recipes and other tools that help them put what they learn about their body into practice. | Create a prescriptive anti-IBS meal plan for a client to follow. |
| Encourage clients to experiment with a multi-disciplinary approach to managing IBS so they can discover the right combination of approaches that works for them. | Tell clients that you have all the answers or that they don’t need to seek medical advice or therapies. |
| Ensure clients know they can choose to make any given lifestyle change—or not. | Use force or fear to manipulate clients into following your advice. |
Elimination diets for IBS: How and when to try them
Elimination diets do what the name suggests: They exclude certain foods for a short period—usually three weeks. Then, you slowly reintroduce specific foods and monitor your symptoms for possible reactions.
Elimination diets work a lot like a science experiment that helps you identify problematic foods.
The phrase “elimination diet” may sound scary and off-putting, as if you’ll be living for months on bland food you have to slurp through a straw.
However, there are many different types of elimination diets, with some much less restrictive than others.
Here are a few versions.
Elimination diet “lite” for IBS
This is an excellent option for people who suspect they already know which foods and beverages trigger symptoms.
It goes like this: You eliminate up to four foods for several weeks. Then, slowly reintroduce them one at a time to see if your symptoms return.
Let’s say, for example, from experience, you know you feel bad whenever you eat dairy. On the lite elimination diet, you’d eliminate just dairy for three weeks. Then you’d reintroduce it to see how you feel.
Elimination Diet “medium” for IBS
If you’re unsure of how food interacts with your GI tract—but aren’t ready for a super restrictive eating plan, our Precision Nutrition elimination diet is likely the way to go.
Created by PN and approved by several registered dietitians, the plan removes many of the foods most likely to cause problems, while still including a variety of vegetables, fruits, starches, legumes, nuts, seeds, and meats, so you can continue to eat a well-balanced diet.
To learn more, download our FREE Ultimate Guide to Elimination Diets. This ebook has everything you need to be successful, including an at-a-glance chart that helps you easily follow the diet, along with recipes, meal ideas, and tip sheets.
The FODMAP diet for IBS
Over several years, researchers at Monash University in Australia have developed and extensively studied a low-FODMAP elimination diet for people with IBS.22
Unlike other types of elimination diets, the FODMAP diet is a highly specialized form of medical nutrition therapy. The FODMAP diet’s list of problematic foods (shown below) is anything but intuitive, and the reintroduction phase is more complex than other elimination diets.
As a result, if you’ve been diagnosed with IBS and suspect you have a FODMAP issue, seek the expertise of a FODMAP-certified practitioner. You can also download Monash University’s FODMAP Diet app, which will help you navigate low-FODMAP eating.
| Food Group | Low FODMAP | High FODMAP |
|---|---|---|
| Vegetables | Green beans, bok choy, green bell peppers, carrots, cucumbers, lettuce, potatoes | Artichoke, asparagus, mushrooms, onions, garlic, snowpeas, cauliflower, leeks |
| Fruits | Cantaloupe, kiwi, mandarin, orange, pineapple, firm bananas, blueberries | Apples, cherries, mango, nectarines, peaches, pears, plums, watermelon, ripe bananas |
| Dairy and Dairy Alternatives | Almond milk, brie, feta, hard cheese, lactose-free milk & yogurt | Cow’s milk and foods made from cow’s milk, soy milk |
| Protein-Rich Foods | Eggs, tofu, tempeh, most minimally-processed meats, poultry, seafood | Most legumes, some marinated and processed meats |
| Starches | Foods made from oats, quinoa, rice, spelt, or corn | Foods made from wheat, rye, and barley |
| Sweeteners | Dark chocolate, maple syrup, rice malt, table sugar | High-fructose corn syrup, honey, sugar alcohols, agave |
| Nuts and Seeds | Peanuts, pumpkin seeds, almonds, macadamias, and walnuts | Cashews, pistachios |
The power of health coaching
In isolation, more knowledge doesn’t always lead to more power.
For example, there’s a difference between knowing that dairy messes with your gut and doing something with that knowledge.
Similarly, you might know that you feel better when you eat a small dinner earlier in the evening, but you may struggle to plan your life so an early dinner happens regularly.
This is where a certified health coach can help.
“Many of my clients already have an idea of the foods that tend to cause them problems,” says Maughan, “But they’re nervous to know for sure because they fear that the knowledge will make eating more challenging.”
That’s why Maughan assures clients…
Even if you do an elimination diet and you learn your favorite food is contributing to your IBS, you don’t have to do anything with that information.
You can choose to continue to eat your favourite foods if you want, AND you can choose to avoid them when it’s really important for you not to experience IBS symptoms, she says.
“With knowledge, you have choices,” says Maughan.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- Drossman, Douglas A., Carolyn Blank Morris, Susan Schneck, Yuming J. B. Hu, Nancy J. Norton, William F. Norton, Stephan R. Weinland, Christine Dalton, Jane Leserman, and Shrikant I. Bangdiwala. 2009. “International Survey of Patients with IBS: Symptom Features and Their Severity, Health Status, Treatments, and Risk Taking to Achieve Clinical Benefit‘.” Journal of Clinical Gastroenterology 43 (6): 541–50.
- Lacy, Brian E., Kelly K. Everhart, Kirsten T. Weiser, Ryan DeLee, Sebastian Strobel, Corey Siegel, and Michael D. Crowell. 2012. “IBS Patients’ Willingness to Take Risks with Medications.” The American Journal of Gastroenterology 107 (6): 804–9.
- Farndale R, Roberts L. Long-term impact of irritable bowel syndrome: a qualitative study. Prim Health Care Res Dev. 2011 Jan;12(1):52–67.
- Trindade IA, Melchior C, Törnblom H, Simrén M. Quality of life in irritable bowel syndrome: Exploring mediating factors through structural equation modelling. J Psychosom Res. 2022 Aug 1;159(110809):110809.
- Arif TB, Ali SH, Sadiq M, Bhojwani KD, Hasan F, Rahman AU, et al. S753 meta-analysis of global prevalence and gender distribution of irritable bowel syndrome (IBS) using Rome III and IV criteria. Am J Gastroenterol. 2024 Oct;119(10S):S517–S517.
- Riezzo G, Prospero L, D’Attoma B, Ignazzi A, Bianco A, Franco I, et al. The impact of a twelve-week moderate aerobic exercise program on gastrointestinal symptom profile and psychological well-being of irritable bowel syndrome patients: Preliminary data from a southern Italy cohort. J Clin Med. 2023 Aug 17;12(16):5359.
- Royes LFF. Cross-talk between gut and brain elicited by physical exercise. Biochim Biophys Acta Mol Basis Dis. 2020 Oct 1;1866(10):165877.
- Chiang H-L, Chuang Y-F, Chen Y-A, Hsu C-T, Ho C-C, Hsu H-T, et al. Physical fitness and risk of mental disorders in children and adolescents. JAMA Pediatr. 2024 Jun 1;178(6):595–607.
- Sohail MU, Yassine HM, Sohail A, Thani AAA. Impact of physical exercise on gut microbiome, inflammation, and the pathobiology of metabolic disorders. Rev Diabet Stud. 2019 Aug 4;15(1):35–48.
- Zhang L, Wang H-L, Zhang Y-F, Mao X-T, Wu T-T, Huang Z-H, et al. Stress triggers irritable bowel syndrome with diarrhea through a spermidine-mediated decline in type I interferon. Cell Metab. 2025 Jan 7;37(1):87-103.e10.
- Schaper SJ, Stengel A. Emotional stress responsivity of patients with IBS – a systematic review. J Psychosom Res. 2022 Feb 1;153(110694):110694.
- Staudacher HM, Black CJ, Teasdale SB, Mikocka-Walus A, Keefer L. Irritable bowel syndrome and mental health comorbidity – approach to multidisciplinary management. Nat Rev Gastroenterol Hepatol. 2023 Sep 2;20(9):582–96.
- Patel A, Hasak S, Cassell B, Ciorba MA, Vivio EE, Kumar M, et al. Effects of disturbed sleep on gastrointestinal and somatic pain symptoms in irritable bowel syndrome. Aliment Pharmacol Ther. 2016 Aug 30;44(3):246–58.
- Topan R, Vork L, Fitzke H, Pandya S, Keszthelyi D, Cornelis J, et al. Poor subjective sleep quality predicts symptoms in irritable bowel syndrome using the experience sampling method. Am J Gastroenterol. 2024 Jan 1;119(1):155–64.
- Koochakpoor G, Salari-Moghaddam A, Keshteli AH, Esmaillzadeh A, Adibi P. Association of coffee and caffeine intake with irritable bowel syndrome in adults. Front Nutr. 2021 Jun 15;8:632469.
- Reding KW, Cain KC, Jarrett ME, Eugenio MD, Heitkemper MM. Relationship between patterns of alcohol consumption and gastrointestinal symptoms among patients with irritable bowel syndrome. Am J Gastroenterol. 2013 Feb;108(2):270–6.
- Esmaillzadeh A, Keshteli AH, Hajishafiee M, Feizi A, Feinle-Bisset C, Adibi P. Consumption of spicy foods and the prevalence of irritable bowel syndrome. World J Gastroenterol. 2013 Oct 14;19(38):6465–71.
- Yao CK, Tan H-L, van Langenberg DR, Barrett JS, Rose R, Liels K, et al. Dietary sorbitol and mannitol: food content and distinct absorption patterns between healthy individuals and patients with irritable bowel syndrome. J Hum Nutr Diet. 2014 Apr;27 Suppl 2(s2):263–75.
- Suez J, Korem T, Zeevi D, Zilberman-Schapira G, Thaiss CA, Maza O, et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature. 2014 Oct 9;514(7521):181–6.
- Capili B, Anastasi JK, Chang M. Addressing the role of food in irritable bowel syndrome symptom management. J Nurse Pract. 2016 May;12(5):324–9.
- Simrén M, Agerforz P, Björnsson ES, Abrahamsson H. Nutrient-dependent enhancement of rectal sensitivity in irritable bowel syndrome (IBS). Neurogastroenterol Motil. 2007 Jan;19(1):20–9.
- De Giorgio R, Volta U, Gibson PR. Sensitivity to wheat, gluten and FODMAPs in IBS: facts or fiction? Gut. 2016 Jan 1;65(1):169–78.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)
The post Over a Tenth of Your Clients Are Dealing With IBS—And Here’s How to Help appeared first on Precision Nutrition.
Source: Health1
Do you want to live longer?
If you’re like most people, your answer is probably, “Yes!”
And, you probably want to live not only a longer life, but also a healthier one.
If so, you don’t have to look very far to find claims about how to improve—no, “optimize”—your health.
Want to reverse chronic disease? Extend that youthful glow? Live to 115… or forever? Lots of fitness influencers, authors, and podcasters will tell you how to do it.
But are their ultra-specific, advanced protocols necessary—or even effective?
And just how much effort, time, and money do these methods really require?
Most of all: Are the benefits worth the trade-offs?
In this infographic, we’ll explore.
By the end of it, you’ll have clarity about how to get the health and longevity you want, while living a life you enjoy.
Click here for a fully printable version of this infographic.
And, for a complete explanation of this infographic, including a review of the latest research, check out our accompanying article: The True Cost of “Optimal” Health—Here’s what it really takes to live as long and healthy as possible.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
Dalton, Amy N., and Stephen A. Spiller. 2012. “Too Much of a Good Thing: The Benefits of Implementation Intentions Depend on the Number of Goals.” The Journal of Consumer Research 39 (3): 600–614.
Diener, Ed, and Micaela Y. Chan. 2011. “Happy People Live Longer: Subjective Well-Being Contributes to Health and Longevity.” Applied Psychology. Health and Well-Being 3 (1): 1–43.
Suarez-Lledo, Victor, and Javier Alvarez-Galvez. 2021. “Prevalence of Health Misinformation on Social Media: Systematic Review.” Journal of Medical Internet Research 23 (1): e17187.
Crawford, Cindy, Bharathi Avula, Andrea T. Lindsey, Abraham Walter, Kumar Katragunta, Ikhlas A. Khan, and Patricia A. Deuster. 2022. “Analysis of Select Dietary Supplement Products Marketed to Support or Boost the Immune System.” JAMA Network Open 5 (8): e2226040.
Crawford, Cindy, Courtney Boyd, Bharathi Avula, Yan-Hong Wang, Ikhlas A. Khan, and Patricia A. Deuster. 2020. “A Public Health Issue: Dietary Supplements Promoted for Brain Health and Cognitive Performance.” Journal of Alternative and Complementary Medicine (New York, N.Y.) 26 (4): 265–72.
White, C. Michael. 2022. “Continued Risk of Dietary Supplements Adulterated with Approved and Unapproved Drugs: Assessment of the US Food and Drug Administration’s Tainted Supplements Database 2007 through 2021.” Journal of Clinical Pharmacology 62 (8): 928–34.
Paffenbarger, R. S., Jr, R. T. Hyde, A. L. Wing, and C. C. Hsieh. 1986. “Physical Activity, All-Cause Mortality, and Longevity of College Alumni.” The New England Journal of Medicine 314 (10): 605–13.
Watts, Eleanor L., Charles E. Matthews, Joshua R. Freeman, Jessica S. Gorzelitz, Hyokyoung G. Hong, Linda M. Liao, Kathleen M. McClain, Pedro F. Saint-Maurice, Eric J. Shiroma, and Steven C. Moore. 2022. “Association of Leisure Time Physical Activity Types and Risks of All-Cause, Cardiovascular, and Cancer Mortality among Older Adults.” JAMA Network Open 5 (8): e2228510.
Jayedi, Ahmad, Ali Gohari, and Sakineh Shab-Bidar. 2022. “Daily Step Count and All-Cause Mortality: A Dose-Response Meta-Analysis of Prospective Cohort Studies.” Sports Medicine (Auckland, N.Z.) 52 (1): 89–99.
Del Pozo Cruz, Borja, Matthew Ahmadi, Sharon L. Naismith, and Emmanuel Stamatakis. 2022. “Association of Daily Step Count and Intensity with Incident Dementia in 78 430 Adults Living in the UK.” JAMA Neurology 79 (10): 1059–63.
Abou Sawan, Sidney; Nunes, Everson A.; Lim, Changhyun; McKendry, James; Phillips, Stuart M.. “The Health Benefits of Resistance Exercise: Beyond Hypertrophy and Big Weights.” Exercise, Sport, and Movement 1(1):e00001, Winter 2023.
“Falls.” n.d. Accessed May 6, 2025. https://www.who.int/news-room/fact-sheets/detail/falls.
Sadaqa, Munseef, Zsanett Németh, Alexandra Makai, Viktória Prémusz, and Márta Hock. 2023. “Effectiveness of Exercise Interventions on Fall Prevention in Ambulatory Community-Dwelling Older Adults: A Systematic Review with Narrative Synthesis.” Frontiers in Public Health 11 (August): 1209319.
Massini, Danilo A., Flávio H. Nedog, Thiago P. de Oliveira, Tiago A. F. Almeida, Caroline A. A. Santana, Cassiano M. Neiva, Anderson G. Macedo, et al. 2022. “The Effect of Resistance Training on Bone Mineral Density in Older Adults: A Systematic Review and Meta-Analysis.” Healthcare (Basel, Switzerland) 10 (6): 1129.
Park, Jung Ha, Ji Hyun Moon, Hyeon Ju Kim, Mi Hee Kong, and Yun Hwan Oh. 2020. “Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks.” Korean Journal of Family Medicine 41 (6): 365–73.
Zisko, Nina, Kjerstin Næss Skjerve, Atefe R. Tari, Silvana Bucher Sandbakk, Ulrik Wisløff, Bjarne M. Nes, and Javaid Nauman. 2017. “Personal Activity Intelligence (PAI), Sedentary Behavior and Cardiovascular Risk Factor Clustering – the HUNT Study.” Progress in Cardiovascular Diseases 60 (1): 89–95.
“Exercise or Physical Activity.” 2024. September 25, 2024. https://www.cdc.gov/nchs/fastats/exercise.htm.
Carrard, Justin, Anne-Catherine Rigort, Christian Appenzeller-Herzog, Flora Colledge, Karsten Königstein, Timo Hinrichs, and Arno Schmidt-Trucksäss. 2022. “Diagnosing Overtraining Syndrome: A Scoping Review.” Sports Health 14 (5): 665–73.
Weakley, Jonathon, Shona L. Halson, and Iñigo Mujika. 2022. “Overtraining Syndrome Symptoms and Diagnosis in Athletes: Where Is the Research? A Systematic Review.” International Journal of Sports Physiology and Performance 17 (5): 675–81.
Breuckmann, Frank, Stefan Möhlenkamp, Kai Nassenstein, Nils Lehmann, Susanne Ladd, Axel Schmermund, Burkhard Sievers, et al. 2009. “Myocardial Late Gadolinium Enhancement: Prevalence, Pattern, and Prognostic Relevance in Marathon Runners.” Radiology 251 (1): 50–57.
Wilson, M., R. O’Hanlon, S. Prasad, A. Deighan, P. Macmillan, D. Oxborough, R. Godfrey, et al. 2011. “Diverse Patterns of Myocardial Fibrosis in Lifelong, Veteran Endurance Athletes.” Journal of Applied Physiology (Bethesda, Md.: 1985) 110 (6): 1622–26.
Möhlenkamp, Stefan, Nils Lehmann, Frank Breuckmann, Martina Bröcker-Preuss, Kai Nassenstein, Martin Halle, Thomas Budde, et al. 2008. “Running: The Risk of Coronary Events : Prevalence and Prognostic Relevance of Coronary Atherosclerosis in Marathon Runners.” European Heart Journal 29 (15): 1903–10.
Müssigbrodt, A., A. Weber, J. Mandrola, Y. van Belle, S. Richter, M. Döring, A. Arya, P. Sommer, A. Bollmann, and G. Hindricks. 2017. “Excess of Exercise Increases the Risk of Atrial Fibrillation.” Scandinavian Journal of Medicine & Science in Sports 27 (9): 910–17.
Eijsvogels, Thijs M. H., Paul D. Thompson, and Barry A. Franklin. 2018. “The ‘Extreme Exercise Hypothesis’: Recent Findings and Cardiovascular Health Implications.” Current Treatment Options in Cardiovascular Medicine 20 (10): 84.
Franklin, Barry A., and Scott Billecke. 2012. “Putting the Benefits and Risks of Aerobic Exercise in Perspective.” Current Sports Medicine Reports 11 (4): 201–8.
Oteng, Antwi-Boasiako, and Sander Kersten. 2020. “Mechanisms of Action of Trans Fatty Acids.” Advances in Nutrition 11 (3): 697–708.
Souza, Russell J. de, Andrew Mente, Adriana Maroleanu, Adrian I. Cozma, Vanessa Ha, Teruko Kishibe, Elizabeth Uleryk, et al. 2015. “Intake of Saturated and Trans Unsaturated Fatty Acids and Risk of All Cause Mortality, Cardiovascular Disease, and Type 2 Diabetes: Systematic Review and Meta-Analysis of Observational Studies.” BMJ 351 (August): h3978.
Dhaka, Vandana, Neelam Gulia, Kulveer Singh Ahlawat, and Bhupender Singh Khatkar. 2011. “Trans Fats-Sources, Health Risks and Alternative Approach – A Review.” Journal of Food Science and Technology 48 (5): 534–41.
Ortega, Miguel A., Óscar Fraile-Martínez, Cielo García-Montero, Miguel Angel Alvarez-Mon, Guillermo Lahera, Jorge Monserrat, Maria Llavero-Valero, et al. 2022. “Biological Role of Nutrients, Food and Dietary Patterns in the Prevention and Clinical Management of Major Depressive Disorder.” Nutrients 14 (15): 3099.
Piao, Jingjing, Yingwei Wang, Tianqi Zhang, Jiayu Zhao, Qianyu Lv, Mengyu Ruan, Qin Yu, and Bingjin Li. 2023. “Antidepressant-like Effects of Representative Types of Food and Their Possible Mechanisms.” Molecules (Basel, Switzerland) 28 (19): 6992.
Saghafian, Faezeh, Hanieh Malmir, Parvane Saneei, Alireza Milajerdi, Bagher Larijani, and Ahmad Esmaillzadeh. 2018. “Fruit and Vegetable Consumption and Risk of Depression: Accumulative Evidence from an Updated Systematic Review and Meta-Analysis of Epidemiological Studies.” The British Journal of Nutrition 119 (10): 1087–1101.
Juul, Filippa, Georgeta Vaidean, and Niyati Parekh. 2021. “Ultra-Processed Foods and Cardiovascular Diseases: Potential Mechanisms of Action.” Advances in Nutrition (Bethesda, Md.) 12 (5): 1673–80.
Du, Shutong, Valerie K. Sullivan, Michael Fang, Lawrence J. Appel, Elizabeth Selvin, and Casey M. Rebholz. 2024. “Ultra-Processed Food Consumption and Risk of Diabetes: Results from a Population-Based Prospective Cohort.” Diabetologia 67 (10): 2225–35.
Kliemann, Nathalie, Fernanda Rauber, Renata Bertazzi Levy, Vivian Viallon, Eszter P. Vamos, Reynalda Cordova, Heinz Freisling, et al. 2023. “Food Processing and Cancer Risk in Europe: Results from the Prospective EPIC Cohort Study.” The Lancet. Planetary Health 7 (3): e219–32.
Fadnes, Lars T., Carlos Celis-Morales, Jan-Magnus Økland, Solange Parra-Soto, Katherine M. Livingstone, Frederick K. Ho, Jill P. Pell, et al. 2023. “Life Expectancy Can Increase by up to 10 Years Following Sustained Shifts towards Healthier Diets in the United Kingdom.” Nature Food 4 (11): 961–65.
Lane, Melissa M., Elizabeth Gamage, Shutong Du, Deborah N. Ashtree, Amelia J. McGuinness, Sarah Gauci, Phillip Baker, et al. 2024. “Ultra-Processed Food Exposure and Adverse Health Outcomes: Umbrella Review of Epidemiological Meta-Analyses.” BMJ (Clinical Research Ed.) 384 (February): e077310.
Rico-Campà, Anaïs, Miguel A. Martínez-González, Ismael Alvarez-Alvarez, Raquel de Deus Mendonça, Carmen de la Fuente-Arrillaga, Clara Gómez-Donoso, and Maira Bes-Rastrollo. 2019. “Association between Consumption of Ultra-Processed Foods and All Cause Mortality: SUN Prospective Cohort Study.” BMJ (Clinical Research Ed.) 365 (May): l1949.
Wolfson, Julia A., Anna Claire Tucker, Cindy W. Leung, Casey M. Rebholz, Vanessa Garcia-Larsen, and Euridice Martinez-Steele. 2025. “Trends in Adults’ Intake of Un-Processed/Minimally Processed, and Ultra-Processed Foods at Home and Away from Home in the United States from 2003-2018.” The Journal of Nutrition 155 (1): 280–92.
Wang, Dong D., Yanping Li, Shilpa N. Bhupathiraju, Bernard A. Rosner, Qi Sun, Edward L. Giovannucci, Eric B. Rimm, et al. 2021. “Fruit and Vegetable Intake and Mortality.” Circulation 143 (17): 1642–54.
Boeing, Heiner, Angela Bechthold, Achim Bub, Sabine Ellinger, Dirk Haller, Anja Kroke, Eva Leschik-Bonnet, et al. 2012. “Critical Review: Vegetables and Fruit in the Prevention of Chronic Diseases.” European Journal of Nutrition 51 (6): 637–63.
N.d. Accessed May 2, 2025. https://odphp.health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidelines.pdf.
Lee-Kwan, Seung Hee, Latetia V. Moore, Heidi M. Blanck, Diane M. Harris, and Deb Galuska. 2017. “Disparities in State-Specific Adult Fruit and Vegetable Consumption – United States, 2015.” MMWR. Morbidity and Mortality Weekly Report 66 (45): 1241–47.
Naghshi, Sina, Omid Sadeghi, Walter C. Willett, and Ahmad Esmaillzadeh. 2020. “Dietary Intake of Total, Animal, and Plant Proteins and Risk of All Cause, Cardiovascular, and Cancer Mortality: Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies.” BMJ (Clinical Research Ed.) 370 (July): m2412.
Haghighatdoost, Fahimeh, Noushin Mohammadifard, Parisa Zakeri, Jamshid Najafian, Masoumeh Sadeghi, Hamidreza Roohafza, and Nizal Sarrafzadegan. 2023. “Differences in All-Cause Mortality Risk Associated with Animal and Plant Dietary Protein Sources Consumption.” Scientific Reports 13 (1): 3396.
Chen, Zhangling, Marija Glisic, Mingyang Song, Hamid A. Aliahmad, Xiaofang Zhang, Alice C. Moumdjian, Valentina Gonzalez-Jaramillo, et al. 2020. “Dietary Protein Intake and All-Cause and Cause-Specific Mortality: Results from the Rotterdam Study and a Meta-Analysis of Prospective Cohort Studies.” European Journal of Epidemiology 35 (5): 411–29.
N.d. Accessed May 2, 2025. https://www.aicr.org/cancer-prevention/recommendations/limit-consumption-of-red-and-processed-meat/#what-the-science-says.
“Cancer: Carcinogenicity of the Consumption of Red Meat and Processed Meat.” n.d. Accessed May 2, 2025. https://www.who.int/news-room/questions-and-answers/item/cancer-carcinogenicity-of-the-consumption-of-red-meat-and-processed-meat.
Li, Chunxiao, Tom R. P. Bishop, Fumiaki Imamura, Stephen J. Sharp, Matthew Pearce, Soren Brage, Ken K. Ong, et al. 2024. “Meat Consumption and Incident Type 2 Diabetes: An Individual-Participant Federated Meta-Analysis of 1·97 Million Adults with 100 000 Incident Cases from 31 Cohorts in 20 Countries.” The Lancet. Diabetes & Endocrinology 12 (9): 619–30.
Phillips, Stuart M., Stéphanie Chevalier, and Heather J. Leidy. 2016. “Protein ‘Requirements’ beyond the RDA: Implications for Optimizing Health.” Applied Physiology Nutrition and Metabolism 41 (5): 565–72.
Houston, Denise K., Barbara J. Nicklas, Jingzhong Ding, Tamara B. Harris, Frances A. Tylavsky, Anne B. Newman, Jung Sun Lee, et al. 2008. “Dietary Protein Intake Is Associated with Lean Mass Change in Older, Community-Dwelling Adults: The Health, Aging, and Body Composition (Health ABC) Study.” The American Journal of Clinical Nutrition 87 (1): 150–55.
Hengeveld, Linda M., Jolanda M. A. Boer, Pierrette Gaudreau, Martijn W. Heymans, Carol Jagger, Nuno Mendonça, Marga C. Ocké, et al. 2020. “Prevalence of Protein Intake below Recommended in Community-Dwelling Older Adults: A Meta-Analysis across Cohorts from the PROMISS Consortium.” Journal of Cachexia, Sarcopenia and Muscle 11 (5): 1212–22.
Bischoff-Ferrari, Heike A., Stephanie Gängler, Maud Wieczorek, Daniel W. Belsky, Joanne Ryan, Reto W. Kressig, Hannes B. Stähelin, et al. 2025. “Individual and Additive Effects of Vitamin D, Omega-3 and Exercise on DNA Methylation Clocks of Biological Aging in Older Adults from the DO-HEALTH Trial.” Nature Aging 5 (3): 376–85.
Navarro, Victor J., Ikhlas Khan, Einar Björnsson, Leonard B. Seeff, Jose Serrano, and Jay H. Hoofnagle. 2017. “Liver Injury from Herbal and Dietary Supplements.” Hepatology (Baltimore, Md.) 65 (1): 363–73.
Li, H., F. Qian, L. Han, W. Feng, D. Zheng, X. Guo, and H. Zhang. 2024. “Association of Healthy Sleep Patterns with Risk of Mortality and Life Expectancy at Age of 30 Years: A Population-Based Cohort Study.” QJM: Monthly Journal of the Association of Physicians 117 (3): 177–86.
Makarem, Nour, Cecilia Castro-Diehl, Marie-Pierre St-Onge, Susan Redline, Steven Shea, Donald Lloyd-Jones, Hongyan Ning, and Brooke Aggarwal. 2022. “Redefining Cardiovascular Health to Include Sleep: Prospective Associations with Cardiovascular Disease in the MESA Sleep Study.” Journal of the American Heart Association 11 (21): e025252.
Chaput, Jean-Philippe, Caroline Dutil, Ryan Featherstone, Robert Ross, Lora Giangregorio, Travis J. Saunders, Ian Janssen, et al. 2020. “Sleep Duration and Health in Adults: An Overview of Systematic Reviews.” Applied Physiology Nutrition and Metabolism 45 (10 (Suppl. 2)): S218–31.
Winer, Joseph R., Kacie D. Deters, Gabriel Kennedy, Meghan Jin, Andrea Goldstein-Piekarski, Kathleen L. Poston, and Elizabeth C. Mormino. 2021. “Association of Short and Long Sleep Duration with Amyloid-β Burden and Cognition in Aging.” JAMA Neurology 78 (10): 1187–96.
“Sleep Health.” 2023. December 27, 2023. https://www.cdc.gov/nchs/fastats/sleep-health.htm.
Han, Han, Ying Wang, Tongtong Li, Chengwu Feng, Catherine Kaliszewski, Yang Su, Yinfan Wu, Jian Zhou, Liang Wang, and Geng Zong. 2023. “Sleep Duration and Risks of Incident Cardiovascular Disease and Mortality among People with Type 2 Diabetes.” Diabetes Care 46 (1): 101–10.
Wang, Yafeng, Wentao Huang, Adrienne O’Neil, Yutao Lan, Dagfinn Aune, Wei Wang, Chuanhua Yu, and Xiong Chen. 2020. “Association between Sleep Duration and Mortality Risk among Adults with Type 2 Diabetes: A Prospective Cohort Study.” Diabetologia 63 (11): 2292–2304.
Jike, Maki, Osamu Itani, Norio Watanabe, Daniel J. Buysse, and Yoshitaka Kaneita. 2018. “Long Sleep Duration and Health Outcomes: A Systematic Review, Meta-Analysis and Meta-Regression.” Sleep Medicine Reviews 39 (June): 25–36.
Satyjeet, Fnu, Sidra Naz, Vinesh Kumar, Norah H. Aung, Kanwal Bansari, Sana Irfan, and Amber Rizwan. 2020. “Psychological Stress as a Risk Factor for Cardiovascular Disease: A Case-Control Study.” Cureus 12 (10): e10757.
Vaccarino, Viola, and J. Douglas Bremner. 2024. “Stress and Cardiovascular Disease: An Update.” Nature Reviews. Cardiology 21 (9): 603–16.
Ebstrup, Jeanette Frost, and Torben Jørgensen. 2012. “Stress and cardiovascular disease.” Ugeskrift for laeger 174 (4): 204–7.
Schneiderman, Neil, Gail Ironson, and Scott D. Siegel. 2005. “Stress and Health: Psychological, Behavioral, and Biological Determinants.” Annual Review of Clinical Psychology 1 (1): 607–28.
N.d. Accessed May 2, 2025. https://www.apa.org/news/press/releases/2021/03/one-year-pandemic-stress#:~:text=Nearly.
Neff, Kristin D. 2023. “Self-Compassion: Theory, Method, Research, and Intervention.” Annual Review of Psychology 74 (1): 193–218.
Dweck CS. Mindset: The New Psychology of Success. Random House Publishing Group; 2006.
Jamieson, Jeremy P., Alia J. Crum, J. Parker Goyer, Marisa E. Marotta, and Modupe Akinola. 2018. “Optimizing Stress Responses with Reappraisal and Mindset Interventions: An Integrated Model.” Anxiety, Stress, and Coping 31 (3): 245–61.
N.d. Accessed May 2, 2025. https://www.apa.org/news/press/releases/stress/2022/concerned-future-inflation.
Government of Canada, and Statistics Canada. 2023. “Perceived Life Stress, by Age Group.” Government of Canada, Statistics Canada. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009604.
N.d. Accessed May 2, 2025. https://www.apa.org/news/press/releases/stress/2023/collective-trauma-recovery.
N.d. Accessed May 2, 2025. https://nap.nationalacademies.org/catalog/25663/social-isolation-and-loneliness-in-older-adults-opportunities-for-the.
Reblin, Maija, and Bert N. Uchino. 2008. “Social and Emotional Support and Its Implication for Health.” Current Opinion in Psychiatry 21 (2): 201–5.
Holt-Lunstad, Julianne, Timothy B. Smith, and J. Bradley Layton. 2010. “Social Relationships and Mortality Risk: A Meta-Analytic Review.” PLoS Medicine 7 (7): e1000316.
“Harvard Second Generation Study.” n.d. Harvardstudy. Accessed May 2, 2025. https://www.adultdevelopmentstudy.org/.
CDC. 2025. “Health Effects of Social Isolation and Loneliness.” Social Connection. February 3, 2025. https://www.cdc.gov/social-connectedness/risk-factors/.
“Loneliness Linked to Dementia Risk in Large-Scale Analysis.” n.d. National Institute on Aging. Accessed May 2, 2025. https://www.nia.nih.gov/news/loneliness-linked-dementia-risk-large-scale-analysis.
Holt-Lunstad, Julianne. 2024. “Social Connection as a Critical Factor for Mental and Physical Health: Evidence, Trends, Challenges, and Future Implications.” World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 23 (3): 312–32.
N.d. Accessed May 2, 2025. https://www.hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf.
Goddard, Isabel. 2023. “What Does Friendship Look like in America?” Pew Research Center. October 12, 2023. https://www.pewresearch.org/short-reads/2023/10/12/what-does-friendship-look-like-in-america/.
Martino, Jessica, Jennifer Pegg, and Elizabeth Pegg Frates. 2017. “The Connection Prescription: Using the Power of Social Interactions and the Deep Desire for Connectedness to Empower Health and Wellness.” American Journal of Lifestyle Medicine 11 (6): 466–75.
Kang, Weixi. 2023. “Understanding the Associations between the Number of Close Friends and Life Satisfaction: Considering Age Differences.” Frontiers in Psychology 14 (March): 1105771.
Dunbar, Robin. 2011. “How Many ‘Friends’ Can You Really Have?” IEEE Spectrum 48 (6): 81–83.
Steptoe, Andrew, Aparna Shankar, Panayotes Demakakos, and Jane Wardle. 2013. “Social Isolation, Loneliness, and All-Cause Mortality in Older Men and Women.” Proceedings of the National Academy of Sciences of the United States of America 110 (15): 5797–5801.
Falci, Christina & McNeely, Clea. (2009). “Too Many Friends: Social Integration, Network Cohesion and Adolescent Depressive Symptoms.” Social Forces – SOC FORCES. 87. 10.1353/sof.0.0189.
Stavrova, Olga, and Dongning Ren. 2021. “Is More Always Better? Examining the Nonlinear Association of Social Contact Frequency with Physical Health and Longevity.” Social Psychological and Personality Science 12 (6): 1058–70.
Leikas, Sointu, and Ville-Juhani Ilmarinen. 2017. “Happy Now, Tired Later? Extraverted and Conscientious Behavior Are Related to Immediate Mood Gains, but to Later Fatigue.” Journal of Personality 85 (5): 603–15.
“Cigarette Smoking and Electronic Cigarette Use.” 2024. September 4, 2024. https://www.cdc.gov/nchs/fastats/smoking.htm.
N.d. Accessed May 2, 2025. https://ourworldindata.org/smoking.
“Tobacco.” n.d. Accessed May 2, 2025. https://www.who.int/news-room/fact-sheets/detail/tobacco.
US Burden of Disease Collaborators, Ali H. Mokdad, Katherine Ballestros, Michelle Echko, Scott Glenn, Helen E. Olsen, Erin Mullany, et al. 2018. “The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors among US States.” JAMA: The Journal of the American Medical Association 319 (14): 1444–72.
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. 2014. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US).
Manuello, Jordi, Joosung Min, Paul McCarthy, Fidel Alfaro-Almagro, Soojin Lee, Stephen Smith, Lloyd T. Elliott, Anderson M. Winkler, and Gwenaëlle Douaud. 2024. “The Effects of Genetic and Modifiable Risk Factors on Brain Regions Vulnerable to Ageing and Disease.” Nature Communications 15 (1): 2576.
Livingston, Gill, Jonathan Huntley, Andrew Sommerlad, David Ames, Clive Ballard, Sube Banerjee, Carol Brayne, et al. 2020. “Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission.” Lancet 396 (10248): 413–46.
“Alcohol.” n.d. Accessed May 2, 2025. https://www.who.int/news-room/fact-sheets/detail/alcohol.
GBD 2016 Alcohol Collaborators. 2018. “Alcohol Use and Burden for 195 Countries and Territories, 1990-2016: A Systematic Analysis for the Global Burden of Disease Study 2016.” Lancet 392 (10152): 1015–35.
N.d. Accessed May 2, 2025. https://www.dietaryguidelines.gov/alcohol/info.
“Surveillance Report #120.” n.d. Accessed May 2, 2025. https://www.niaaa.nih.gov/publications/surveillance-reports/surveillance120.
Livingston, Michael, and Sarah Callinan. 2015. “Underreporting in Alcohol Surveys: Whose Drinking Is Underestimated?” Journal of Studies on Alcohol and Drugs 76 (1): 158–64.
Boniface, Sadie, James Kneale, and Nicola Shelton. 2014. “Drinking Pattern Is More Strongly Associated with Under-Reporting of Alcohol Consumption than Socio-Demographic Factors: Evidence from a Mixed-Methods Study.” BMC Public Health 14 (1): 1297.
N.d. Accessed May 2, 2025. https://ourworldindata.org/alcohol-consumption.
Spencer, Merianne Rose, Sally C. Curtin, and Holly Hedegaard. 2020. “Rates of Alcohol-Induced Deaths among Adults Aged 25 and over in Urban and Rural Areas: United States, 2000-2018.” NCHS Data Brief, no. 383 (October): 1–8.
“No Level of Alcohol Consumption Is Safe for Our Health.” n.d. Accessed May 2, 2025. https://www.who.int/europe/news/item/04-01-2023-no-level-of-alcohol-consumption-is-safe-for-our-health.
Biddinger KJ, Emdin CA, Haas ME, et al. “Association of Habitual Alcohol Intake With Risk of Cardiovascular Disease.” JAMA Netw Open. 2022;5(3):e223849.
Kahane, Work by Charles. n.d. “Lives Saved by Vehicle Safety Technologies 1960 to 2012.” Accessed May 2, 2025. https://www.nhtsa.gov/sites/nhtsa.gov/files/2015sae-kindelberger-livessaved.pdf.
Green, A., G. Williams, R. Neale, V. Hart, D. Leslie, P. Parsons, G. C. Marks, et al. 1999. “Daily Sunscreen Application and Betacarotene Supplementation in Prevention of Basal-Cell and Squamous-Cell Carcinomas of the Skin: A Randomised Controlled Trial.” Lancet 354 (9180): 723–29.
Green, Adèle C., Gail M. Williams, Valerie Logan, and Geoffrey M. Strutton. 2011. “Reduced Melanoma after Regular Sunscreen Use: Randomized Trial Follow-Up.” Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology 29 (3): 257–63.
Tan, Yunfei, Lili Fang, Yichen Zhu, and Kenji Hashimoto. 2024. “Relationship between Hearing Loss and Depression: A Cross-Sectional Analysis from the National Health and Nutrition Examination Survey 2015-2018.” Journal of Psychiatric Research 178 (October): 1–7.
Bigelow, Robin T., Nicholas S. Reed, Katharine K. Brewster, Alison Huang, George Rebok, Bret R. Rutherford, and Frank R. Lin. 2020. “Association of Hearing Loss with Psychological Distress and Utilization of Mental Health Services among Adults in the United States.” JAMA Network Open 3 (7): e2010986.
Wang, Hui-Fu, Wei Zhang, Edmund T. Rolls, Alzheimer’s Disease Neuroimaging Initiative, Yuzhu Li, Linbo Wang, Ya-Hui Ma, et al. 2022. “Hearing Impairment Is Associated with Cognitive Decline, Brain Atrophy and Tau Pathology.” EBioMedicine 86 (104336): 104336.
Huang, Alison R., Kening Jiang, Frank R. Lin, Jennifer A. Deal, and Nicholas S. Reed. 2023. “Hearing Loss and Dementia Prevalence in Older Adults in the US.” JAMA: The Journal of the American Medical Association 329 (2): 171–73.
Hung, Shih-Chang, Kuan-Fu Liao, Chih-Hsin Muo, Shih-Wei Lai, Chia-Wei Chang, and Hung-Chang Hung. 2015. “Hearing Loss Is Associated with Risk of Alzheimer’s Disease: A Case-Control Study in Older People.” Journal of Epidemiology 25 (8): 517–21.
Campos, Laura, Allan Prochazka, Melinda Anderson, Alexander Kaizer, Carol Foster, and Timothy Hullar. 2023. “Consistent Hearing Aid Use Is Associated with Lower Fall Prevalence and Risk in Older Adults with Hearing Loss.” Journal of the American Geriatrics Society 71 (10): 3163–71.
Riska, Kristal M., Sarah B. Peskoe, Maragatha Kuchibhatla, Alexander Gordee, Juliessa M. Pavon, Se Eun Kim, Jessica S. West, and Sherri L. Smith. 2022. “Impact of Hearing Aid Use on Falls and Falls-Related Injury: Results from the Health and Retirement Study.” Ear and Hearing 43 (2): 487–94.
N.d. Accessed May 2, 2025. https://injuryfacts.nsc.org/motor-vehicle/occupant-protection/seat-belts/.
Fleming, Eleanor B., Duong Nguyen, Joseph Afful, Margaret D. Carroll, and Phillip D. Woods. 2018. “Prevalence of Daily Flossing among Adults by Selected Risk Factors for Periodontal Disease-United States, 2011-2014.” Journal of Periodontology 89 (8): 933–39.
Olsson, Bjørn. 2023. “Increased Bicycle Helmet Use in the Absence of Mandatory Bicycle Helmet Legislation: Prevalence and Trends from Longitudinal Observational Studies on the Use of Bicycle Helmets among Cyclists in Denmark 2004-2022.” Journal of Safety Research 87 (December): 54–63.
Bonyun, Marissa, Andi Camden, Colin Macarthur, and Andrew Howard. 2012. “Helmet Use in BIXI Cyclists in Toronto, Canada: An Observational Study.” BMJ Open 2 (3): e001049.
Shool, Sina, Seyed Mohammad Piri, Zahra Ghodsi, Reza Tabrizi, Mohammad Hosein Amirzade-Iranaq, Mahdieh Mashayekhi, Mohammad Amin Dabbagh Ohadi, et al. 2024. “The Prevalence of Helmet Use in Motorcyclists around the World: A Systematic Review and Meta-Analysis of 5,006,476 Participants.” International Journal of Injury Control and Safety Promotion 31 (3): 431–69.
Waltzman, Dana, Kelly Sarmiento, Xinjian Zhang, and Gabrielle F. Miller. 2023. “Estimated Prevalence of Helmet Use While Bicycling, Rollerblading, and Skateboarding among Middle School Students in Selected U.S. States- Youth Behavior Risk Survey, 2013-2019.” Journal of Safety Research 87 (December): 367–74.
Livingston, Gill, Jonathan Huntley, Andrew Sommerlad, David Ames, Clive Ballard, Sube Banerjee, Carol Brayne, et al. 2020. “Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission.” Lancet 396 (10248): 413–46.
Kim, Eric S., Ying Chen, Julia S. Nakamura, Carol D. Ryff, and Tyler J. VanderWeele. 2022. “Sense of Purpose in Life and Subsequent Physical, Behavioral, and Psychosocial Health: An Outcome-Wide Approach.” American Journal of Health Promotion: AJHP 36 (1): 137–47.
++++
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)
The post Infographic | The Cost of Health “Optimization” appeared first on Precision Nutrition.
Source: Health1
“I want to know I’m doing absolutely everything I can to preserve my health for as long as possible.”
We hear this kind of thing a lot.
People tell us they not only want to stay in good shape as they age, they also want to outlive their peers and age expectancies.
Imagine you could maximize your healthspan and lifespan, fend off disease, and generally remain fit, lean, and youthful into your 90’s, 100’s, and then some.
Sounds pretty compelling, doesn’t it?
There’s just one problem: Common longevity advice seems to involve an extraordinary amount of effort. And time. And money. And complexity.
Is all the effort necessary? Is it worth it?
And, will it even work?
In this article, we’ll explore:
- The biggest myths—and realities—about optimizing your health
- The real costs and tradeoffs of “optimizing” your health
- What’s actually required to improve your healthspan and lifespan
- Why enjoying your life isn’t separate from good health; it’s part of it
And, we’ll help you weigh the pros and cons so you can make informed decisions about your health, your body, and your life.
The myths—and realities—of “optimizing” your health
Health and longevity advice is everywhere these days: podcasts, books, social media, that guy at the gym…
Plus, influential “figureheads” have given the movement outsized attention. Think: popular podcasters and health experts Dr. Peter Attia, Dr. Andrew Huberman, and Dr. Rhonda Patrick, and biohacker Bryan Johnson.
We understand the appeal of this kind of content. Who doesn’t want a longer, healthier life? (Not to mention the comforting sense of control that can come from designing and executing a “perfect” health plan.)
But for us at PN, where we’ve collectively coached hundreds of thousands of people with real human lives, we know that “optimal” is rarely realistic.
Not only that, optimal isn’t necessary.
Making modest, relatively consistent efforts towards health and well-being will likely give you better results than following an intense, highly “optimized” protocol.
If that sounds hard to believe, we get it. So let’s explore that bold statement, starting with the biggest myths surrounding longevity and health optimization.
Myth: The “basics” aren’t enough.
There’s an idea that getting and staying healthy must require a set of complex, “cutting edge” strategies—especially if your goal is to outlive the average American.
In reality, the “basics” work really, really well. (These are things like exercising regularly; eating a nutrient-rich diet; getting adequate sleep; managing stress; and staying socially connected. We’ll discuss these more later.)
Only, very few people do the basics consistently.
The real reason more people aren’t living as long, or as well, as they could be isn’t because they’re not taking ice baths or getting vitamin C infusions…
It’s because they’re not doing the (relatively) simple stuff, consistently.
If you’re really, truly doing a well-rounded set of health-promoting behaviors with 80-90 percent consistency, you’re probably already close to peak optimization.
Myth: More is better
If a handful of basic behaviors get results, then doing them perfectly and as much as possible will help you get, and stay, even healthier—right?
Not so fast. There’s a law of diminishing returns when it comes to health and fitness efforts.

Plus, in our experience, doing too many things or adding in too much complexity to your health and fitness regime can:
- Add risk factors that could actually make your health and fitness worse (such as chronic injuries or burnout due to overtraining, and/or nutrient deficiencies or disordered eating due to an over-preoccupation with “clean” or restrictive eating).
- Make it harder for you to sustain good habits. People who take on too much are more likely to burn out. Research shows people who try to accomplish multiple goals are less committed and less likely to succeed than those focused on a single goal.1
- Make your life less enjoyable, which in turn compromises health. Striving to maximize physical health can interfere with mental, emotional, and social well-being, which plays an essential role in healthspan and lifespan. (One study showed people with high levels of happiness and life satisfaction lived up to 10 years longer than people with low levels.2)
And what’s the point of living longer if you’re not living a full, well-rounded, enjoyable life? While some effort is definitely important, past a certain point, more isn’t necessarily better.
Myth: Cutting-edge strategies offer significant benefits.
Let’s say you could put all those advanced, complex strategies into action without sacrificing consistency or life enjoyment, or compromising your overall well-being.
They’d have to pay off, wouldn’t they?
Not necessarily.
Much of the research on longevity optimization (so far) is either in mice, is observational, is theoretical, or has been tested on very small numbers of people for very short periods of time.
In fact, many of the fringe methods and supplements touted by influencers or biohackers are not only unproven but even potentially unsafe.3 4 5 6
Point being: Put your efforts towards foundational health behaviors with proven track records (the kind we’ll cover in this article) before you invest in fringe efforts.
Myth: It’s all or nothing.
You might think, “Well, I’m not getting out of bed at 5 a.m. five times a week to go running for 60 to 90 minutes to optimize my VO₂ max, so I may as well just accept I’m not going to be a healthy person.”
Some folks feel overwhelmed by the idea of optimizing their health, so they figure they might as well do nothing.
However, our internal data shows that you can be far from “perfect” to get results.
In our year long PN Coaching program, even clients who practiced their (basic) habits less than half of the time got measurable results.

(Read more: Nearly 1 million data points show what it REALLY takes to lose fat, get healthy, and change your body)
Don’t let optimization culture convince you great health is beyond your capabilities.
Instead, we encourage you to…
- Consider your options. Review the facts, and get a clear understanding of which behaviors are most likely to give you the best bang for your buck.
- Get clear on the tradeoffs. Decide which things you are, and aren’t willing to commit to.
- Make decisions that align with your goals. Including what kind of lifestyle you want, and how you want to spend your time and dollars.
Keep reading and we’ll guide you through it.
The benefits—and tradeoffs—of a healthy lifestyle
Putting effort towards your health is great. But efforts come with tradeoffs.
Here’s a look at both the efforts, and the tradeoffs, to achieve the health you want for yourself.

A deeper look: The most effective health behaviors (and their optimal dose)
If you want to reduce your risk of chronic disease, and generally stay healthier for longer, what should you do?
As we said earlier, the issue isn’t that we need some highly detailed, cutting-edge protocol. The basics work. The issue is that most people don’t do them.
For example, as shown in the image below, most people don’t get enough fruits and veggies, sleep, or exercise. And the number of people who do all these things on a regular basis (while also avoiding tobacco and minimizing alcohol) is extremely low: likely a fraction of a percent.

Finally, let’s take a closer look at what these basics are, and the “sweet spot” of effort versus reward.
Foundational Health Behavior #1: Exercise regularly
All health experts agree: Moving your body is important.
Yes, exercise will help you stay lean, and improve mood, energy, and function, but it will also help you stay alive (and healthier) for longer.
In fact, a study of Harvard alumni found that any amount of physical activity reduces the risk of death from any cause. Exercise extended lifespan regardless of body weight, blood pressure, smoking habits, or genetic predisposition.7
Another study of 272,550 older adults found engaging in even low amounts of physical activity significantly decreased risk of death from cancer, cardiovascular disease, and all causes.8
Specifically, steep risk declines happened when accumulating at least 7.5 MET-hours* of activity per week. The greatest increase in benefits came from achieving 7.5 to 15 MET hours. Increasing activity beyond that further decreases risk, but at a continually lower rate, as the graph below shows.

*MET-hours (Metabolic Equivalent Hours) measures the energy cost of activity, based on duration and intensity. Some examples: 2 hours of resting = ~2 MET-hours; 2 hours of moderate-intensity aerobic activity = ~8 MET-hours; 2 hours of moderate resistance training = ~7 MET-hours.
Increasing the intensity of exercise is an efficient way to rack up MET-hours, but plain old walking counts too: In a study of 28,000 adults, every 1,000 daily step increase was associated with a 12 percent lower risk of death. (This association began at 2,500 steps and continued up to 17,000 steps.)9
(Cool factoid: For folks concerned with dementia in particular, one study showed that getting just 3,826 steps per day was associated with a 25 percent reduced risk of dementia—and getting 9,826 steps per day was associated with a 50 percent lower risk!10)
Ideally, cardiovascular activity is paired with resistance or weight-bearing exercise.
Resistance training supports health and longevity in various ways: it can help preserve valuable muscle mass, maintain mental sharpness, improve odds of surviving cancer, support metabolic health, and generally help you stay alive.11
Among older adults especially, falls are a leading cause of death.12 Resistance training can both prevent the risk of falls–because of improved balance and muscle stability13—as well as reduce the risk of serious injury–because of better bone density.14
A sedentary lifestyle does the opposite, increasing risk of cardiovascular disease, diabetes, hypertension, cancer (breast, colon, colorectal, endometrial, and epithelial ovarian cancer), and all-cause mortality.15
In fact, two decades of sedentary lifestyle is associated with twice the risk of premature death compared to being physically active.16
 How much exercise should you do?
How much exercise should you do?
Standard exercise recommendations suggest:17
- 150 minutes per week of moderate-intensity aerobic activity, or 75 minutes per week of vigorous aerobic activity (or some combination of both), plus
- 2 sessions per week of resistance training, targeting most major muscle groups
Getting up to 300 minutes per week of moderate-intensity or 150 minutes of vigorous-intensity aerobic activity (or some mix of both) as well as three resistance training sessions per week provides further benefits.
 Are people getting enough exercise?
Are people getting enough exercise?
Most people are not.
Only 24 percent meet the recommendations for both aerobic and resistance exercise. And fewer than 47 percent of American adults meet recommendations for aerobic physical activity.17
 Is getting more than the recommended amount better?
Is getting more than the recommended amount better?
For the most part yes, but past a certain point, more effort delivers less benefit—and potentially more risk.
Overtraining (and/or under-recovering) can disrupt hormone levels, mess with sleep and mood, cause excess fatigue, chronically elevate your heart rate, cause injuries, and more.18 19 Extreme volumes of endurance exercise training may be detrimental for the heart, and increase risk of myocardial fibrosis, coronary artery calcification, and atrial fibrillation.20 21 22 23
So, the benefits of exercise exist on a U-shaped curve. (This is known as the “Extreme Exercise Hypothesis,”24 as seen in the image below.)

A “high” amount of exercise is good for you, but the “highest” amount possible probably isn’t. (Health benefits likely max out around 7-10 hours of cardio, and 3-4 resistance training sessions per week.)
We like what one study concluded: “If the mantra ‘exercise is medicine’ is embraced, underdosing and overdosing are possible.”25
Foundational Health Behavior #2: Eat a nourishing, nutrient-rich diet
Eating well doesn’t have to be complicated. There are a few key elements to nail down, and the rest is up to your own personal preferences and needs.
We suggest focusing on three nutrition fundamentals.
Nutritional key #1: Eat more whole and minimally-processed foods
Whole and minimally-processed foods are naturally nutrient rich—complete with fiber, healthy fats, vitamins, minerals, and phytochemicals—and far less calorie-dense than highly- or ultra-processed foods (UPFs). They also have less sugar, sodium, and trans fats—the latter which is directly linked to an increased risk of cardiovascular disease, breast cancer, complications during pregnancy, colon cancer, diabetes, obesity, and allergy.26 27 28
These qualities contribute to their many health benefits; Diets rich in whole or minimally-processed foods are associated with lower rates of depression,29 30 31 heart disease,32 type 2 diabetes,33 cancer,34 and improved longevity.35
The largest study on processed foods—which included almost 10 million participants—found UPFs are linked to 32 harmful effects, including type 2 diabetes, mental health disorders, obesity, cardiovascular disease, and all-cause mortality.36
Another study found that a higher consumption of ultra-processed foods (four or more servings daily) was associated with a 62 percent increased risk of all-cause mortality. (For each additional serving of ultra-processed food, all-cause mortality increased by 18 percent.)37
Not that you need to be plucking tomatoes straight off the vine.
Eating a minimally processed food diet is more about overall dietary patterns—and moving along the continuum of improvement—rather than rigidly avoiding all forms of processing.

 How many minimally-processed foods should you eat?
How many minimally-processed foods should you eat?
There currently aren’t any formal guidelines for the amount of minimally-processed foods to eat. In our experience coaching over 100,000 clients, we find people are most satisfied, and get significant health improvements, when 70 to 80 percent of their diet comes from whole or minimally-processed foods.
Any improvement counts though. If you’re currently eating very few whole and minimally processed foods, getting at least 50 percent of your diet from these foods would make a big difference to your health, energy, and longevity.
 Are people eating enough minimally-processed foods?
Are people eating enough minimally-processed foods?
No.
Recent US data shows that Americans get about 28.5 percent of their calories from whole or minimally-processed foods, and 56 percent of their calories from highly- or ultra-processed foods.38
 Is getting more than the recommended amount better?
Is getting more than the recommended amount better?
Not beyond a certain point.
If you want to, consuming up to 90 percent of calories from minimally-processed foods will truly maximize your benefits, but beyond that there are likely no further benefits.
Besides, some processed foods enhance health rather than detract from it. Think about the protein powder that helps you meet your protein requirements, the commercial salad dressing that helps you eat your vegetables, or the weekly brownie à la mode you share with your grandkid that brings joy to both of your lives.
(Read more: What you should know about minimally-processed foods vs. highly-processed foods)
Nutritional key #2: Eat five fruits and vegetables
You’ve heard it a million times. We’ll be the nag and say it again: Eat your fruits and veggies.
A massive study involving over 1.8 million people showed that eating more fruits and vegetables was significantly associated with a decreased risk of death—with the benefits plateauing at five servings a day. People who ate five servings a day had a 13 percent lower risk of death from any cause compared to people who ate two servings per day.39
Additionally, the consumption of fruits and vegetables very likely reduces the risk of hypertension, coronary heart disease, and stroke; probably reduces the risk of cancer; and possibly prevents weight gain.40
 How many fruits and vegetables should you eat?
How many fruits and vegetables should you eat?
A healthy target is five fist-sized servings of fruits and vegetables daily. (Generally, we recommend dividing that into three servings of veggies and two servings of fruit.)
For bonus points, try to eat a variety of colors.
The pigments in fruits and veggies come from various healthful nutrients (called phytochemicals or phytonutrients). Different colors mean different phytochemicals, giving you a diverse array of these beneficial compounds, which are likely responsible for a majority of the health benefits of fruits and vegetables.
(Read more: What the colors of fruits and vegetables mean)
 Are people eating enough fruits and vegetables?
Are people eating enough fruits and vegetables?
No.
Americans only eat an average of 2.5 servings of produce (fruit and vegetables combined) per day.41
Only 12.2 percent of people meet fruit intake recommendations, and less—9.3 percent—meet vegetable intake recommendations.
A mere ten percent of Americans get a full five servings of fruits and vegetables combined per day.42
 Is getting more than the recommended amount better?
Is getting more than the recommended amount better?
There are likely diminishing returns to eating more than the above suggestions.
In that massive study mentioned earlier that observed 1.8 million people, the life-extending benefits of fruits and veggies plateaued at five servings per day.39
In other words, higher intake (beyond two servings of fruit and three servings of vegetables) was not associated with additional disease risk reduction.
That said, there may be other benefits to eating more fruits and vegetables. For example, due to their fiber and water content, fruits and vegetables are filling yet low in calories, so they can support weight management—and they certainly aren’t going to harm your health.
Nutritional key #3: Eat enough protein
Protein is the most important macronutrient to get right, especially as we age.
Plant protein in particular is linked to a reduced risk of cardiovascular disease and death from all causes.43 44 45
In terms of animal proteins, the results are more mixed. (That said, research on protein intake and mortality is generally based on observational studies that don’t give us clear ideas about cause and effect.) Generally, minimally processed forms of fish, poultry, and low-fat dairy are the best animal protein sources.
To minimize health risks such as diabetes, cardiovascular disease, and cancer, limit processed forms of red meat (like bacon, hot dogs, deli slices, and pepperoni sticks). Even unprocessed forms of red meat should likely be limited to about 18 oz (~4 to 5 palm-sized portions) or less per week.46 47 48
Nonetheless, regardless of the source, getting sufficient protein—at least 1.2 g of protein per kg of body weight—significantly reduces the risk for sarcopenia (muscle loss), frailty, and neuromuscular decline.49 50
Protein is also vital for maintaining and building muscle, keeping bones and soft tissues healthy, supporting immunity, and more. It’s also the most satiating macronutrient, and thus helpful for fat loss and/or body recompositioning.
 How much protein should you eat?
How much protein should you eat?
The current USDA recommendation for protein intake is at least 0.8 grams of protein per kg of body weight (0.35 g/lb). However, newer research suggests this is likely the absolute minimum amount, and only for relatively young sedentary individuals.
A better minimum intake for most is likely 1.2 g/kg (0.55 g/lb, or about 3 to 5 palm-sized portions of protein-rich foods), especially for older adults, as they’re at greater risk of muscle loss.
Protein intake for muscle growth and retention, and/or if performing resistance training or other vigorous exercise would be 1.6 to 2.2 g/kg (0.75-1 g/lb), or about 4 to 8 palm-sized portions of protein-rich foods.
 Are people eating enough protein?
Are people eating enough protein?
That depends on how “enough” is defined.
Most adults eat at least 0.8 g/kg. However, up to 10 percent of young women and up to 46 percent of older adults don’t hit this mark.51 And, as noted, that recommendation is probably conservative compared to the ideal intake.
Protein is also especially critical for those on GLP-1 medications (Ozempic, Wegovy, Zepbound) to help prevent the muscle loss they can lead to. Aiming for at least 1.2 g/kg is vital for this population, especially if they are also older. (Getting closer to 1.6 g/kg is even better, if possible.)
 Is getting more than the recommended amount better?
Is getting more than the recommended amount better?
Once you get up to 1.2 g/kg, not necessarily. That amount is likely adequate for most, especially sedentary folks.
If you’re trying to build muscle and strength or recover from vigorous exercise, or are taking GLP-1 medication for fat loss, striving towards 1.6 g/kg would help you achieve that goal more easily.
If you’re trying to maximize strength and muscle gains, and/or are doing lots of strenuous exercise, consuming 1.6-2.2 g/kg is optimal (with the highest end of that range maxing out all benefits).
What about supplements?
Supplements make up a large part of the discussion around aging, but in reality only play a small role when it comes to increasing health and longevity.
Using supplements (like a multivitamin, or doctor recommended vitamin D or iron) to prevent or correct deficiencies can be helpful for overall health well-being.
Then, there are other supplements that have reasonably strong track records and can help us meet nutritional needs (protein powder), improve performance (creatine), or potentially even slow aging (fish oil might slow biological aging by a small amount).52
However, the buzziest, trendiest supplements are often less proven.
For example, curcumin, spirulina, and ginger are often listed as supplements that might help with inflammation, a hallmark of aging. However, the research here is still early, and far from definitive.
There are also even less substantiated supplements that might modify other aspects of aging (resveratrol, NAD+, NAC), but the evidence is either very minimal or only in animal models.
Some supplements (especially herbal supplements) can even cause harm, like liver damage.53
If you want to give supplements a try, check for high-quality third-party seals of approval from organizations such as NSF.
Examine.com—an online database that provides independent research summaries and analyses on most popular supplements—is also an excellent resource to help you determine which supplements might actually be effective.
Regardless, talk to your healthcare provider before taking supplements, particularly if you take other medication.
Foundational Health Behavior #3: Get adequate sleep
Research shows that men who get enough quality sleep live almost five years longer than men who don’t, and women who get enough live two and a half years longer.54
Studies also show sleep is just as important for your heart health as exercise, whole foods, weight management, cholesterol, blood pressure, and blood sugar control.55
Compared to 7 hours of sleep per day, a 1 hour decrease in sleep duration has been associated with an 11 percent increased risk of cardiovascular disease and a 9 percent increased risk of type 2 diabetes.56
Older adults who sleep less than 6 hours per night are at higher risk for dementia and cognitive decline than those who sleep 7 to 8 hours.57 (Deep sleep helps clear beta-amyloid plaques and wash out toxins from our brain, thought to be partially responsible for dementia.)
 How much sleep should you get?
How much sleep should you get?
Sleep experts agree that 7 to 9 hours a night on average—with at least 7 hours of sleep most nights of the week—is ideal for most.
However, the exact ideal hours may vary person to person.
Generally, the right amount of sleep for you is the amount that allows you to feel relatively refreshed shortly after waking up, and allows you to fall asleep relatively easily at bedtime, with relatively sustained energy throughout the day.
 Are people getting enough sleep?
Are people getting enough sleep?
About a third of US adults don’t meet the recommended amount of 7 to 9 hours of sleep per night.58
 Is getting more than the recommended amount better?
Is getting more than the recommended amount better?
Not necessarily.
It seems that 7 to 9 hours of sleep a night is ideal in terms of health outcomes.56
Interestingly, longer sleep duration (over 9 hours per night on average) is associated with an increased risk of cardiovascular disease, type 2 diabetes, and overall mortality.59 60 61
However, it’s not clear that these risks are caused by sleeping more. Just as likely, it may be other health problems (such as depression, sleep apnea, or heavy alcohol consumption) that lead to both longer sleep times and higher health risks.
(Read more: Transform your sleep—The scientific way to energize your body, sharpen your mind, and stop hitting snooze)
Foundational Health Behavior #4: Manage stress
When left unchecked for long periods of time (say, months or years without periods of recovery), stress can have negative effects on nearly every aspect of our health, as the below image shows.

Chronic stress—which tends to increase heart rate, blood pressure, and inflammation—increases the risk of cardiovascular disease.62 63 64 Additionally, long-term stress tends to worsen mental and emotional health, increasing the risk of anxiety and depression.65 It can also make people more likely to turn to substances like alcohol as an attempt to cope.66
That said… Not all stress is bad.
In fact, stress is a normal, natural, and even beneficial part of life; the right amount helps us feel motivated, purposeful, and engaged with life.
So, rather than avoiding or demonizing stress, it’s helpful to work with it, using it as an opportunity to develop healthy coping mechanisms, appropriate recovery strategies, and overall resilience.
And this doesn’t necessarily mean sitting on a cushion and meditating.
Stress management can include simple mindset shifts: Practicing self-compassion,67 having a growth mindset,68 and framing stress as a normal and even beneficial part of life69 have all been associated with better coping under stress.
Basic self-regulation skills also help. This involves noticing and naming what you’re feeling, having good control over your actions, and using a broad range of coping skills to help yourself process emotions and recover from stress. With these skills, you build self-awareness and the ability to handle challenges better, because you know how to calm yourself down after an activating event—regardless of how it went.
The below image offers a spectrum of more—small and big—ways to regulate stress.

 How much stress management should you engage in?
How much stress management should you engage in?
Think of stress management and recovery as a thing you do in proportion to the stress and demands of your life.
We often use the analogy of a jug: When stress drains your tank, stress management and recovery practices help fill it back up again.

And, as with all of the foundational health habits we’ve discussed, every little bit counts.
Whether you’re experiencing a little or a lot of stress in your life, even three to five minutes of purposeful recovery—doing deep breathing exercises, some journaling or gentle stretching, or just stepping outside to get some fresh air and listen to the birds—can help fill your tank.
 Are people doing enough to manage stress?
Are people doing enough to manage stress?
Probably not.
In the US, over a quarter of people report that most days, they’re so stressed they can’t function.70 In Canada, it’s similar: Just under a quarter of people say that most days in their life are either “quite a bit” or “extremely” stressful.71
Additionally, over a third of people say they don’t know where to start when it comes to managing their stress.72
 Is getting more than the recommended amount better?
Is getting more than the recommended amount better?
Not necessarily.
The goal is to find your stress “sweet spot.” Because we all enjoy and tolerate different types and amounts of stress, how you feel is actually a pretty good indicator of whether stress is too low, too high, or “just right.”
As the image below shows, if you generally feel bored and purposeless, stress is likely too low; if you feel energized and engaged, stress is probably close to your “sweet spot”; and if you feel panicky or so overwhelmed you’ve started to feel hopeless, stress is likely too high.

While having a routine for stress management is a smart idea, there’s likely a point of diminishing returns here too. If you’re in that stress “sweet spot” (energized/engaged, not bored and not overwhelmed), then adding more stress reduction techniques might not help further—and may actually add stress by giving you yet another task to do.
Foundational Health Behavior #5: Stay socially connected
You might not think of social connection as a health imperative, but it is.
Not only is the social and emotional support associated with improved well-being, it’s also associated with reduced risk of premature death.73 74 When relationships are strong, people have a 50 percent increased likelihood of survival during any given time.75
In fact, one of the longest running studies—the Study of Adult Development out of Harvard Medical School, which has been tracking participants for over 87 years (and counting)—found that strong relationships were the biggest predictor of not only life satisfaction but longevity. (Relationships were more predictive of these outcomes than social class, wealth, IQ, or genetics.)76
No surprise, not having a social circle comes with its own distinct risks.
Social isolation and loneliness can increase a person’s risk for heart disease and stroke, type 2 diabetes, depression and anxiety, suicidality and self-harm, dementia, and earlier death.77 78
A frequently cited statistic highlights its profound impact:
The effect of social isolation on mortality is comparable to smoking up to 15 cigarettes per day79—surpassing even the risks associated with obesity and physical inactivity.80
 Are people getting enough social connection?
Are people getting enough social connection?
It seems many of us could use more friends.
About 1 in 3 adults report feeling lonely, and 1 in 4 report not having social and emotional support.77
Eight percent of adults say they have no close friends, 53 percent say they have between one and four close friends, and 38 percent report having five or more friends.81
 How much social connection should you aim for?
How much social connection should you aim for?
Generally speaking, research finds that people who have three to five close friends they regularly interact with (one to three times per week, in-person or via phone call) get the most social benefit.82 83 84 85
On average, interaction with a smaller group of people tends to provide more benefit than a large network of acquaintances.86
That said, individual needs vary. If you feel authentically connected to others, have a strong sense of belonging, and generally feel socially fulfilled, that’s what matters most.
 Is getting more than the recommended amount better?
Is getting more than the recommended amount better?
Likely not. Some evidence suggests that excessive social engagement (daily or multiple times daily) actually might increase mortality risk.87 That’s probably because over-socializing can increase mental, emotional, and physical fatigue,88 and often this level of socialization includes alcohol or other potentially risky behaviors.
Additionally, it can take away time and energy that could be put towards other life-building and health-promoting behaviors (like work, exercise, or sleep).
The takeaway? Strive for socializing that brings value to your life. No need to add so much that you wind up exhausted, or unable to keep up with other priorities.
Foundational Health Behavior #6: Minimize known harms
Minimizing activities we know to be harmful is a key part of looking after your long-term health, yet it can be easy to overlook these things. (Maybe because we’d rather keep doing them.)
Two of the biggest culprits are smoking and drinking alcohol.
Harm Avoidance Key #1: Don’t Smoke
We all know smoking is bad for us. But smoking is still relatively common:
- In the US, 10.9 percent of adults smoke cigarettes, and 6.6 percent smoke e-cigarettes.89
- Globally, the trend is even higher: 22.3 percent of the world’s population use tobacco (36.7 percent of men and 7.8 percent of women).90
The WHO estimates more than 8 million people die prematurely yearly from tobacco use (with an additional 56,000 people dying annually from chewing tobacco).91 This makes tobacco a leading (i.e. top 3) risk factor for premature death and all-cause mortality.92
Smoking is also a risk factor for several chronic conditions, including coronary heart disease, stroke, emphysema, and cancer.93 (Globally, about a quarter of cancer deaths are attributed to smoking.90)
Harm avoidance key #2: Limit alcohol
At this point, the research is pretty clear: Alcohol has negative implications for your health, especially past a certain point of regular use.

Alcohol plays a causal role in 200+ diseases, particularly liver diseases, heart diseases, at least seven types of cancers, depression, anxiety, alcohol use disorders, and dementia.94 95
In 2019, 2.6 million deaths worldwide were attributable to alcohol consumption.96 For people in the 15-49 age range, alcohol is the leading risk factor for death, with 3.8 percent of female deaths and 12.2 percent of male deaths attributable to alcohol use.97
 How much alcohol is “safe” to drink?
How much alcohol is “safe” to drink?
US guidance on alcohol suggests keeping intake at moderate levels, or less.98
A moderate intake means:
- Two drinks or less per day for men (14 or less per week), with no more than 4 at a single sitting
- One drink or less per day for women (7 or less per week), with no more than 3 at a single sitting
Importantly, a drink is defined as containing 14 grams (about 0.6 fluid ounces) of pure ethanol, which equates to:
- 12 ounces of regular beer (5% alcohol by volume)
- 5 ounces of table wine (12% alcohol by volume)
- 1.5 ounces of 80-proof distilled spirits (40% alcohol by volume)
 Are people limiting their alcohol enough?
Are people limiting their alcohol enough?
In the US, people tend to drink more than the recommended guidelines.
In 2021, the National Institute on Alcohol Abuse and Alcoholism reported that the average American aged 21 or older consumed 2.51 gallons of pure alcohol over the course of a year—equivalent to about 10 standard drinks/week.99 However, research suggests surveys typically underestimate consumption by 40 to 50 percent.100 Further, other research shows that the heavier a person drinks, the more significantly they’re likely to underestimate and/or underreport their drinking.101
All that to say, the average American is likely having more (or even far more) than 10 drinks per week.
Add to that:
- In 2016, 36.4 percent of Americans (age 15+) said they had at least one episode of binge drinking (6+ drinks in one session) in the last month102
- About 7 percent of the world’s population aged 15+ years have an alcohol use disorder96
- Alcohol-related deaths have been rising: in the last five years, alcohol-induced deaths have increased by 26 percent103
 Is more abstinence from alcohol better?
Is more abstinence from alcohol better?
In 2023, the WHO released a statement saying no amount of alcohol is “safe.”104 This interpretation is still debated, and data continues to emerge.
Here’s our take: An abstinence-only policy is likely a failed policy for many. Rather, we want people to be informed so they can make intentional decisions.
To be clear, alcohol is not beneficial for physical health; it’s a known human carcinogen. However, while alcohol does increase health risks, risk does not rise in a linear fashion with intake. Meaning, small doses are unlikely to have a significant impact on your health. But when you drink more heavily, the risks rise exponentially.105
Drinking heavily can mean either:
- Having more than 7 drinks in a week for a woman, or more than 14 drinks in a week for a man, or
- Having 4 or more drinks in one sitting for a woman, or 5 or more drinks in one sitting for a man (binge drinking).
(Reminder: A single drink refers to those definitions mentioned previously. Pints of beer, and heavily poured wine glasses and cocktails are more than single servings… Just because it fits in a single glass doesn’t mean it counts as “one” drink.)
Ultimately, it’s about finding the level of risk you’re willing to tolerate relative to whatever benefits you feel alcohol provides you.
Our general recommendations:
- If you’re otherwise healthy and have no other alcohol-related risk factors, limit drinking to moderate levels or less
- If you’re otherwise healthy but have one or two alcohol-related risk factors (such as breast cancer history), limit drinking to light levels (1 to 3 or 4 drinks per week) with occasional moderate intakes on special occasions, or less
- If you have several alcohol-related risk factors (such as breast cancer history, family history of alcoholism, or contraindicated medications) abstain from alcohol entirely
Foundational Health Behavior #7: Do Basic Preventive Health Measures
In all the chatter about longevity optimization, it can be easy to forget about all the boring—but no less important—things that help you stay safe and healthy throughout your life.
These include things like:
- Getting regular check-ups, or seeing your doctor or healthcare provider if questions or concerns arise
- Getting recommended bloodwork, screenings, and vaccines
- Getting and keeping blood cholesterol, sugar, and pressure in recommended ranges as early as possible
- Regularly seeing your dentist, and regularly brushing and flossing
- Practicing safer sex
- Seeing medical specialists as recommended or appropriate (OBGYN, optometrist, ENT, dermatologist, etc.)
- Wearing seatbelts (Buckling up in the front seat reduces risk of fatal injury by 45 percent!106)
- Wearing a helmet when cycling, skateboarding, or motorbiking
- Regularly wearing sunscreen (Used appropriately, sunscreen decreases risk of skin cancers by 40 to 50 percent107 108)
- Protecting your hearing (Untreated hearing loss increases risks for depression, social isolation,109 110 cognitive decline,111 dementia,112 113 and falls114 115)
… And generally using common sense. (As in, avoid the “hold my beer” type stuff.)
Basic health maintenance and risk avoidance practices matter—a lot.
Notably, we can’t control every element of our environment. Some factors influencing our health are more structural and systemic, woven into the fabric of our societies.
These are called social determinants of health, and include poverty, racism, homophobia, lack of accommodation for disabilities, and displacement (as in the case of refugees). For some folks, doing the above protective behaviors—like visiting the family doctor, getting glasses, going to the dentist, or even walking safely down the street—will be harder, sometimes near impossible.
This isn’t meant to be a throwaway line that diminishes the difficult reality for so many people, but rather a gritty, realistic mantra: Do the best you can with what you’ve got.
 How much preventative health care do you need to do?
How much preventative health care do you need to do?
Generally speaking, aim to be consistent with the habits you know you “should” do.
You know the drill: Brush and floss daily; wear your helmet every time you ride a bike; wear your seatbelt every time you drive; put on sunscreen when you go out into the midday sun; don’t regularly blast your music at full volume; and so on.
And if you have lingering things on your “I should really do that” list (like getting that weird mole checked out, or that bloodwork done), go do it.
 Are people practicing enough basic preventative health measures?
Are people practicing enough basic preventative health measures?
We’ve offered a long-ish list of basic health practices that can protect health, so we won’t go into each in-depth.
That said, when looking at the above list, it’s probably fair to say most people will notice a few behaviors they might practice more consistently.
For example, while most of us are really consistent with our seat belts (usage is close to 92 percent!116), many of us could break out the floss more often (only 32 percent of Americans floss daily117).
And, research shows that only about half of cyclists and motorcyclists wear helmets when riding118 119 120 (and use is even lower among skateboarders and rollerbladers121).
Hearing loss is the number one modifiable risk factor for dementia,122 so make sure you also follow the “60/60 rule” if you like to pump up the tunes on your headphones: Listen at 60 percent of your device’s maximum volume for 60 minutes, then take a break. (And wear earplugs when you mow the lawn!)
 Are more preventative measures better?
Are more preventative measures better?
Once again, there’s likely a law of diminishing returns when it comes to preventative health measures, just like everything else.
The point isn’t to become obsessed with eliminating all possible risks at every turn.
Rather, it’s that reasonable efforts towards protecting your health do count, and they‘re immeasurably more important for overall health than the latest optimization fads.
Bonus Foundational Health Behavior: Foster a sense of purpose and meaning
Research consistently shows that having a strong sense of purpose and meaning for our life improves our health, overall well-being, and longevity too.123
A sense of purpose seems to help people live longer, even when controlling for other markers of psychological well-being.
There’s something uniquely beneficial about having a strong purpose that’s different from, say, being happy.
Having a strong sense of purpose can mean many things, but it generally indicates that you have goals, and an aim in life.
This purpose can be many things:
- Helping others
- Being connected to family and/or close friends
- Being a key part of a community
- Enjoying a hobby
- Learning new skills
Having purpose may help with longevity for a few reasons:
It makes you more likely to engage in health-promoting behaviors, such as getting enough sleep and eating more fruits and vegetables.123
It also tends to improve mental health. For example, one study showed that people with the strongest sense of purpose had a 43 percent reduced risk of depression.123
Finally, it may simply help people live longer because it makes you want to live longer. When people have a sense of purpose, they often want to live longer, healthier lives, so they can fulfill that purpose to its fullest. And while wanting to live won’t make it so, it certainly doesn’t hurt.
Still thinking about optimizing? Consider these additional tradeoffs
We hope it’s clear by now: You can take yourself really far with some solid basics (that will themselves take some decent time and effort!).
But, if you want to go even further, your effort might have to increase exponentially, just as those gains become less certain, and more marginal.
Here’s what to keep in mind.
First, it takes a lot of time (and money) to optimize.
Let’s compare the time and financial investment of two imaginary people.
The first person is what you might call a “healthy” or “medium effort” person. They’re someone who is pretty consistently meeting all of the above recommendations.
The second person is what you might call an “optimizer.” They do all the above recommendations, but to the max, and many of the fringe recommendations often discussed on health-related podcasts and books.
How much time and money might each of these people invest in their health efforts on a weekly basis? Here’s what that might look like.

On top of that, there are “optimizing” behaviors and assessments that might be performed less often—say, monthly, seasonally, annually, or even every few years. Of course, these practices will still require time and money, so even though they’re less frequent, they still have to be accounted for.
Here are some examples of those kinds of products, therapies, and tests:
- Dietary supplements (vitamin, mineral, and/or herbal supplements; “superfoods”; fish oil; probiotics, resveratrol, NAD+, NAC, curcumin, & more)
- Bloodwork testing (for advanced lipid testing, inflammatory markers, hormone levels, and nutrient status)
- IV therapy (for hydration, vitamins, glutathione, or NAD+)
- Infrared sauna sessions
- Plasma transfusions
- Gene therapy
- Stem cell therapy
- Medical tourism and therapeutics retreats
- Full-body MRIs
- Genetic testing
- Concierge medical services
- And more…
Though it’s hard to estimate the cost of these items, opting to do just a handful could easily cost an extra $10,000+ per year.
Overall, we’d estimate it takes at least three to four times the time, effort, and money to follow an “optimizer” type lifestyle, compared to a plain old “healthy” lifestyle.
As we’ve seen above, this 3-4x effort will likely translate to some extra benefits, but the medium-effort “healthy” lifestyle will likely get most people at least 80 percent of the results they’re after (such as improved lifespan, healthspan, and quality of life).
Besides, optimizing too much can negatively impact your well-being and quality of life.
The harder and more extreme someone’s fitness or health regime, the harder they typically fall off the wagon. So, taking on too much can actually put you more at risk of quitting the foundational health behaviors we mentioned earlier.
Even if you stick with it, over-focusing on health and longevity will almost certainly interfere with your ability to enjoy a full, well-rounded, meaningful life.
For example, if you get too focused on physical health, you may find other aspects of your deep health and overall wellbeing suffer, such as your relational, existential, mental, and emotional health.

Take this a step further, and “optimizing” can tip over into obsession. Sometimes, under the surface of “I just really care about my health” is disordered eating, orthorexia, or another mental health condition.

This, to us, is the heart of things: It’s important to not only stay relatively healthy, but also to enjoy your life while you’re living it.
In fact, enjoying your life isn’t separate from good health. It’s part of it.
What to do next
1. Clarify your goals.
Take a step back and consider what you really want most for yourself.
What kind of life do you want to have?
How important is it to maximize your healthspan and lifespan, and how does that line up with your other priorities?
2. Consider the tradeoffs.
Given what you want most for yourself, and the resources you have available, what’s realistic for you?
How much time, money, and effort are you willing to put in to achieve health and lifespan goals?
What are you prepared to give up? What aren’t you prepared to give up?
3. When looking to make improvements, start with the basics first.
Review the foundational health behaviors in this article. How many of them are you already doing? Consistently?
If you’re covering most of the basics, you might not need to do more. (Give yourself a pat on the back. You’re already elite!)
Or, maybe there’s some room for improvement and you’d like to step it up a bit. Great! For the vast majority of people, improving any of these behaviors will deliver real, tangible results. Start with these, before chasing faddish, fringe, “super-optimal” stuff.
4. Tune out the noise.
Those people you hear on podcasts or social media aren’t the experts on you and your life.
You get to decide what you want, and how to go about getting it.
Be honest with yourself, and make choices aligned with what matters most to you.
There’s plenty of advice out there, but remember: It’s your life. You get to make decisions that work for you.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- Dalton, Amy N., and Stephen A. Spiller. 2012. “Too Much of a Good Thing: The Benefits of Implementation Intentions Depend on the Number of Goals.” The Journal of Consumer Research 39 (3): 600–614.
- Diener, Ed, and Micaela Y. Chan. 2011. “Happy People Live Longer: Subjective Well-Being Contributes to Health and Longevity.” Applied Psychology. Health and Well-Being 3 (1): 1–43.
- Suarez-Lledo, Victor, and Javier Alvarez-Galvez. 2021. “Prevalence of Health Misinformation on Social Media: Systematic Review.” Journal of Medical Internet Research 23 (1): e17187.
- Crawford, Cindy, Bharathi Avula, Andrea T. Lindsey, Abraham Walter, Kumar Katragunta, Ikhlas A. Khan, and Patricia A. Deuster. 2022. “Analysis of Select Dietary Supplement Products Marketed to Support or Boost the Immune System.” JAMA Network Open 5 (8): e2226040.
- Crawford, Cindy, Courtney Boyd, Bharathi Avula, Yan-Hong Wang, Ikhlas A. Khan, and Patricia A. Deuster. 2020. “A Public Health Issue: Dietary Supplements Promoted for Brain Health and Cognitive Performance.” Journal of Alternative and Complementary Medicine (New York, N.Y.) 26 (4): 265–72.
- White, C. Michael. 2022. “Continued Risk of Dietary Supplements Adulterated with Approved and Unapproved Drugs: Assessment of the US Food and Drug Administration’s Tainted Supplements Database 2007 through 2021.” Journal of Clinical Pharmacology 62 (8): 928–34.
- Paffenbarger, R. S., Jr, R. T. Hyde, A. L. Wing, and C. C. Hsieh. 1986. “Physical Activity, All-Cause Mortality, and Longevity of College Alumni.” The New England Journal of Medicine 314 (10): 605–13.
- Watts, Eleanor L., Charles E. Matthews, Joshua R. Freeman, Jessica S. Gorzelitz, Hyokyoung G. Hong, Linda M. Liao, Kathleen M. McClain, Pedro F. Saint-Maurice, Eric J. Shiroma, and Steven C. Moore. 2022. “Association of Leisure Time Physical Activity Types and Risks of All-Cause, Cardiovascular, and Cancer Mortality among Older Adults.” JAMA Network Open 5 (8): e2228510.
- Jayedi, Ahmad, Ali Gohari, and Sakineh Shab-Bidar. 2022. “Daily Step Count and All-Cause Mortality: A Dose-Response Meta-Analysis of Prospective Cohort Studies.” Sports Medicine (Auckland, N.Z.) 52 (1): 89–99.
- Del Pozo Cruz, Borja, Matthew Ahmadi, Sharon L. Naismith, and Emmanuel Stamatakis. 2022. “Association of Daily Step Count and Intensity with Incident Dementia in 78 430 Adults Living in the UK.” JAMA Neurology 79 (10): 1059–63.
- Abou Sawan, Sidney; Nunes, Everson A.; Lim, Changhyun; McKendry, James; Phillips, Stuart M.. “The Health Benefits of Resistance Exercise: Beyond Hypertrophy and Big Weights.” Exercise, Sport, and Movement 1(1):e00001, Winter 2023.
- “Falls.” n.d. Accessed May 6, 2025. https://www.who.int/news-room/fact-sheets/detail/falls.
- Sadaqa, Munseef, Zsanett Németh, Alexandra Makai, Viktória Prémusz, and Márta Hock. 2023. “Effectiveness of Exercise Interventions on Fall Prevention in Ambulatory Community-Dwelling Older Adults: A Systematic Review with Narrative Synthesis.” Frontiers in Public Health 11 (August): 1209319.
- Massini, Danilo A., Flávio H. Nedog, Thiago P. de Oliveira, Tiago A. F. Almeida, Caroline A. A. Santana, Cassiano M. Neiva, Anderson G. Macedo, et al. 2022. “The Effect of Resistance Training on Bone Mineral Density in Older Adults: A Systematic Review and Meta-Analysis.” Healthcare (Basel, Switzerland) 10 (6): 1129.
- Park, Jung Ha, Ji Hyun Moon, Hyeon Ju Kim, Mi Hee Kong, and Yun Hwan Oh. 2020. “Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks.” Korean Journal of Family Medicine 41 (6): 365–73.
- Zisko, Nina, Kjerstin Næss Skjerve, Atefe R. Tari, Silvana Bucher Sandbakk, Ulrik Wisløff, Bjarne M. Nes, and Javaid Nauman. 2017. “Personal Activity Intelligence (PAI), Sedentary Behavior and Cardiovascular Risk Factor Clustering – the HUNT Study.” Progress in Cardiovascular Diseases 60 (1): 89–95.
- “Exercise or Physical Activity.” 2024. September 25, 2024. https://www.cdc.gov/nchs/fastats/exercise.htm.
- Carrard, Justin, Anne-Catherine Rigort, Christian Appenzeller-Herzog, Flora Colledge, Karsten Königstein, Timo Hinrichs, and Arno Schmidt-Trucksäss. 2022. “Diagnosing Overtraining Syndrome: A Scoping Review.” Sports Health 14 (5): 665–73.
- Weakley, Jonathon, Shona L. Halson, and Iñigo Mujika. 2022. “Overtraining Syndrome Symptoms and Diagnosis in Athletes: Where Is the Research? A Systematic Review.” International Journal of Sports Physiology and Performance 17 (5): 675–81.
- Breuckmann, Frank, Stefan Möhlenkamp, Kai Nassenstein, Nils Lehmann, Susanne Ladd, Axel Schmermund, Burkhard Sievers, et al. 2009. “Myocardial Late Gadolinium Enhancement: Prevalence, Pattern, and Prognostic Relevance in Marathon Runners.” Radiology 251 (1): 50–57.
- Wilson, M., R. O’Hanlon, S. Prasad, A. Deighan, P. Macmillan, D. Oxborough, R. Godfrey, et al. 2011. “Diverse Patterns of Myocardial Fibrosis in Lifelong, Veteran Endurance Athletes.” Journal of Applied Physiology (Bethesda, Md.: 1985) 110 (6): 1622–26.
- Möhlenkamp, Stefan, Nils Lehmann, Frank Breuckmann, Martina Bröcker-Preuss, Kai Nassenstein, Martin Halle, Thomas Budde, et al. 2008. “Running: The Risk of Coronary Events : Prevalence and Prognostic Relevance of Coronary Atherosclerosis in Marathon Runners.” European Heart Journal 29 (15): 1903–10.
- Müssigbrodt, A., A. Weber, J. Mandrola, Y. van Belle, S. Richter, M. Döring, A. Arya, P. Sommer, A. Bollmann, and G. Hindricks. 2017. “Excess of Exercise Increases the Risk of Atrial Fibrillation.” Scandinavian Journal of Medicine & Science in Sports 27 (9): 910–17.
- Eijsvogels, Thijs M. H., Paul D. Thompson, and Barry A. Franklin. 2018. “The ‘Extreme Exercise Hypothesis’: Recent Findings and Cardiovascular Health Implications.” Current Treatment Options in Cardiovascular Medicine 20 (10): 84.
- Franklin, Barry A., and Scott Billecke. 2012. “Putting the Benefits and Risks of Aerobic Exercise in Perspective.” Current Sports Medicine Reports 11 (4): 201–8.
- Oteng, Antwi-Boasiako, and Sander Kersten. 2020. “Mechanisms of Action of Trans Fatty Acids.” Advances in Nutrition 11 (3): 697–708.
- Souza, Russell J. de, Andrew Mente, Adriana Maroleanu, Adrian I. Cozma, Vanessa Ha, Teruko Kishibe, Elizabeth Uleryk, et al. 2015. “Intake of Saturated and Trans Unsaturated Fatty Acids and Risk of All Cause Mortality, Cardiovascular Disease, and Type 2 Diabetes: Systematic Review and Meta-Analysis of Observational Studies.” BMJ 351 (August): h3978.
- Dhaka, Vandana, Neelam Gulia, Kulveer Singh Ahlawat, and Bhupender Singh Khatkar. 2011. “Trans Fats-Sources, Health Risks and Alternative Approach – A Review.” Journal of Food Science and Technology 48 (5): 534–41.
- Ortega, Miguel A., Óscar Fraile-Martínez, Cielo García-Montero, Miguel Angel Alvarez-Mon, Guillermo Lahera, Jorge Monserrat, Maria Llavero-Valero, et al. 2022. “Biological Role of Nutrients, Food and Dietary Patterns in the Prevention and Clinical Management of Major Depressive Disorder.” Nutrients 14 (15): 3099.
- Piao, Jingjing, Yingwei Wang, Tianqi Zhang, Jiayu Zhao, Qianyu Lv, Mengyu Ruan, Qin Yu, and Bingjin Li. 2023. “Antidepressant-like Effects of Representative Types of Food and Their Possible Mechanisms.” Molecules (Basel, Switzerland) 28 (19): 6992.
- Saghafian, Faezeh, Hanieh Malmir, Parvane Saneei, Alireza Milajerdi, Bagher Larijani, and Ahmad Esmaillzadeh. 2018. “Fruit and Vegetable Consumption and Risk of Depression: Accumulative Evidence from an Updated Systematic Review and Meta-Analysis of Epidemiological Studies.” The British Journal of Nutrition 119 (10): 1087–1101.
- Juul, Filippa, Georgeta Vaidean, and Niyati Parekh. 2021. “Ultra-Processed Foods and Cardiovascular Diseases: Potential Mechanisms of Action.” Advances in Nutrition (Bethesda, Md.) 12 (5): 1673–80.
- Du, Shutong, Valerie K. Sullivan, Michael Fang, Lawrence J. Appel, Elizabeth Selvin, and Casey M. Rebholz. 2024. “Ultra-Processed Food Consumption and Risk of Diabetes: Results from a Population-Based Prospective Cohort.” Diabetologia 67 (10): 2225–35.
- Kliemann, Nathalie, Fernanda Rauber, Renata Bertazzi Levy, Vivian Viallon, Eszter P. Vamos, Reynalda Cordova, Heinz Freisling, et al. 2023. “Food Processing and Cancer Risk in Europe: Results from the Prospective EPIC Cohort Study.” The Lancet. Planetary Health 7 (3): e219–32.
- Fadnes, Lars T., Carlos Celis-Morales, Jan-Magnus Økland, Solange Parra-Soto, Katherine M. Livingstone, Frederick K. Ho, Jill P. Pell, et al. 2023. “Life Expectancy Can Increase by up to 10 Years Following Sustained Shifts towards Healthier Diets in the United Kingdom.” Nature Food 4 (11): 961–65.
- Lane, Melissa M., Elizabeth Gamage, Shutong Du, Deborah N. Ashtree, Amelia J. McGuinness, Sarah Gauci, Phillip Baker, et al. 2024. “Ultra-Processed Food Exposure and Adverse Health Outcomes: Umbrella Review of Epidemiological Meta-Analyses.” BMJ (Clinical Research Ed.) 384 (February): e077310.
- Rico-Campà, Anaïs, Miguel A. Martínez-González, Ismael Alvarez-Alvarez, Raquel de Deus Mendonça, Carmen de la Fuente-Arrillaga, Clara Gómez-Donoso, and Maira Bes-Rastrollo. 2019. “Association between Consumption of Ultra-Processed Foods and All Cause Mortality: SUN Prospective Cohort Study.” BMJ (Clinical Research Ed.) 365 (May): l1949.
- Wolfson, Julia A., Anna Claire Tucker, Cindy W. Leung, Casey M. Rebholz, Vanessa Garcia-Larsen, and Euridice Martinez-Steele. 2025. “Trends in Adults’ Intake of Un-Processed/Minimally Processed, and Ultra-Processed Foods at Home and Away from Home in the United States from 2003-2018.” The Journal of Nutrition 155 (1): 280–92.
- Wang, Dong D., Yanping Li, Shilpa N. Bhupathiraju, Bernard A. Rosner, Qi Sun, Edward L. Giovannucci, Eric B. Rimm, et al. 2021. “Fruit and Vegetable Intake and Mortality.” Circulation 143 (17): 1642–54.
- Boeing, Heiner, Angela Bechthold, Achim Bub, Sabine Ellinger, Dirk Haller, Anja Kroke, Eva Leschik-Bonnet, et al. 2012. “Critical Review: Vegetables and Fruit in the Prevention of Chronic Diseases.” European Journal of Nutrition 51 (6): 637–63.
- N.d. Accessed May 2, 2025. https://odphp.health.gov/sites/default/files/2019-09/2015-2020_Dietary_Guidelines.pdf.
- Lee-Kwan, Seung Hee, Latetia V. Moore, Heidi M. Blanck, Diane M. Harris, and Deb Galuska. 2017. “Disparities in State-Specific Adult Fruit and Vegetable Consumption – United States, 2015.” MMWR. Morbidity and Mortality Weekly Report 66 (45): 1241–47.
- Naghshi, Sina, Omid Sadeghi, Walter C. Willett, and Ahmad Esmaillzadeh. 2020. “Dietary Intake of Total, Animal, and Plant Proteins and Risk of All Cause, Cardiovascular, and Cancer Mortality: Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies.” BMJ (Clinical Research Ed.) 370 (July): m2412.
- Haghighatdoost, Fahimeh, Noushin Mohammadifard, Parisa Zakeri, Jamshid Najafian, Masoumeh Sadeghi, Hamidreza Roohafza, and Nizal Sarrafzadegan. 2023. “Differences in All-Cause Mortality Risk Associated with Animal and Plant Dietary Protein Sources Consumption.” Scientific Reports 13 (1): 3396.
- Chen, Zhangling, Marija Glisic, Mingyang Song, Hamid A. Aliahmad, Xiaofang Zhang, Alice C. Moumdjian, Valentina Gonzalez-Jaramillo, et al. 2020. “Dietary Protein Intake and All-Cause and Cause-Specific Mortality: Results from the Rotterdam Study and a Meta-Analysis of Prospective Cohort Studies.” European Journal of Epidemiology 35 (5): 411–29.
- N.d. Accessed May 2, 2025. https://www.aicr.org/cancer-prevention/recommendations/limit-consumption-of-red-and-processed-meat/#what-the-science-says.
- “Cancer: Carcinogenicity of the Consumption of Red Meat and Processed Meat.” n.d. Accessed May 2, 2025. https://www.who.int/news-room/questions-and-answers/item/cancer-carcinogenicity-of-the-consumption-of-red-meat-and-processed-meat.
- Li, Chunxiao, Tom R. P. Bishop, Fumiaki Imamura, Stephen J. Sharp, Matthew Pearce, Soren Brage, Ken K. Ong, et al. 2024. “Meat Consumption and Incident Type 2 Diabetes: An Individual-Participant Federated Meta-Analysis of 1·97 Million Adults with 100 000 Incident Cases from 31 Cohorts in 20 Countries.” The Lancet. Diabetes & Endocrinology 12 (9): 619–30.
- Phillips, Stuart M., Stéphanie Chevalier, and Heather J. Leidy. 2016. “Protein ‘Requirements’ beyond the RDA: Implications for Optimizing Health.” Applied Physiology Nutrition and Metabolism 41 (5): 565–72.
- Houston, Denise K., Barbara J. Nicklas, Jingzhong Ding, Tamara B. Harris, Frances A. Tylavsky, Anne B. Newman, Jung Sun Lee, et al. 2008. “Dietary Protein Intake Is Associated with Lean Mass Change in Older, Community-Dwelling Adults: The Health, Aging, and Body Composition (Health ABC) Study.” The American Journal of Clinical Nutrition 87 (1): 150–55.
- Hengeveld, Linda M., Jolanda M. A. Boer, Pierrette Gaudreau, Martijn W. Heymans, Carol Jagger, Nuno Mendonça, Marga C. Ocké, et al. 2020. “Prevalence of Protein Intake below Recommended in Community-Dwelling Older Adults: A Meta-Analysis across Cohorts from the PROMISS Consortium.” Journal of Cachexia, Sarcopenia and Muscle 11 (5): 1212–22.
- Bischoff-Ferrari, Heike A., Stephanie Gängler, Maud Wieczorek, Daniel W. Belsky, Joanne Ryan, Reto W. Kressig, Hannes B. Stähelin, et al. 2025. “Individual and Additive Effects of Vitamin D, Omega-3 and Exercise on DNA Methylation Clocks of Biological Aging in Older Adults from the DO-HEALTH Trial.” Nature Aging 5 (3): 376–85.
- Navarro, Victor J., Ikhlas Khan, Einar Björnsson, Leonard B. Seeff, Jose Serrano, and Jay H. Hoofnagle. 2017. “Liver Injury from Herbal and Dietary Supplements.” Hepatology (Baltimore, Md.) 65 (1): 363–73.
- Li, H., F. Qian, L. Han, W. Feng, D. Zheng, X. Guo, and H. Zhang. 2024. “Association of Healthy Sleep Patterns with Risk of Mortality and Life Expectancy at Age of 30 Years: A Population-Based Cohort Study.” QJM: Monthly Journal of the Association of Physicians 117 (3): 177–86.
- Makarem, Nour, Cecilia Castro-Diehl, Marie-Pierre St-Onge, Susan Redline, Steven Shea, Donald Lloyd-Jones, Hongyan Ning, and Brooke Aggarwal. 2022. “Redefining Cardiovascular Health to Include Sleep: Prospective Associations with Cardiovascular Disease in the MESA Sleep Study.” Journal of the American Heart Association 11 (21): e025252.
- Chaput, Jean-Philippe, Caroline Dutil, Ryan Featherstone, Robert Ross, Lora Giangregorio, Travis J. Saunders, Ian Janssen, et al. 2020. “Sleep Duration and Health in Adults: An Overview of Systematic Reviews.” Applied Physiology Nutrition and Metabolism 45 (10 (Suppl. 2)): S218–31.
- Winer, Joseph R., Kacie D. Deters, Gabriel Kennedy, Meghan Jin, Andrea Goldstein-Piekarski, Kathleen L. Poston, and Elizabeth C. Mormino. 2021. “Association of Short and Long Sleep Duration with Amyloid-β Burden and Cognition in Aging.” JAMA Neurology 78 (10): 1187–96.
- “Sleep Health.” 2023. December 27, 2023. https://www.cdc.gov/nchs/fastats/sleep-health.htm.
- Han, Han, Ying Wang, Tongtong Li, Chengwu Feng, Catherine Kaliszewski, Yang Su, Yinfan Wu, Jian Zhou, Liang Wang, and Geng Zong. 2023. “Sleep Duration and Risks of Incident Cardiovascular Disease and Mortality among People with Type 2 Diabetes.” Diabetes Care 46 (1): 101–10.
- Wang, Yafeng, Wentao Huang, Adrienne O’Neil, Yutao Lan, Dagfinn Aune, Wei Wang, Chuanhua Yu, and Xiong Chen. 2020. “Association between Sleep Duration and Mortality Risk among Adults with Type 2 Diabetes: A Prospective Cohort Study.” Diabetologia 63 (11): 2292–2304.
- Jike, Maki, Osamu Itani, Norio Watanabe, Daniel J. Buysse, and Yoshitaka Kaneita. 2018. “Long Sleep Duration and Health Outcomes: A Systematic Review, Meta-Analysis and Meta-Regression.” Sleep Medicine Reviews 39 (June): 25–36.
- Satyjeet, Fnu, Sidra Naz, Vinesh Kumar, Norah H. Aung, Kanwal Bansari, Sana Irfan, and Amber Rizwan. 2020. “Psychological Stress as a Risk Factor for Cardiovascular Disease: A Case-Control Study.” Cureus 12 (10): e10757.
- Vaccarino, Viola, and J. Douglas Bremner. 2024. “Stress and Cardiovascular Disease: An Update.” Nature Reviews. Cardiology 21 (9): 603–16.
- Ebstrup, Jeanette Frost, and Torben Jørgensen. 2012. “Stress and cardiovascular disease.” Ugeskrift for laeger 174 (4): 204–7.
- Schneiderman, Neil, Gail Ironson, and Scott D. Siegel. 2005. “Stress and Health: Psychological, Behavioral, and Biological Determinants.” Annual Review of Clinical Psychology 1 (1): 607–28.
- N.d. Accessed May 2, 2025. https://www.apa.org/news/press/releases/2021/03/one-year-pandemic-stress#:~:text=Nearly.
- Neff, Kristin D. 2023. “Self-Compassion: Theory, Method, Research, and Intervention.” Annual Review of Psychology 74 (1): 193–218.
- Dweck CS. Mindset: The New Psychology of Success. Random House Publishing Group; 2006.
- Jamieson, Jeremy P., Alia J. Crum, J. Parker Goyer, Marisa E. Marotta, and Modupe Akinola. 2018. “Optimizing Stress Responses with Reappraisal and Mindset Interventions: An Integrated Model.” Anxiety, Stress, and Coping 31 (3): 245–61.
- N.d. Accessed May 2, 2025. https://www.apa.org/news/press/releases/stress/2022/concerned-future-inflation.
- Government of Canada, and Statistics Canada. 2023. “Perceived Life Stress, by Age Group.” Government of Canada, Statistics Canada. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009604.
- N.d. Accessed May 2, 2025. https://www.apa.org/news/press/releases/stress/2023/collective-trauma-recovery.
- N.d. Accessed May 2, 2025. https://nap.nationalacademies.org/catalog/25663/social-isolation-and-loneliness-in-older-adults-opportunities-for-the.
- Reblin, Maija, and Bert N. Uchino. 2008. “Social and Emotional Support and Its Implication for Health.” Current Opinion in Psychiatry 21 (2): 201–5.
- Holt-Lunstad, Julianne, Timothy B. Smith, and J. Bradley Layton. 2010. “Social Relationships and Mortality Risk: A Meta-Analytic Review.” PLoS Medicine 7 (7): e1000316.
- “Harvard Second Generation Study.” n.d. Harvardstudy. Accessed May 2, 2025. https://www.adultdevelopmentstudy.org/.
- CDC. 2025. “Health Effects of Social Isolation and Loneliness.” Social Connection. February 3, 2025. https://www.cdc.gov/social-connectedness/risk-factors/.
- “Loneliness Linked to Dementia Risk in Large-Scale Analysis.” n.d. National Institute on Aging. Accessed May 2, 2025. https://www.nia.nih.gov/news/loneliness-linked-dementia-risk-large-scale-analysis.
- Holt-Lunstad, Julianne. 2024. “Social Connection as a Critical Factor for Mental and Physical Health: Evidence, Trends, Challenges, and Future Implications.” World Psychiatry: Official Journal of the World Psychiatric Association (WPA) 23 (3): 312–32.
- N.d. Accessed May 2, 2025. https://www.hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf.
- Goddard, Isabel. 2023. “What Does Friendship Look like in America?” Pew Research Center. October 12, 2023. https://www.pewresearch.org/short-reads/2023/10/12/what-does-friendship-look-like-in-america/.
- Martino, Jessica, Jennifer Pegg, and Elizabeth Pegg Frates. 2017. “The Connection Prescription: Using the Power of Social Interactions and the Deep Desire for Connectedness to Empower Health and Wellness.” American Journal of Lifestyle Medicine 11 (6): 466–75.
- Kang, Weixi. 2023. “Understanding the Associations between the Number of Close Friends and Life Satisfaction: Considering Age Differences.” Frontiers in Psychology 14 (March): 1105771.
- Dunbar, Robin. 2011. “How Many ‘Friends’ Can You Really Have?” IEEE Spectrum 48 (6): 81–83.
- Steptoe, Andrew, Aparna Shankar, Panayotes Demakakos, and Jane Wardle. 2013. “Social Isolation, Loneliness, and All-Cause Mortality in Older Men and Women.” Proceedings of the National Academy of Sciences of the United States of America 110 (15): 5797–5801.
- Falci, Christina & McNeely, Clea. (2009). “Too Many Friends: Social Integration, Network Cohesion and Adolescent Depressive Symptoms.” Social Forces – SOC FORCES. 87. 10.1353/sof.0.0189.
- Stavrova, Olga, and Dongning Ren. 2021. “Is More Always Better? Examining the Nonlinear Association of Social Contact Frequency with Physical Health and Longevity.” Social Psychological and Personality Science 12 (6): 1058–70.
- Leikas, Sointu, and Ville-Juhani Ilmarinen. 2017. “Happy Now, Tired Later? Extraverted and Conscientious Behavior Are Related to Immediate Mood Gains, but to Later Fatigue.” Journal of Personality 85 (5): 603–15.
- “Cigarette Smoking and Electronic Cigarette Use.” 2024. September 4, 2024. https://www.cdc.gov/nchs/fastats/smoking.htm.
- N.d. Accessed May 2, 2025. https://ourworldindata.org/smoking.
- “Tobacco.” n.d. Accessed May 2, 2025. https://www.who.int/news-room/fact-sheets/detail/tobacco.
- US Burden of Disease Collaborators, Ali H. Mokdad, Katherine Ballestros, Michelle Echko, Scott Glenn, Helen E. Olsen, Erin Mullany, et al. 2018. “The State of US Health, 1990-2016: Burden of Diseases, Injuries, and Risk Factors among US States.” JAMA: The Journal of the American Medical Association 319 (14): 1444–72.
- National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. 2014. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US).
- Manuello, Jordi, Joosung Min, Paul McCarthy, Fidel Alfaro-Almagro, Soojin Lee, Stephen Smith, Lloyd T. Elliott, Anderson M. Winkler, and Gwenaëlle Douaud. 2024. “The Effects of Genetic and Modifiable Risk Factors on Brain Regions Vulnerable to Ageing and Disease.” Nature Communications 15 (1): 2576.
- Livingston, Gill, Jonathan Huntley, Andrew Sommerlad, David Ames, Clive Ballard, Sube Banerjee, Carol Brayne, et al. 2020. “Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission.” Lancet 396 (10248): 413–46.
- “Alcohol.” n.d. Accessed May 2, 2025. https://www.who.int/news-room/fact-sheets/detail/alcohol.
- GBD 2016 Alcohol Collaborators. 2018. “Alcohol Use and Burden for 195 Countries and Territories, 1990-2016: A Systematic Analysis for the Global Burden of Disease Study 2016.” Lancet 392 (10152): 1015–35.
- N.d. Accessed May 2, 2025. https://www.dietaryguidelines.gov/alcohol/info.
- “Surveillance Report #120.” n.d. Accessed May 2, 2025. https://www.niaaa.nih.gov/publications/surveillance-reports/surveillance120.
- Livingston, Michael, and Sarah Callinan. 2015. “Underreporting in Alcohol Surveys: Whose Drinking Is Underestimated?” Journal of Studies on Alcohol and Drugs 76 (1): 158–64.
- Boniface, Sadie, James Kneale, and Nicola Shelton. 2014. “Drinking Pattern Is More Strongly Associated with Under-Reporting of Alcohol Consumption than Socio-Demographic Factors: Evidence from a Mixed-Methods Study.” BMC Public Health 14 (1): 1297.
- N.d. Accessed May 2, 2025. https://ourworldindata.org/alcohol-consumption.
- Spencer, Merianne Rose, Sally C. Curtin, and Holly Hedegaard. 2020. “Rates of Alcohol-Induced Deaths among Adults Aged 25 and over in Urban and Rural Areas: United States, 2000-2018.” NCHS Data Brief, no. 383 (October): 1–8.
- “No Level of Alcohol Consumption Is Safe for Our Health.” n.d. Accessed May 2, 2025. https://www.who.int/europe/news/item/04-01-2023-no-level-of-alcohol-consumption-is-safe-for-our-health.
- Biddinger KJ, Emdin CA, Haas ME, et al. “Association of Habitual Alcohol Intake With Risk of Cardiovascular Disease.” JAMA Netw Open. 2022;5(3):e223849.
- Kahane, Work by Charles. n.d. “Lives Saved by Vehicle Safety Technologies 1960 to 2012.” Accessed May 2, 2025. https://www.nhtsa.gov/sites/nhtsa.gov/files/2015sae-kindelberger-livessaved.pdf.
- Green, A., G. Williams, R. Neale, V. Hart, D. Leslie, P. Parsons, G. C. Marks, et al. 1999. “Daily Sunscreen Application and Betacarotene Supplementation in Prevention of Basal-Cell and Squamous-Cell Carcinomas of the Skin: A Randomised Controlled Trial.” Lancet 354 (9180): 723–29.
- Green, Adèle C., Gail M. Williams, Valerie Logan, and Geoffrey M. Strutton. 2011. “Reduced Melanoma after Regular Sunscreen Use: Randomized Trial Follow-Up.” Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology 29 (3): 257–63.
- Tan, Yunfei, Lili Fang, Yichen Zhu, and Kenji Hashimoto. 2024. “Relationship between Hearing Loss and Depression: A Cross-Sectional Analysis from the National Health and Nutrition Examination Survey 2015-2018.” Journal of Psychiatric Research 178 (October): 1–7.
- Bigelow, Robin T., Nicholas S. Reed, Katharine K. Brewster, Alison Huang, George Rebok, Bret R. Rutherford, and Frank R. Lin. 2020. “Association of Hearing Loss with Psychological Distress and Utilization of Mental Health Services among Adults in the United States.” JAMA Network Open 3 (7): e2010986.
- Wang, Hui-Fu, Wei Zhang, Edmund T. Rolls, Alzheimer’s Disease Neuroimaging Initiative, Yuzhu Li, Linbo Wang, Ya-Hui Ma, et al. 2022. “Hearing Impairment Is Associated with Cognitive Decline, Brain Atrophy and Tau Pathology.” EBioMedicine 86 (104336): 104336.
- Huang, Alison R., Kening Jiang, Frank R. Lin, Jennifer A. Deal, and Nicholas S. Reed. 2023. “Hearing Loss and Dementia Prevalence in Older Adults in the US.” JAMA: The Journal of the American Medical Association 329 (2): 171–73.
- Hung, Shih-Chang, Kuan-Fu Liao, Chih-Hsin Muo, Shih-Wei Lai, Chia-Wei Chang, and Hung-Chang Hung. 2015. “Hearing Loss Is Associated with Risk of Alzheimer’s Disease: A Case-Control Study in Older People.” Journal of Epidemiology 25 (8): 517–21.
- Campos, Laura, Allan Prochazka, Melinda Anderson, Alexander Kaizer, Carol Foster, and Timothy Hullar. 2023. “Consistent Hearing Aid Use Is Associated with Lower Fall Prevalence and Risk in Older Adults with Hearing Loss.” Journal of the American Geriatrics Society 71 (10): 3163–71.
- Riska, Kristal M., Sarah B. Peskoe, Maragatha Kuchibhatla, Alexander Gordee, Juliessa M. Pavon, Se Eun Kim, Jessica S. West, and Sherri L. Smith. 2022. “Impact of Hearing Aid Use on Falls and Falls-Related Injury: Results from the Health and Retirement Study.” Ear and Hearing 43 (2): 487–94.
- N.d. Accessed May 2, 2025. https://injuryfacts.nsc.org/motor-vehicle/occupant-protection/seat-belts/.
- Fleming, Eleanor B., Duong Nguyen, Joseph Afful, Margaret D. Carroll, and Phillip D. Woods. 2018. “Prevalence of Daily Flossing among Adults by Selected Risk Factors for Periodontal Disease-United States, 2011-2014.” Journal of Periodontology 89 (8): 933–39.
- Olsson, Bjørn. 2023. “Increased Bicycle Helmet Use in the Absence of Mandatory Bicycle Helmet Legislation: Prevalence and Trends from Longitudinal Observational Studies on the Use of Bicycle Helmets among Cyclists in Denmark 2004-2022.” Journal of Safety Research 87 (December): 54–63.
- Bonyun, Marissa, Andi Camden, Colin Macarthur, and Andrew Howard. 2012. “Helmet Use in BIXI Cyclists in Toronto, Canada: An Observational Study.” BMJ Open 2 (3): e001049.
- Shool, Sina, Seyed Mohammad Piri, Zahra Ghodsi, Reza Tabrizi, Mohammad Hosein Amirzade-Iranaq, Mahdieh Mashayekhi, Mohammad Amin Dabbagh Ohadi, et al. 2024. “The Prevalence of Helmet Use in Motorcyclists around the World: A Systematic Review and Meta-Analysis of 5,006,476 Participants.” International Journal of Injury Control and Safety Promotion 31 (3): 431–69.
- Waltzman, Dana, Kelly Sarmiento, Xinjian Zhang, and Gabrielle F. Miller. 2023. “Estimated Prevalence of Helmet Use While Bicycling, Rollerblading, and Skateboarding among Middle School Students in Selected U.S. States- Youth Behavior Risk Survey, 2013-2019.” Journal of Safety Research 87 (December): 367–74.
- Livingston, Gill, Jonathan Huntley, Andrew Sommerlad, David Ames, Clive Ballard, Sube Banerjee, Carol Brayne, et al. 2020. “Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission.” Lancet 396 (10248): 413–46.
- Kim, Eric S., Ying Chen, Julia S. Nakamura, Carol D. Ryff, and Tyler J. VanderWeele. 2022. “Sense of Purpose in Life and Subsequent Physical, Behavioral, and Psychosocial Health: An Outcome-Wide Approach.” American Journal of Health Promotion: AJHP 36 (1): 137–47.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)
The post The True Cost of “Optimal” Health appeared first on Precision Nutrition.
Source: Health1
Are vegetable and seed oils “toxic”?!
From TikTok to bestseller lists, vegetable oils—a.k.a. “seed oils”—are a big topic right now.
To be fair, folks have debated the merits of vegetable oils dating back to when they first entered the marketplace.
More recently, however, with the advent of the carnivore diet, vegetable oil hate has roared back into the socials. Maybe you’ve come across posts that refer to these cooking oils as “toxic sludge,” “motor oil,” “the hateful eight,” and “the biggest cause of chronic disease that nobody knows about.”
The anti-vegetable oil logic goes something like this…
Animal fats have been with humans for thousands of years. Vegetable fats, on the other hand, were invented during the last century when profit-seeking companies wanted to find a way to sell cheap-to-grow foods to unsuspecting consumers.
Another argument: Like margarine, vegetable oils were marketed as healthier alternatives for butter, and yet, people argue, these oils are worse than butter, raising your risk for obesity, anxiety, depression, ulcerative colitis, and more.
In contrast to the above line of thought, other experts will tell you that vegetable oils are harmless, potentially even health-promoting—and absolutely better than butter.
So, who’s right?
Like so many nutrition topics, the truth is too nuanced to fit on a meme.
In this story, we’ll help you sort the science from the pseudoscience so you can make informed decisions about the oils you choose to include in your diet.
What are vegetable oils?
Sometimes called “seed oils,” vegetable oils start, as you might suspect, from the seed of a plant. The most common ones you’ll find in a typical grocery aisle include:
- Canola oil
- Corn oil
- Safflower oil
- Sesame oil
- Sunflower oil
- Soybean oil
- Grapeseed oil
By the way, if you feel like there’s a bunch of oils missing from that list, it’s probably because those oils come from non-seed plants (such as olive, avocado, palm, or coconut oil, which all come from fruits, and aren’t considered vegetable or seed oils).
How are vegetable oils processed?
Non-vegetable oils—such as olive and avocado oil—are derived from naturally fatty foods. In fact, olives are so oily that you could theoretically make your own olive oil at home. (Just Google “how to make olive oil from scratch,” and you’ll find a number of videos walking you through the steps.)
The same can’t be said of most vegetable oils, which mostly come from foods with a relatively tiny fat content to begin with.
Case in point: A cup of green olives contains about 20 grams of fat,1 whereas a cup of corn has 2 grams.2
As a result, manufacturers must use an extensive multi-step process to extract this small amount of oil from these non-oily foods. These steps include:
- Crushing: A machine uses high pressure to press oil from the seeds.
- Refining: The seeds are heated with a solvent, such as hexane, to extract more oil.
- Deodorizing: To create a neutral taste and remove unwanted compounds, the extracted oil is then cooked at 400 F (204 C) for several hours.
During this process, health-promoting polyphenols and other stabilizing nutrients are lost, and small amounts of unsaturated fats are transformed into trans fatty acids (also called partially hydrogenated fat).
(Interesting fact: This also happens during deep frying. When vegetable oils sizzle in a restaurant’s deep fryer for hours, the trans fat content of the oil increases.)
To call these processed oils “toxic” might be an exaggeration. However, nutrition scientists generally agree that people should avoid trans fats in the diet, and in 2018, the Food and Drug Administration banned manufacturers from adding trans fats to processed foods.3 4
What cooking oils should you eat?
At PN, we’ve created several visual guides people can use to make informed decisions about what to eat.
(We’ve also created a shopping list, which you or your clients can print out and take to the grocery store. Check it out: Healthy Fats Shopping List)
In these guides, we’ve placed a few vegetable oils—expeller-pressed canola oil, high-oleic sunflower, and safflower oils—in the “Eat Some” section. For us, “eat some” is another way of saying that these foods will neither improve health nor harm health—when consumed in reasonable amounts. In some cases, like in the example of dark chocolate, when consumed in small amounts, they might even improve health.
The rest of the vegetable oils, along with butter and other saturated fats, fall into the “Eat Less” category, as the image below shows. You’ll find vegetable oils in bold.

We’ve gotten hate mail from folks who say certain vegetable oils—especially cold-pressed canola oil—should appear alongside olive oil in the “eat more” category. Plenty of others say all vegetable oils belong in the “eat less” column, and that butter belongs in “eat some” or even “eat more.”
To understand the scientific reasoning behind our recommendations, let’s explore some head-to-head matchups.
Extra-virgin olive oil vs. expeller-pressed canola oil
These oils are the least refined of their kind.
To make extra virgin olive oil (EVOO), manufacturers grind and mechanically press olives, without using any heat. Similarly, expeller-pressed canola oil is made by mechanically pressing rapeseed, without the use of heat or chemical solvents.
 The case for extra virgin olive oil (EVOO)
The case for extra virgin olive oil (EVOO)
Olive oil is richer in heart-healthy monounsaturated fatty acids (MUFAs) than almost any other cooking oil.
In addition, unlike the more refined “light” olive oil, EVOO maintains most of the olive fruit’s original polyphenols. These plant-based substances help to combat inflammation and protect cells from damage.
Perhaps most importantly…
More studies vouch for EVOO’s health-promoting qualities than for any other cooking fat.
For example, researchers asked 22,892 adults from Southern Italy to self-report their olive oil consumption. People who consumed the most olive oil (more than two tablespoons a day) were 20 percent less likely to die over the 13-year study than people who consumed the least olive oil (less than one tablespoon a day).5
Other research has linked the consumption of olive oil with a reduced risk of:
- High blood pressure6
- Heart disease
- Type 2 diabetes7
- Dementia8
- Cancer9
Consumption of olive oil is also associated with reductions in LDL cholesterol, especially when used to replace saturated fats like butter and coconut oil.10
Smoke point: Should you avoid cooking with olive oil?
Years ago, culinary experts recommended using EVOO only on salads and other uncooked foods. Back then, they assumed EVOO’s relatively low smoke point (350 to 410F) meant the oil would break down when heated, losing some of its distinctive flavor and health benefits.
We now know that smoke point isn’t as big a deal as previously thought.
That’s especially true in the case of EVOO, whose polyphenols and high concentrations of monounsaturated fats help keep the oil stable when heated.
In research that heated a variety of cooking oils to 464 F (240C) and then held them at 356 F (180C) for several hours, EVOO remained more stable than any other oil tested, including canola oil.11
 The case for expeller-pressed canola oil
The case for expeller-pressed canola oil
One of the more affordable cooking oils on the shelf, canola oil, is made from a Canadian-made hybrid of the rapeseed plant.
(The word “canola” refers to the first three letters of “Canada” with a fun “ola” added to the end for marketing purposes.)12
Among vegetable oils, canola is the richest in heart-healthy monounsaturated fats (though several non-vegetable oils have it beat) as well as alpha-linolenic acid, a plant-based omega-3 fatty acid.
In addition, canola oil contains plant substances called phytosterols that help influence blood cholesterol for the better, especially when used as a substitute for butter, research has found.13 14 15
The winner
Extra virgin olive oil is the clear winner.
The body of research in support of EVOO dwarfs the body of research in support of expeller-pressed canola.
In addition, EVOO has a more favorable fatty acid profile. By the way, so does avocado oil, which is why you’ll also find it in the “eat more” column.
However, you can buy roughly twice as much expeller-pressed canola oil for half as much money as EVOO. Because of this, expeller-pressed canola can be a good budget-friendly choice. In addition, because of expeller-pressed canola’s more neutral flavor, many people prefer it over EVOO for baking.
When used in moderation, expeller-pressed canola can be part of a healthy diet. It is likely to be at least health neutral, if not somewhat health beneficial.
Expeller-pressed canola oil vs. refined canola oil
This match-up comes down to how processing methods affect the end product.
 Expeller-pressed canola oil
Expeller-pressed canola oil
An expeller press is a machine that squeezes oil out of seeds.
It’s able to do this without the use of solvents or heat, which helps preserve beneficial compounds such as alpha-linolenic acid and phytosterols.
 Refined canola oil
Refined canola oil
Refining removes some protective alpha-linoleic acid while adding small amounts of unhealthy trans fatty acids. This results in a product that is proportionally lower in omega-3 fatty acids and higher in omega-6 fatty acids.
The winner
Expeller-pressed canola oil wins, but only by a small margin.
That’s because canola oil starts with a less controversial fatty acid profile than many other vegetable oils, as the chart below shows. Soybean oil, for example, has less heart-healthy monounsaturated fat and much more theoretically inflammation-contributing omega-6 fat.

Are omega 6 fatty acids “inflammatory?”
The typical American consumes around 16 to 20 times more omega-6 fats than omega-3s.
This imbalance could theoretically increase inflammation in your body, potentially raising your risk for diabetes, obesity, and other health problems, argue some experts.16
Years ago, the recommendation to balance your omega 6s with omega 3s was widespread. (The suggested “ideal” ratio: Anywhere from 1:1 to 4:1, in favor of omega 6s.)
These days, there’s more debate among nutritional scientists as to whether this imbalance contributes to chronic inflammation, especially when those omega 6s are consumed in whole foods that contain many other beneficial compounds.
For example, nuts and seeds—both naturally rich in omega-6 fats—have been associated with a range of health benefits, including reductions in blood cholesterol and inflammation.17 18
In 2019, Harvard Health ran the headline “No need to avoid healthy omega-6 fats.” In support of their argument, a 2019 study from the American Heart Association journal Circulation determined that, if anything, the consumption of omega-6 fats reduced the risk for stroke, heart disease, and early death.19
However, while nuts and refined canola oil may share a somewhat similar fatty acid profile, the two foods differ in one important way. As we mentioned earlier, refined canola oil is basically pure oil. Meanwhile, nuts and seeds come packaged with health-protective fiber, polyphenols, protein, vitamins, and minerals.
Minimally-processed foods, like nuts or extra virgin oils, include a complex matrix of health-promoting nutrients. Highly-processed oils, on the other hand, have lost the vast majority of those healthful compounds, leaving mostly just the fatty acids which are more prone to oxidation (we’ll cover that next).
Refined vegetable oil oil vs. butter
This is the match-up that triggers the most arguing on the interwebs.
Let’s cover the major claims from both sides—plus what the research says.
 The case for butter
The case for butter
Butter proponents argue that saturated fats have been unnecessarily vilified. They point to nutrition recommendations during the 1980s and 1990s that recommended people replace butter with trans-fat rich margarine.
(We all know how that went.)
Margarine aside, others claim the research in support of reducing saturated fats is thin at best.20
However, excessive saturated fat consumption (beyond 10 percent of total calories) does seem to boost cholesterol levels and may increase your risk of heart disease.21
Some research has found that replacing 5 percent of the saturated fats in your diet with monounsaturated fats could reduce the risk of heart disease by 15 percent. Similarly, replacing 5 percent of the saturated fats in your diet with polyunsaturated fats (with most of that coming from refined vegetable oils) reduces the risk of a future heart attack by 10 percent, according to an analysis of eight studies involving 13,614 people.22 Many other studies support this finding.23
But not all saturated fats affect blood cholesterol equally. In some dairy foods, a membrane—called a milk fat globule membrane—surrounds the saturated fats and seems to limit their cholesterol-raising properties.
However, butter is low in this protective membrane, and consequently raises blood cholesterol more than other high-fat dairy products, like full-fat milk, cream, yogurt, or cheese.24 25 26
The U.S. Dietary Guidelines recommend capping saturated fat at less than 10 percent of your calorie intake. A tablespoon of butter contains 7 grams of saturated fat—a third of the recommended daily limit in a 2000 Calorie diet.
So, while you don’t necessarily need to eliminate butter, it’s worth moderating your intake.
(Interested in learning about all the nuances of saturated fat consumption? Read: Is saturated fat good or bad for you?)
 The case for refined vegetable oils
The case for refined vegetable oils
Due to their chemical structure, polyunsaturated fats are inherently less stable and more prone to oxidation than saturated or monounsaturated fats.
During the refining process, protective phytochemicals and antioxidants are stripped, making these oils more prone to oxidation. The theory is that this oxidation increases inflammation in the body and elevates the risk of various health conditions.
There’s some evidence to suggest that diets rich in polyunsaturated fats, especially from refined vegetable oils, are associated with increased levels of oxidized blood lipids, lipid peroxidation, and other markers of inflammation.27 28
If you only use refined corn or safflower oils to lightly coat veggies before roasting them, you likely don’t have much to worry about.
However, for the vast majority of people, the biggest source of refined vegetable oils isn’t home-cooked meals—it’s ultra-processed foods.
The extra processing and repeated heat exposure used to create ultra-processed foods further oxidize these oils. Additionally, these foods are often loaded with potentially harmful ingredients like added sodium and sugars, and low in beneficial nutrients like fiber, vitamins, minerals, and phytonutrients.
Plus, they’re incredibly calorie-dense and difficult to stop eating, which can raise your risk for obesity. (Find out exactly why highly-processed foods are so “addictive”: Why you can’t stop eating ultra-processed foods.)
Most ultra-processed foods list one or more vegetable oils as one of their ingredients. Even ultra-processed foods that you wouldn’t think of as “fatty” contain small amounts. You’ll find them in store-bought cookies, chips, crackers, sauces, frozen dinners, meal replacement shakes, boxed macaroni and cheese, salad dressing, boxed rice blends, and more.
In a large review involving nearly 10 million people, the consumption of ultra-processed foods was associated with a higher risk of premature death.29 In addition, studies have linked high consumption of ultra-processed foods with the following health problems:30 31 32 33
- Heart disease and heart attacks
- Stroke
- High blood pressure
- Depression
- Overweight and obesity
- Diabetes
- Reduced HDL cholesterol
- Cancer
You don’t have to abolish ultra-processed foods.
But your health will benefit from capping your consumption to about 20 percent or so of your intake, with the other 80 percent or so from mostly minimally-processed whole foods.
This alone will naturally lower your refined vegetable oil intake to a safer level, without much fuss. Plus, consuming refined vegetable oils in the context of a diet that’s rich in colorful plants, fiber, phytochemicals, and antioxidants may help offset the concern of oxidation. (For example, by putting a reasonable amount of commercial salad dressing on a large, colorful salad.)
The winner
This match-up is a draw.
Ultimately, both should be limited in the diet, and neither are health-promoting.
Most refined vegetable oils are lopsidedly rich in polyunsaturated fatty acids compared to monounsaturated fats, and are stripped of many protective compounds. As mentioned earlier, some experts argue that these omega-6-rich fats may contribute to inflammation (but the evidence here is mixed). Because of how they’re processed, seed oils also contain some of those trans fats that everyone agrees we should all minimize.
In contrast, butter is low in omega 6s but high in saturated fat, which can be problematic in higher amounts. Especially since it’s so low in the protective milk fat globule membrane. However, compared to refined vegetable oil, butter is less processed. Like olive oil, it’s one of those fats you could theoretically make at home.
Some final parting advice
This might be obvious from the head-to-head matchups, but we’ll say it anyway.
If you like it and can afford it, EVOO is a great choice.
Cold-pressed avocado oil and walnut oil are also great options, as both are rich in antioxidant compounds. Like EVOO, avocado oil is a rich source of MUFAs. Walnut oil’s fat primarily comes from polyunsaturated fats, so it’s best used as a dressing rather than used for cooking (as it’s less heat stable).
However, like EVOO, avocado and walnut oil tend to be expensive. If you or your client are budget-conscious, expeller-pressed canola oil is a solid runner-up.
Similarly, high-oleic sunflower and safflower oils are richer sources of monounsaturated fats than their high-linoleic cousins. When substituted for saturated fats like butter, high-oleic oils have been associated with cardiovascular benefits.34 35
Regardless of what cooking fats you or your client choose, you’ll also want to do the following:
 Prioritize minimally-processed whole foods.
Prioritize minimally-processed whole foods.
Whole and minimally-processed foods—such as nuts, seeds, avocados, olives, and salmon—are more likely to feature health-promoting monounsaturated (MUFAs) and omega-3 fats. They also come packaged with a wide array of other good-for-you nutrients such as fiber, protein, minerals, and antioxidants.
In contrast, ultra-professed foods are generally devoid of everything you keep hearing you should consume more of. These foods also tend to be calorie-dense, highly rewarding, and hard to stop eating.
If you’re not sure whether packaged food is minimally processed or highly processed, take a close look and consider:
- Does anything in nature resemble this food?
- Does it look like it came from an animal or a plant?
- If you look at the list of ingredients, do you see animal or plant components?
If you answer “no” to most of the above, the food is likely highly processed.
 Limit deep-fried foods.
Limit deep-fried foods.
It doesn’t matter what source of fat is used to fry them.
Sort all fried foods into the “eat less” category.
 Get most of your fats from food, not oils.
Get most of your fats from food, not oils.
EVOO is associated with longer, healthier lives. However, that doesn’t mean you should be doing shots of it.
As a general rule, you’re better off getting most of your fat from foods like avocados, olives, nuts and seeds than from any cooking oil.
Whole food fats are rich in fiber, phytochemicals, vitamins, and minerals, and are generally less calorie-dense than oils. (But having one to three servings of oils or butter per day is reasonable.)
And if you want personalized advice to suit your body, your eating preferences, and your goals, check out our Nutrition Calculator to figure out how fats fit into your overall diet.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- N.d. Accessed January 14, 2025. https://fdc.nal.usda.gov/fdc-app.html#/food-details/1103679/nutrients.
- N.d. Accessed January 14, 2025. https://fdc.nal.usda.gov/fdc-app.html#/food-details/169998/nutrients.
- Center for Food Safety, and Applied Nutrition. 2024. “Trans Fat.” U.S. Food and Drug Administration. FDA. April 30, 2024. https://www.fda.gov/food/food-additives-petitions/trans-fat.
- Szabo, Zoltan, Tamas Marosvölgyi, Eva Szabo, Viktor Koczka, Zsofia Verzar, Maria Figler, and Tamas Decsi. 2022. Effects of Repeated Heating on Fatty Acid Composition of Plant-Based Cooking Oils. Foods (Basel, Switzerland) 11 (2): 192.
- Ruggiero, Emilia, Augusto Di Castelnuovo, Simona Costanzo, Simona Esposito, Amalia De Curtis, Mariarosaria Persichillo, Chiara Cerletti, et al. 2024. Olive Oil Consumption Is Associated with Lower Cancer, Cardiovascular and All-Cause Mortality among Italian Adults: Prospective Results from the Moli-Sani Study and Analysis of Potential Biological Mechanisms. European Journal of Clinical Nutrition 78 (8): 684–93.
- Ferrara, L. A., A. S. Raimondi, L. d’Episcopo, L. Guida, A. Dello Russo, and T. Marotta. 2000. Olive Oil and Reduced Need for Antihypertensive Medications. Archives of Internal Medicine 160 (6): 837–42.
- Martínez-González, Miguel A., Carmen Sayón-Orea, Vanessa Bullón-Vela, Maira Bes-Rastrollo, Fernando Rodríguez-Artalejo, María José Yusta-Boyo, and Marta García-Solano. 2022. Effect of Olive Oil Consumption on Cardiovascular Disease, Cancer, Type 2 Diabetes, and All-Cause Mortality: A Systematic Review and Meta-Analysis. Clinical Nutrition (Edinburgh, Scotland) 41 (12): 2659–82.
- Tessier, Anne-Julie, Marianna Cortese, Changzheng Yuan, Kjetil Bjornevik, Alberto Ascherio, Daniel D. Wang, Jorge E. Chavarro, et al. 2024. Consumption of Olive Oil and Diet Quality and Risk of Dementia-Related Death. JAMA Network Open 7 (5): e2410021.
- Markellos, Christos, Maria-Eleni Ourailidou, Maria Gavriatopoulou, Panagiotis Halvatsiotis, Theodoros N. Sergentanis, and Theodora Psaltopoulou. 2022. Olive Oil Intake and Cancer Risk: A Systematic Review and Meta-Analysis. PloS One 17 (1): e0261649.
- Teng, Kim-Tiu, Radhika Loganathan, Boon How Chew, and Tsung Fei Khang. 2024. Diverse Impacts of Red Palm Olein, Extra Virgin Coconut Oil and Extra Virgin Olive Oil on Cardiometabolic Risk Markers in Individuals with Central Obesity: A Randomised Trial. European Journal of Nutrition 63 (4): 1225–39.
- De Alzaa, F., C. Guillaume, and L. Ravetti. 2018. Evaluation of Chemical and Physical Changes in Different Commercial Oils during Heating. Acta Scientific Nutritional Health 2 (6): 02–11.
- Hollandbeck, Andy. 2020. “In a Word: The Creation of Canola Oil.” The Saturday Evening Post. November 12, 2020. https://www.saturdayeveningpost.com/2020/11/in-a-word-the-creation-of-canola-oil/.
- Pourrajab, Behnaz, Elham Sharifi-Zahabi, Sepideh Soltani, Hossein Shahinfar, and Farzad Shidfar. 2023. Comparison of Canola Oil and Olive Oil Consumption on the Serum Lipid Profile in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Critical Reviews in Food Science and Nutrition 63 (33): 12270–84.
- Morgan, S. A., A. J. Sinclair, and K. O’Dea. 1993. Effect on Serum Lipids of Addition of Safflower Oil or Olive Oil to Very-Low-Fat Diets Rich in Lean Beef. Journal of the American Dietetic Association 93 (6): 644–48.
- Pourrajab, Behnaz, Elham Sharifi-Zahabi, Sepideh Soltani, Hossein Shahinfar, and Farzad Shidfar. 2023. Comparison of Canola Oil and Olive Oil Consumption on the Serum Lipid Profile in Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Critical Reviews in Food Science and Nutrition 63 (33): 12270–84.
- Shetty, Shilpa S., N. Suchetha Kumari, and Remya Varadarajan. 2023. The Ratio of Omega-6/Omega-3 Fatty Acid: Implications and Application as a Marker to Diabetes. In Biomarkers in Diabetes, 449–67. Cham: Springer International Publishing.
- Guasch-Ferré, Marta, Jun Li, Frank B. Hu, Jordi Salas-Salvadó, and Deirdre K. Tobias. 2018. Effects of Walnut Consumption on Blood Lipids and Other Cardiovascular Risk Factors: An Updated Meta-Analysis and Systematic Review of Controlled Trials. The American Journal of Clinical Nutrition 108 (1): 174–87.
- Yu, Zhi, Vasanti S. Malik, Nana Keum, Frank B. Hu, Edward L. Giovannucci, Meir J. Stampfer, Walter C. Willett, Charles S. Fuchs, and Ying Bao. 2016. Associations between Nut Consumption and Inflammatory Biomarkers. The American Journal of Clinical Nutrition 104 (3): 722–28.
- Marklund, Matti, Jason H. Y. Wu, Fumiaki Imamura, Liana C. Del Gobbo, Amanda Fretts, Janette de Goede, Peilin Shi, et al. 2019. Biomarkers of Dietary Omega-6 Fatty Acids and Incident Cardiovascular Disease and Mortality: An Individual-Level Pooled Analysis of 30 Cohort Studies. Circulation 139 (21): 2422–36.
- Krauss, Ronald M., and Penny M. Kris-Etherton. 2020. Public Health Guidelines Should Recommend Reducing Saturated Fat Consumption as Much as Possible: NO. The American Journal of Clinical Nutrition 112 (1): 19–24.
- Americans, For. n.d. “Cut Down On.” Accessed January 14, 2025. https://odphp.health.gov/sites/default/files/2019-10/DGA_Cut-Down-On-Saturated-Fats.pdf.
- Mozaffarian, Dariush, Renata Micha, and Sarah Wallace. 2010. Effects on Coronary Heart Disease of Increasing Polyunsaturated Fat in Place of Saturated Fat: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS Medicine 7 (3): e1000252.
- Kris-Etherton, Penny M., and Ronald M. Krauss. 2020. Public Health Guidelines Should Recommend Reducing Saturated Fat Consumption as Much as Possible: YES. The American Journal of Clinical Nutrition 112 (1): 13–18.
- Kanon, Alexander P., Sarah J. Spies, Alastair K. H. MacGibbon, and Maher Fuad. 2024. Milk Fat Globule Membrane Is Associated with Lower Blood Lipid Levels in Adults: A Meta-Analysis of Randomized Controlled Trials. Foods (Basel, Switzerland) 13 (17): 2725.
- Pan, Junyu, Meiqing Chen, Ning Li, Rongwei Han, Yongxin Yang, Nan Zheng, Shengguo Zhao, and Yangdong Zhang. 2023. Bioactive Functions of Lipids in the Milk Fat Globule Membrane: A Comprehensive Review. Foods (Basel, Switzerland) 12 (20). https://doi.org/10.3390/foods12203755.
- Rosqvist, Fredrik, Annika Smedman, Helena Lindmark-Månsson, Marie Paulsson, Paul Petrus, Sara Straniero, Mats Rudling, Ingrid Dahlman, and Ulf Risérus. 2015. Potential Role of Milk Fat Globule Membrane in Modulating Plasma Lipoproteins, Gene Expression, and Cholesterol Metabolism in Humans: A Randomized Study. The American Journal of Clinical Nutrition 102 (1): 20–30.
- Choe, Eunok, and David B. Min. 2006. Mechanisms and Factors for Edible Oil Oxidation. Comprehensive Reviews in Food Science and Food Safety 5 (4): 169–86.
- DiNicolantonio, James J., and James H. O’Keefe. 2018. Omega-6 Vegetable Oils as a Driver of Coronary Heart Disease: The Oxidized Linoleic Acid Hypothesis. Open Heart 5 (2): e000898.
- Lane, Melissa M., Elizabeth Gamage, Shutong Du, Deborah N. Ashtree, Amelia J. McGuinness, Sarah Gauci, Phillip Baker, et al. 2024. Ultra-Processed Food Exposure and Adverse Health Outcomes: Umbrella Review of Epidemiological Meta-Analyses. BMJ 384 (February): e077310.
- Pagliai G, Dinu M, Madarena MP, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr. 2021 Feb 14;125;3:308–18.
- Srour B, Fezeu LK, Kesse-Guyot E, Allès B, Méjean C, Andrianasolo RM, et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ. 2019 May 29;365:l1451.
- Mendonça R de D, Lopes ACS, Pimenta AM, Gea A, Martinez-Gonzalez MA, Bes-Rastrollo M. Ultra-Processed Food Consumption and the Incidence of Hypertension in a Mediterranean Cohort: The Seguimiento Universidad de Navarra Project. Am J Hypertens. 2017 Apr 1;30(4):358–66.
- Cordova R, Viallon V, Fontvieille E, Peruchet-Noray L, Jansana A, Wagner KH, et al. Consumption of ultra-processed foods and risk of multimorbidity of cancer and cardiometabolic diseases: a multinational cohort study. Lancet Reg Health Eur. 2023 Dec;35:100771.
- Shramko, Viktoriya S., Yana V. Polonskaya, Elena V. Kashtanova, Ekaterina M. Stakhneva, and Yuliya I. Ragino. 2020. The Short Overview on the Relevance of Fatty Acids for Human Cardiovascular Disorders. Biomolecules 10 (8): 1127.
- Human Foods Program. 2024. “FDA Completes Review of Qualified Health Claim Petition for Oleic Acid and the Risk of Coronary Heart Disease.” U.S. Food and Drug Administration. FDA. September 3, 2024. https://www.fda.gov/food/cfsan-constituent-updates/fda-completes-review-qualified-health-claim-petition-oleic-acid-and-risk-coronary-heart-disease.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)
The post Are seed oils bad for you? Vegetable oil vs. olive oil vs. butter appeared first on Precision Nutrition.
Source: Health1
While our ancestors relied on their senses to assess how they were doing, increasingly, we rely on gadgets.
Today, if you’re curious enough, you can measure your heart rate, your step count, your exercise intensity, and your sleep quality—sometimes all on one sleek device.
In the best cases, these devices offer a bridge between what you subjectively feel and what you can objectively measure.
This is generally a really cool and amazing thing.
Our subjective feelings and assessments matter, but they’re not always the most reliable. Us humans just aren’t particularly skilled at quantifying our experiences and behaviors with cold precision.
Take, for example, a colleague of mine. He believed he was eating within a narrow caloric window, but after careful tracking, he learned that he was putting away a bonus 500 Calories a day—in barbecue sauce.
That said, some of us are better than others.
Ben Johnson, the Canadian sprinter, was reported to have been able to call out his 100 metre time within a tenth of a second of the stopwatch readout.1
That’s outlier performance, to be clear, but it still makes you wonder:
How good are you at assessing yourself?
And, how can you improve your accuracy through the wise use of technology—like fitness trackers—to help you make better decisions about your health?
In the following article, we’ll tackle the above, plus we’ll address:
- How accurate are data trackers in the first place?
- When is tracking helpful? (And when is it not?)
- Can you train yourself to more accurately assess things by feel?
Let’s get into it.
First, how accurate are data trackers anyway?
Not all data is created equal.
Some brands produce better products than others. This is not just hardware but also the quality of their software and datasets.
Beyond that, not all things are equally easy to quantity.
For example, heart rate and step-count data are generally reliable,2 but many other types of outputs—from calories burned to movement velocity—have substantial margins for error.
The below chart shows the reliability of various tracking devices.
(If you’re curious, we cover the accuracy of various progress indicators in more detail here: Are Fitness Trackers Worth It?)
Next, when is tracking actually helpful?
The good: Tracking devices offer us more data about our behaviors and bodies than ever before.
The bad: Tracking devices offer us more data about our behaviors and bodies than ever before.
“What’s really remarkable,” says Samantha Kleinberg, a computer scientist who studies decision-making, “is that even a tiny amount of surplus information has a big negative effect on our decision-making.”3
That’s the paradox of tracking: Too little detail makes it tough to make the right decision, but so does too much. 
This can be expressed as an inverted U, with the sweet spot at the top of the curve.
Today, it’s surprisingly easy to have too much information.
Consider the analysis paralysis you feel after scanning hundreds of reviews from the various taco places in your neighborhood. (All you wanted was a decent el pastor, but now you don’t know which taqueria to pick!)
Finding just enough information to make good decisions is an art form—especially in the world of health and fitness, where it seems like everyone is trying to outdo each other when it comes to providing more science, more customization, and more complexity.
But when all that information starts to blur together with no clear path forward, what should you do?
For starters, you can ask yourself a simple question:
Does tracking increase my wellbeing and performance?
If the answer is a clear yes or no, you know what to do. (Either continue tracking as you were, or drop the gadget and walk away.)
If you’re a little fuzzy, here are three signs to watch for to help you determine if tracking is helpful—or not.
Sign #1: Tracking is decreasing your stress and validating your method(s).
When Zak’s coach raved about the benefits of zone 2 cardio, it sounded logical. But when the rubber on his running shoes hit the road, Zak second-guessed everything. Zak prided himself on his ability to grind, and simply didn’t trust that something that felt easy could also be effective.
Yet, the data didn’t lie. As the weeks went by, Zak watched his resting heart rate drop—along with his recovery time from hard runs. With that reassurance, Zak began to relax about the process—and his resting heart rate dropped further.
Zak hadn’t trusted his feelings, but he did trust the data from his heart rate monitor.
Using a tracking device enabled Zak to calibrate his own perceptions so they were more accurate and realistic.
If you’re a coach who has a client like Zak who’s high performing but doesn’t know it, tracking can help build confidence and reduce the anxiety that they’re “not good enough.”
Here, you empower them by shining a spotlight on existing performance. Expert assurance can go a long way but can also be bolstered by reliable data.
(Recently, many people have begun using continuous glucose monitors, or CGMs, in order to “optimize” their blood sugar levels. This can help “validate” certain food choices… but it can also be a waste of time. Read more: Should people without diabetes use CGMs?)
Bad omen: Tracking is increasing stress or negatively affecting performance.
Sometimes, data can stress you out without any upside—like when you receive poor scores about things beyond your control.
Take the new parent of a newborn who gets a poor sleep quality score.
Tracking has a time and a place. When scores are beyond your control or your priorities lie elsewhere, tracking can create unnecessary stress and is counterproductive.
You can always revisit tracking when circumstances or priorities change.
Sign #2: Clear feedback from data is enhancing your motivation and ability.
For a behaviour to take place, you need three things4:
- Motivation: A compelling reason or desire to take action toward achieving something. This can come from external sources (your spouse is urging you to quit smoking) or internal drives (you’ve always dreamed of running a marathon).
- Ability: You have a combination of skills, plus opportunities to express them. (For example, you know how to do a simple resistance training routine, and you have 20 minutes a day to execute it.) This may involve overcoming constraints like time, money, mental and/or physical effort, social pressures, and changes to routine.5
- Prompt: A prompt is a cue or instruction that elicits an action. (For example, when your GPS tells you to turn left, or when your restless legs “remind” you you’re due for a walk.) Critically, even with high levels of motivation and ability, you may not take action—or the right kind of action—without a prompt.
Fitness trackers shine when you’ve got plenty of motivation and ability—and just lack the prompt.
Take my client, Margaret. She used to have a glass of wine most nights, believing it helped her sleep better. Once she started wearing a sleep tracker though, she saw that her sleep quality was much poorer the nights she imbibed. Once she received this prompt—her sleep score—she adjusted her behavior.
When you highlight important data, the right choices become clearer.
When it comes to changing behaviours, sometimes all it takes is one key piece of data. As they say, “Once you see it, you can’t un-see it.”
(PN’s CEO Tim Jones used the feedback he got from various lifestyle trackers to finally reduce his genetically high cholesterol levels—and built a richer, more meaningful life in the process. Read more: How This Guy Cut His Cholesterol in Half Without Drugs)
Bad omen: Data collection is decreasing motivation or ability.
When Jan, an avid recreational cyclist, found out he could view—then demolish—the records set on local biking trails, he set to work. But as those records were destroyed, so too was his ability to ride for enjoyment. His focus on speed left him under-recovered and eventually led to burnout.
If workouts have become more about the numbers and less about technique, experience, or even enjoyment, tracking is likely no longer helpful.
Sign #3: Tracking is helping you understand yourself better.
The harder you work, the better your results.
Right?
Not necessarily.
This belief tends to get grinders like Zak into trouble because they think they’re making progress—but really they’re just getting in their own way, even inhibiting performance and recovery.
Meanwhile, there are also many people who chronically underestimate their effort and capacity, and would benefit from turning up the heat. Here, data can help us more accurately understand our own potential.
Let’s look at high-intensity interval training (HIIT) as an example. HIIT workouts alternate fixed periods of intense effort with fixed periods of rest. However, these fixed periods of rest are just estimates of recovery times.
Heart rate data can create a more individualized picture of actual recovery needs, which may be faster or slower than you expect.
Sometimes, the mind says yes but the heart says not quite yet.
A good coach does more than just simply ask for more. They also help keep clients out of the unproductive “junk volume” zone, where fatigue accumulates but performance doesn’t improve (and maybe even worsens).
By looking at real-time metrics of output, fatigue, and recovery, you can better understand yourself and your clients, and help keep everyone training and recovering efficiently.
Bad omen: Over-reliance on data is making you lose touch with your own senses.
When you become overly reliant on data, you risk losing touch with your own sense of how you feel, whether that’s hunger and fullness levels, energy and fatigue, or something else.
A relevant example is “The Great My Fitness Pal Blackout.”
In January of 2019, the calorie-tracking app (with a reported 200 million subscribers!) went down for a day. Pretty minor—unless you happened to be tracking your macro and caloric intake and waiting for the app to tell you exactly how much you could eat that day… which I was.
When the app wouldn’t load, I recognized the mild panic I felt was unhelpful. My overreliance on the app had disconnected me from my own internal signals, and without it, I felt adrift. Since then, I’ve shifted my focus to how energetic I feel and one of the oldest tracking technologies available: the mirror.
(If you feel like you’re lost without your besties—your phone and your apps—there’s a name for that. There are also ways to develop a healthier relationship with your tech. Read more: What is nomophobia?)
3 ways to use fitness trackers to help you make more accurate self-assessments
Before we get to how to do the above, let’s talk about why assessing things by feel can be so important.
Whether it’s body fat percentage or movement speed, even supremely motivated and capable clients will experience diminishing objective results from their training.
The scale stops dropping, the number of plates you’re able to load on the bar plateaus, or—gasp—your race time even regresses.
Motivation based purely on progress or other extrinsic goals6 will fall away during these times.
However, exercisers who focus on feelings of mindfulness7, mastery, meaning8, and success9 develop a more resilient practice. They also enjoy the process more, whether that’s the process of running, lifting, winding down for a good night’s sleep, or just enjoying a meal.
So, although objective data can provide essential feedback and guidance, you’ll only reap the full benefits of your practice—that is, enjoyment and results—if you maintain connection with your felt experience.
And good news: You can actually use fitness trackers to calibrate and even improve your ability to accurately sense what’s happening in your body.
Here are three ways to do it.
1. Check in with yourself before you check the data.
Can you imagine asking someone how their vacation was and then waiting for them to look at their photos to be able to answer? That’s what it’s like when you rely purely on external data about your own experience.
Whatever the metric—how far you biked, how many calories you consumed, or how fast your heart was beating—the simplest way to work mindfully with tracker data is to pause, breathe, and then tune into the powerful (if not always accurate) prediction-making powers of your brain.
Once you’ve checked in with yourself, you can calibrate your self-assessment by comparing the detailed (if not always accurate) outputs of your fitness tracker.
Over time, you may be able to narrow the gap between two.
(Note: Don’t forget to regularly update your app. Algorithms and data sets are regularly adjusted for better predictive accuracy.)
2. Develop mental shortcuts that can occasionally stand in for objective measures.
The coaches I work with regularly ask people to estimate the boundaries of their strength (such as how many reps they can do at a given weight until failure).
Novices are often terrible at estimating this—and regularly off the mark by five or more reps. However, the use of objective trackers can help calibrate their understanding, and most people can reduce their margin of error dramatically.
In theory, you might use fancy tools like accelerometers or blood lactate measurements, but our coaches just ask, “For a million dollars a rep, how many more reps do you think you could do?”
Though there’s nothing objective about this question, most clients are able to use the prompt as a kind of shortcut to understand maximal effort. (After all, that last rep may be worth seven figures!)
The question also leverages the rate of perceived exertion (RPE)—your perception of how hard you’re working—which is one of the most validated sensory-driven approaches.
Not everyone is automatically good at estimating RPE, but most people can improve their skills by mapping their felt experience with occasional calibration with objective data.
3. Keep developing your ability to dial into your senses.
Trackers have components like accelerometers, GPS, and gyroscopes to sense data about speed, distance, and more.
But humans are no slouches either.
We have…
- Mechanoreceptors that respond to pressure, vibration, and the joint angles change
- A vestibular system that monitors balance and angle changes
- Proprioceptors that clock the speed and rate of length-change of muscle spindles
- Thermoreceptors that register register warming or cooling
- Chemoreceptors that detect chemical changes, such as scent or taste, as well as changes in the bloodstream
- Nociceptors—part of the body’s alarm system—that sense threat and send signals of potential harm or distress
And that’s only a partial list.
You have access to an incredibly rich network of sensory information—something that technology cannot begin to touch.
All of this information is fed into the powerful pattern-recognition machine of your nervous system.
To continue honing your ability to use this rich network of sensory information, regularly check in with what and how you’re feeling.
When you learn to calibrate your own senses with objective data, you can leverage all the cool advances in wearable tech—while still keeping your own experience front and centre.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- Francis C. Speed Trap: Inside the Biggest Scandal in Olympic History. Toronto: Stoddart Publishing Co. Ltd.; 1990.
- Stat News. Fitbit’s accuracy has a dark-skin problem. Stat News [Internet]. 2019 Jul 24 [cited 2024 Nov 23]. Available from: https://web.archive.org/web/20240129224809/https://www.statnews.com/2019/07/24/fitbit-accuracy-dark-skin/
- Stevens Institute of Technology. Want to make better decisions? Ask for less information, not more. Stevens Institute of Technology [Internet]. 2023 [cited 2024 Nov 23]. Available from: https://www.stevens.edu/news/want-to-make-better-decisions-ask-for-less-information-not-more
- Fogg B. Behavior Model. BehaviorModel.org [Internet]. 2024 [cited 2024 Nov 23]. Available from: https://behaviormodel.org/
- Fogg, B. J. 2019. Tiny Habits: Small Changes Change Everything. New York; Houghton Mifflin Harcourt.
- Bradshaw, Emma L., James H. Conigrave, Ben A. Steward, Kelly A. Ferber, Philip D. Parker, and Richard M. Ryan. 2023. A Meta-Analysis of the Dark Side of the American Dream: Evidence for the Universal Wellness Costs of Prioritizing Extrinsic over Intrinsic Goals. Journal of Personality and Social Psychology 124 (4): 873–99.
- Hagan, John E., Jr, Dietmar Pollmann, and Thomas Schack. 2017. Elite Athletes’ in-Event Competitive Anxiety Responses and Psychological Skills Usage under Differing Conditions. Frontiers in Psychology 8 (December). https://doi.org/10.3389/fpsyg.2017.02280.
- University of Rochester Medical Center. Self-Determination Theory [Internet]. Rochester (NY): University of Rochester Medical Center; [cited 2024 Nov 25]. Available from: https://www.urmc.rochester.edu/community-health/patient-care/self-determination-theory.aspx
- Teixeira DS, Bastos V, Andrade AJ, Palmeira AL, Ekkekakis P. Individualized pleasure-oriented exercise sessions, exercise frequency, and affective outcomes: a pragmatic randomized controlled trial. Int J Behav Nutr Phys Act. 2024;21(1):1636.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)
The post How to use fitness trackers to enhance performance and wellbeing—without losing touch with yourself appeared first on Precision Nutrition.
Source: Health1
While our ancestors relied on their senses to assess how they were doing, increasingly, we rely on gadgets.
Today, if you’re curious enough, you can measure your heart rate, your step count, your exercise intensity, and your sleep quality—sometimes all on one sleek device.
In the best cases, these devices offer a bridge between what you subjectively feel and what you can objectively measure.
This is generally a really cool and amazing thing.
Our subjective feelings and assessments matter, but they’re not always the most reliable. Us humans just aren’t particularly skilled at quantifying our experiences and behaviors with cold precision.
Take, for example, a colleague of mine. He believed he was eating within a narrow caloric window, but after careful tracking, he learned that he was putting away a bonus 500 Calories a day—in barbecue sauce.
That said, some of us are better than others.
Ben Johnson, the Canadian sprinter, was reported to have been able to call out his 100 metre time within a tenth of a second of the stopwatch readout.1
That’s outlier performance, to be clear, but it still makes you wonder:
How good are you at assessing yourself?
And, how can you improve your accuracy through the wise use of technology—like fitness trackers—to help you make better decisions about your health?
In the following article, we’ll tackle the above, plus we’ll address:
- How accurate are data trackers in the first place?
- When is tracking helpful? (And when is it not?)
- Can you train yourself to more accurately assess things by feel?
Let’s get into it.
First, how accurate are data trackers anyway?
Not all data is created equal.
Some brands produce better products than others. This is not just hardware but also the quality of their software and datasets.
Beyond that, not all things are equally easy to quantity.
For example, heart rate and step-count data are generally reliable,2 but many other types of outputs—from calories burned to movement velocity—have substantial margins for error.
The below chart shows the reliability of various tracking devices.
(If you’re curious, we cover the accuracy of various progress indicators in more detail here: Are Fitness Trackers Worth It?)
Next, when is tracking actually helpful?
The good: Tracking devices offer us more data about our behaviors and bodies than ever before.
The bad: Tracking devices offer us more data about our behaviors and bodies than ever before.
“What’s really remarkable,” says Samantha Kleinberg, a computer scientist who studies decision-making, “is that even a tiny amount of surplus information has a big negative effect on our decision-making.”3
That’s the paradox of tracking: Too little detail makes it tough to make the right decision, but so does too much. 
This can be expressed as an inverted U, with the sweet spot at the top of the curve.
Today, it’s surprisingly easy to have too much information.
Consider the analysis paralysis you feel after scanning hundreds of reviews from the various taco places in your neighborhood. (All you wanted was a decent el pastor, but now you don’t know which taqueria to pick!)
Finding just enough information to make good decisions is an art form—especially in the world of health and fitness, where it seems like everyone is trying to outdo each other when it comes to providing more science, more customization, and more complexity.
But when all that information starts to blur together with no clear path forward, what should you do?
For starters, you can ask yourself a simple question:
Does tracking increase my wellbeing and performance?
If the answer is a clear yes or no, you know what to do. (Either continue tracking as you were, or drop the gadget and walk away.)
If you’re a little fuzzy, here are three signs to watch for to help you determine if tracking is helpful—or not.
Sign #1: Tracking is decreasing your stress and validating your method(s).
When Zak’s coach raved about the benefits of zone 2 cardio, it sounded logical. But when the rubber on his running shoes hit the road, Zak second-guessed everything. Zak prided himself on his ability to grind, and simply didn’t trust that something that felt easy could also be effective.
Yet, the data didn’t lie. As the weeks went by, Zak watched his resting heart rate drop—along with his recovery time from hard runs. With that reassurance, Zak began to relax about the process—and his resting heart rate dropped further.
Zak hadn’t trusted his feelings, but he did trust the data from his heart rate monitor.
Using a tracking device enabled Zak to calibrate his own perceptions so they were more accurate and realistic.
If you’re a coach who has a client like Zak who’s high performing but doesn’t know it, tracking can help build confidence and reduce the anxiety that they’re “not good enough.”
Here, you empower them by shining a spotlight on existing performance. Expert assurance can go a long way but can also be bolstered by reliable data.
(Recently, many people have begun using continuous glucose monitors, or CGMs, in order to “optimize” their blood sugar levels. This can help “validate” certain food choices… but it can also be a waste of time. Read more: Should people without diabetes use CGMs?)
Bad omen: Tracking is increasing stress or negatively affecting performance.
Sometimes, data can stress you out without any upside—like when you receive poor scores about things beyond your control.
Take the new parent of a newborn who gets a poor sleep quality score.
Tracking has a time and a place. When scores are beyond your control or your priorities lie elsewhere, tracking can create unnecessary stress and is counterproductive.
You can always revisit tracking when circumstances or priorities change.
Sign #2: Clear feedback from data is enhancing your motivation and ability.
For a behaviour to take place, you need three things4:
- Motivation: A compelling reason or desire to take action toward achieving something. This can come from external sources (your spouse is urging you to quit smoking) or internal drives (you’ve always dreamed of running a marathon).
- Ability: You have a combination of skills, plus opportunities to express them. (For example, you know how to do a simple resistance training routine, and you have 20 minutes a day to execute it.) This may involve overcoming constraints like time, money, mental and/or physical effort, social pressures, and changes to routine.5
- Prompt: A prompt is a cue or instruction that elicits an action. (For example, when your GPS tells you to turn left, or when your restless legs “remind” you you’re due for a walk.) Critically, even with high levels of motivation and ability, you may not take action—or the right kind of action—without a prompt.
Fitness trackers shine when you’ve got plenty of motivation and ability—and just lack the prompt.
Take my client, Margaret. She used to have a glass of wine most nights, believing it helped her sleep better. Once she started wearing a sleep tracker though, she saw that her sleep quality was much poorer the nights she imbibed. Once she received this prompt—her sleep score—she adjusted her behavior.
When you highlight important data, the right choices become clearer.
When it comes to changing behaviours, sometimes all it takes is one key piece of data. As they say, “Once you see it, you can’t un-see it.”
(PN’s CEO Tim Jones used the feedback he got from various lifestyle trackers to finally reduce his genetically high cholesterol levels—and built a richer, more meaningful life in the process. Read more: How This Guy Cut His Cholesterol in Half Without Drugs)
Bad omen: Data collection is decreasing motivation or ability.
When Jan, an avid recreational cyclist, found out he could view—then demolish—the records set on local biking trails, he set to work. But as those records were destroyed, so too was his ability to ride for enjoyment. His focus on speed left him under-recovered and eventually led to burnout.
If workouts have become more about the numbers and less about technique, experience, or even enjoyment, tracking is likely no longer helpful.
Sign #3: Tracking is helping you understand yourself better.
The harder you work, the better your results.
Right?
Not necessarily.
This belief tends to get grinders like Zak into trouble because they think they’re making progress—but really they’re just getting in their own way, even inhibiting performance and recovery.
Meanwhile, there are also many people who chronically underestimate their effort and capacity, and would benefit from turning up the heat. Here, data can help us more accurately understand our own potential.
Let’s look at high-intensity interval training (HIIT) as an example. HIIT workouts alternate fixed periods of intense effort with fixed periods of rest. However, these fixed periods of rest are just estimates of recovery times.
Heart rate data can create a more individualized picture of actual recovery needs, which may be faster or slower than you expect.
Sometimes, the mind says yes but the heart says not quite yet.
A good coach does more than just simply ask for more. They also help keep clients out of the unproductive “junk volume” zone, where fatigue accumulates but performance doesn’t improve (and maybe even worsens).
By looking at real-time metrics of output, fatigue, and recovery, you can better understand yourself and your clients, and help keep everyone training and recovering efficiently.
Bad omen: Over-reliance on data is making you lose touch with your own senses.
When you become overly reliant on data, you risk losing touch with your own sense of how you feel, whether that’s hunger and fullness levels, energy and fatigue, or something else.
A relevant example is “The Great My Fitness Pal Blackout.”
In January of 2019, the calorie-tracking app (with a reported 200 million subscribers!) went down for a day. Pretty minor—unless you happened to be tracking your macro and caloric intake and waiting for the app to tell you exactly how much you could eat that day… which I was.
When the app wouldn’t load, I recognized the mild panic I felt was unhelpful. My overreliance on the app had disconnected me from my own internal signals, and without it, I felt adrift. Since then, I’ve shifted my focus to how energetic I feel and one of the oldest tracking technologies available: the mirror.
(If you feel like you’re lost without your besties—your phone and your apps—there’s a name for that. There are also ways to develop a healthier relationship with your tech. Read more: What is nomophobia?)
3 ways to use fitness trackers to help you make more accurate self-assessments
Before we get to how to do the above, let’s talk about why assessing things by feel can be so important.
Whether it’s body fat percentage or movement speed, even supremely motivated and capable clients will experience diminishing objective results from their training.
The scale stops dropping, the number of plates you’re able to load on the bar plateaus, or—gasp—your race time even regresses.
Motivation based purely on progress or other extrinsic goals6 will fall away during these times.
However, exercisers who focus on feelings of mindfulness7, mastery, meaning8, and success9 develop a more resilient practice. They also enjoy the process more, whether that’s the process of running, lifting, winding down for a good night’s sleep, or just enjoying a meal.
So, although objective data can provide essential feedback and guidance, you’ll only reap the full benefits of your practice—that is, enjoyment and results—if you maintain connection with your felt experience.
And good news: You can actually use fitness trackers to calibrate and even improve your ability to accurately sense what’s happening in your body.
Here are three ways to do it.
1. Check in with yourself before you check the data.
Can you imagine asking someone how their vacation was and then waiting for them to look at their photos to be able to answer? That’s what it’s like when you rely purely on external data about your own experience.
Whatever the metric—how far you biked, how many calories you consumed, or how fast your heart was beating—the simplest way to work mindfully with tracker data is to pause, breathe, and then tune into the powerful (if not always accurate) prediction-making powers of your brain.
Once you’ve checked in with yourself, you can calibrate your self-assessment by comparing the detailed (if not always accurate) outputs of your fitness tracker.
Over time, you may be able to narrow the gap between two.
(Note: Don’t forget to regularly update your app. Algorithms and data sets are regularly adjusted for better predictive accuracy.)
2. Develop mental shortcuts that can occasionally stand in for objective measures.
The coaches I work with regularly ask people to estimate the boundaries of their strength (such as how many reps they can do at a given weight until failure).
Novices are often terrible at estimating this—and regularly off the mark by five or more reps. However, the use of objective trackers can help calibrate their understanding, and most people can reduce their margin of error dramatically.
In theory, you might use fancy tools like accelerometers or blood lactate measurements, but our coaches just ask, “For a million dollars a rep, how many more reps do you think you could do?”
Though there’s nothing objective about this question, most clients are able to use the prompt as a kind of shortcut to understand maximal effort. (After all, that last rep may be worth seven figures!)
The question also leverages the rate of perceived exertion (RPE)—your perception of how hard you’re working—which is one of the most validated sensory-driven approaches.
Not everyone is automatically good at estimating RPE, but most people can improve their skills by mapping their felt experience with occasional calibration with objective data.
3. Keep developing your ability to dial into your senses.
Trackers have components like accelerometers, GPS, and gyroscopes to sense data about speed, distance, and more.
But humans are no slouches either.
We have…
- Mechanoreceptors that respond to pressure, vibration, and the joint angles change
- A vestibular system that monitors balance and angle changes
- Proprioceptors that clock the speed and rate of length-change of muscle spindles
- Thermoreceptors that register register warming or cooling
- Chemoreceptors that detect chemical changes, such as scent or taste, as well as changes in the bloodstream
- Nociceptors—part of the body’s alarm system—that sense threat and send signals of potential harm or distress
And that’s only a partial list.
You have access to an incredibly rich network of sensory information—something that technology cannot begin to touch.
All of this information is fed into the powerful pattern-recognition machine of your nervous system.
To continue honing your ability to use this rich network of sensory information, regularly check in with what and how you’re feeling.
When you learn to calibrate your own senses with objective data, you can leverage all the cool advances in wearable tech—while still keeping your own experience front and centre.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- Francis C. Speed Trap: Inside the Biggest Scandal in Olympic History. Toronto: Stoddart Publishing Co. Ltd.; 1990.
- Stat News. Fitbit’s accuracy has a dark-skin problem. Stat News [Internet]. 2019 Jul 24 [cited 2024 Nov 23]. Available from: https://web.archive.org/web/20240129224809/https://www.statnews.com/2019/07/24/fitbit-accuracy-dark-skin/
- Stevens Institute of Technology. Want to make better decisions? Ask for less information, not more. Stevens Institute of Technology [Internet]. 2023 [cited 2024 Nov 23]. Available from: https://www.stevens.edu/news/want-to-make-better-decisions-ask-for-less-information-not-more
- Fogg B. Behavior Model. BehaviorModel.org [Internet]. 2024 [cited 2024 Nov 23]. Available from: https://behaviormodel.org/
- Fogg, B. J. 2019. Tiny Habits: Small Changes Change Everything. New York; Houghton Mifflin Harcourt.
- Bradshaw, Emma L., James H. Conigrave, Ben A. Steward, Kelly A. Ferber, Philip D. Parker, and Richard M. Ryan. 2023. A Meta-Analysis of the Dark Side of the American Dream: Evidence for the Universal Wellness Costs of Prioritizing Extrinsic over Intrinsic Goals. Journal of Personality and Social Psychology 124 (4): 873–99.
- Hagan, John E., Jr, Dietmar Pollmann, and Thomas Schack. 2017. Elite Athletes’ in-Event Competitive Anxiety Responses and Psychological Skills Usage under Differing Conditions. Frontiers in Psychology 8 (December). https://doi.org/10.3389/fpsyg.2017.02280.
- University of Rochester Medical Center. Self-Determination Theory [Internet]. Rochester (NY): University of Rochester Medical Center; [cited 2024 Nov 25]. Available from: https://www.urmc.rochester.edu/community-health/patient-care/self-determination-theory.aspx
- Teixeira DS, Bastos V, Andrade AJ, Palmeira AL, Ekkekakis P. Individualized pleasure-oriented exercise sessions, exercise frequency, and affective outcomes: a pragmatic randomized controlled trial. Int J Behav Nutr Phys Act. 2024;21(1):1636.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification. (You can enroll now at a big discount.)
The post Private: How to use fitness trackers to enhance performance and wellbeing—without losing touch with yourself appeared first on Precision Nutrition.
Source: Health1
“I worried that if I stopped tracking macros, I would lose my physique.”
After years of careful macro tracking, Dr. Fundaro finally admitted to herself that the method no longer worked for her. Yet she was afraid to give it up.
If anyone should feel confident in their food choices, it would be Dr. Gabrielle Fundaro. After all, Dr. Fundaro has a PhD in Human Nutrition, a decade-plus of nutrition coaching experience, and six powerlifting competitions under her belt.
Yet, when she was really honest with herself, Dr. Fundaro realized that she felt far from confident around food. For years, she’d used macro counting as a way to stay “on track” with her eating.
And it worked… until it didn’t.
After years of macro tracking, Dr. Fundaro was tired of the whole thing. She was tired of making sure her macros were perfectly in balance. She was sick of not being able to just pick whatever she wanted off a menu and enjoy the meal, trusting that her health and physique wouldn’t go sideways as a result.
Yet the idea of not tracking freaked her out. Every time she quit tracking, she worried:
“What if I don’t eat enough protein, and lose all my muscle?”
“What if I overeat and gain fat?”
“What if I have no idea how to fuel myself without tracking macros? And what does that say about me as an expert in the field of nutrition?”
The more Dr. Fundaro wrestled with macro tracking, the more she wanted to find an alternative.
Something that would support her nutritional goals while also giving her a sense of freedom and peace around food.
Calorie counting wouldn’t do it. That was just as restrictive as counting macros—maybe more.
Intuitive eating didn’t seem like a good fit either. Intuitive eating relies heavily on a person’s ability to tune into internal hunger and fullness cues to guide food choices and amounts. After years of relying on external cues (like her macro targets), Dr. Fundaro didn’t feel trusting enough of her own instincts; she wanted more structure.
Meanwhile, at the gym, Dr. Fundaro began lifting based on the Rate of Perceived Exertion (RPE) scale—a framework that helps individuals quantify the amount of effort they’re putting into a given movement or activity. It’s considered a valuable tool to help people train safely and effectively according to their ability and goals. (More on that soon.)
While using the RPE scale in her training, Dr. Fundaro found she was both getting stronger and recovering better. There was something to this combination of structure and intuition that just worked.
And then, it dawned on Dr. Fundaro like the apple hit Sir Isaac Newton on the head:
If Rate of Perceived Exertion could help her train better, couldn’t a similar framework help her eat better?
With that, the RPE-Eating Scale was born.
Dr. Fundaro has since used this alternative method to help herself and her clients regain confidence and self-trust around food; improve nutritional awareness and competence; and free themselves from food tracking.
(Yup, Dr. Fundaro finally trusts her eating choices—no macro tracker in sight.)
In this article, you’ll learn how she did it, plus:
- What the RPE-Eating scale is
- How to practice RPE-Eating
- How to use RPE-Eating for weight loss or gain
- Whether RPE-Eating is right for you or your clients
- What to keep in mind if you’re skeptical of the concept
What is RPE-Eating?
Invented by Gunnar Borg in the 1960’s, Rate of Perceived Exertion (RPE) is a scale that’s used to measure an individual’s perceived level of effort or exertion during exercise.
Though Borg’s RPE uses a scale that goes from 6 to 20, many modern scales use a 0 to 10 range (which is the range that Dr. Fundaro adapted for her RPE-Eating scale).
Here’s the RPE scale used in fitness.
| Rating | Perceived Exertion Level |
|---|---|
| 0 | No exertion, at rest |
| 1 | Very light |
| 2-3 | Light |
| 4-5 | Moderate, somewhat hard |
| 6-7 | High, vigorous |
| 8-9 | Very hard |
| 10 | Maximum effort, highest possible |
Originally used in physiotherapy settings, the scale is now frequently used in fitness training.
For example, powerlifters might use it to choose how heavy they want to go during a training session. Or, pregnant women might use it to ensure they aren’t over-exerting themselves during a fitness class or strength training session.
Because human experience is highly subjective and individual, the scale allows the exerciser to judge how hard they’re working for themselves. A coach can provide a general guideline, such as “aim for a 7/10 this set,” but it’s up to the client to determine exactly what that means for them.
Dr. Fundaro had used the scale many times with herself, and clients. She always appreciated the sense of autonomy it gave her clients, while still providing some structure.
So, she decided to take the same 1-10 scale and its principles, and apply it to eating.
Here’s what the RPE-Eating Scale looks like:

The goal with RPE-Eating is similar to RPE when training: Develop the skills to determine what is sufficient for you, without having to rely on other external metrics (such as apps or trackers).
How to practice RPE-Eating
If you’ve ever practiced RPE-training, you’ll know it takes some time to get used to. RPE-Eating is the same.
Don’t expect to be in lockstep with all of your body’s internal cues at first, especially if you’ve been ignoring them for a long time.
With this in mind, apply the steps below to practice the RPE-Eating process.
Step #1: Get clear on your goals.
RPE-Eating is not just another diet.
“It’s not about aiming to change your body,” Dr. Fundaro explains. “It’s not about feeling more control over your diet. Nor is it about feeling like you’re eating the ‘optimal’ diet.”
If your priority is maintaining a specific physique (such as staying ultra lean) or changing your body (building muscle or losing fat), this method can be adapted for that, though it isn’t the most efficient one to use.
Instead, RPE-Eating is about sensing into what your body needs and giving yourself appropriate nourishment—while building inner trust and confidence along the way.
“You have to trust that you’ll be able to nourish your body, and that you’ll be okay even though things may change in your body,” says Dr. Fundaro.
Admittedly, this can be challenging to do. It can also be difficult to let go of the expectation that you’ll hit the “right” macros at every meal—which RPE-Eating isn’t specifically designed to do.
However, if your goal is to build more self-trust, RPE-Eating can be a great tool to help you do that.
Step #2: Practice identifying your hunger cues
Before we explore this step, let’s distinguish between two motivators for eating.
First, there’s hunger. Hunger occurs when physical cues in your body (like a general sense of emptiness or rumbling in your stomach, or lightheadedness) tells you that you require energy—known to us mortals as food.
Then, there’s appetite. Appetite is our desire or interest in eating. It can stay peaked even after hunger is quelled, especially if something looks or tastes especially delicious—like a warm, gooey cookie offered after dinner that you feel you have to try, even though you’re technically full.
While it’s normal to eat for both hunger and appetite drives, the two can become mixed up. Especially if we have a history of dieting and tracking food.
The RPE-Eating scale helps you tap back into those true physical hunger cues, and learn the difference between hunger and appetite.
To put this in practice, try this before your next meal:
 Using the RPE-Eating scale mentioned above, identify your current level of hunger. Record the number on paper or the notes app on your phone.
Using the RPE-Eating scale mentioned above, identify your current level of hunger. Record the number on paper or the notes app on your phone.
 Then, eat your meal with as much presence as possible. (Note: This in itself takes practice. It can help to limit distractions, such as eating at the table rather than in front of the TV, and focusing on the flavors and textures of the food you’re eating, and how you feel eating it.)
Then, eat your meal with as much presence as possible. (Note: This in itself takes practice. It can help to limit distractions, such as eating at the table rather than in front of the TV, and focusing on the flavors and textures of the food you’re eating, and how you feel eating it.)
 About halfway through the meal, check in again. Based on the scale, how hungry are you now? As before, record the number.
About halfway through the meal, check in again. Based on the scale, how hungry are you now? As before, record the number.
 If you’re still hungry, finish your meal. When you’re finished, repeat the same process, writing down where you are on the scale.
If you’re still hungry, finish your meal. When you’re finished, repeat the same process, writing down where you are on the scale.
 Once you’re done, take a minute and tune into what your body feels like. What does it feel like to be full? “Download” that feeling into your mind and internalize it in your body, as if you’re updating your phone with the latest software.
Once you’re done, take a minute and tune into what your body feels like. What does it feel like to be full? “Download” that feeling into your mind and internalize it in your body, as if you’re updating your phone with the latest software.
Repeat this for as many meals as you can. Aim to do it for one meal a day for a week or so, or for as long as feels good to you. Don’t worry if you forget: simply repeat the practice when you can.
The more you practice this, the better you’ll become at being attuned with your actual hunger cues. With time, you’ll likely find you develop more trust in your internal compass than what the latest diet tracker says for your needs.
(For more on fully-tuned-in, mindful eating, read: The benefits of slow eating.)
Step #3: Get to know your non-hunger triggers
Have you ever come home after a super stressful day and you’ve basically thrown yourself onto a bag of chips or a carton of ice cream?
We might like to imagine ourselves eating every meal mindfully, using the RPE- Eating system to a tee, but life rarely works like that.
Chances are, there are certain situations that trigger you to eat more quickly, mindlessly, and beyond the point of hunger.
That’s okay.
Dr. Fundaro’s suggestion? Aim to become more aware of the situations that cause you to overeat in the first place.
To do this, you can practice something we use in PN Coaching: Notice and name.
When you find yourself scarfing down food faster than you can blink, simply try to notice what’s going on.
Can you name a feeling—such as anxiety, or sadness?
Can you identify a situation or moment that happened before you started eating—say, an argument with your teenager, or a nasty email from your boss?
Once you’ve identified the feeling, event, or person that’s triggered you to eat compulsively, see if you can also identify what you might really be needing or desiring.
Eating for comfort is normal. However, if it’s the only coping method we have, it can cause more problems than it solves in the long run.
When you find yourself with an urge to eat mindlessly, consider what non-food coping mechanisms might help you feel better. That could be 10 minutes away from your computer to close your eyes and breathe, a walk outside, or a quick call to a friend to rant—or just talk about something completely unrelated.
Getting to know your non-hunger eating triggers—plus widening your repertoire of self-soothing methods—is just as valuable as getting to know your hunger cues. Over time, this awareness will allow you to eat with more intention.
Step #4: Eat for satiety AND satisfaction
Even when you’re “adequately fueled” from a physical perspective, you might still feel unsatisfied from an emotional perspective.
That’s because, according to the RPE-Eating framework, eating should fulfill two criteria:
 Satiety describes the physical sensation of being full; your calorie or fuel needs are met.
Satiety describes the physical sensation of being full; your calorie or fuel needs are met.
 Satisfaction describes a more holistic feeling of being nourished; your calorie needs are met, but your meal also felt pleasurable.
Satisfaction describes a more holistic feeling of being nourished; your calorie needs are met, but your meal also felt pleasurable.
If you ate to satiety only, your calorie needs might be met and your physical hunger quelled, but you might still feel unsatisfied—maybe because chocolate is on your “don’t” list, and even though you’ve eaten everything else in your kitchen that isn’t chocolate, nothing quite “hit the spot.”
In other words, you can eat to satiety at every meal, yet still be “restricting” foods.
You may not be restricting calories per se, but you may have banned entire food groups—baked goods, pizza, or whatever else curls your toes. This can lead to a feeling of constantly needing to police yourself, and doesn’t leave much room for the flexibility and spontaneity that real-life (enjoyable) eating requires.
(Plus, avoiding particular foods tends to work like a pendulum: restrict now; binge later. If you want to learn how to stop those wild swings, read: How to eat junk food: A guide for conflicted humans)
Satisfaction is a key part of eating.
After all, humans don’t just eat for adequate nutrients and energy. We eat for other reasons too: pleasure, novelty, tradition, community, enjoyment.
So, to take your RPE-Eating to the next level, Dr. Fundaro recommends trying it with meals and foods you genuinely enjoy.
If any foods or meals have been “off-limits,” try eating them using the RPE technique. (Macaroni and cheese, anyone?)
Practice using the scale with a variety of meals (including those you may have restricted previously), and notice how you feel over time.
With experience, you’ll get to know what it feels like to adequately fuel yourself with a variety of foods—including those you genuinely enjoy.
How do I know if RPE-Eating is right for me or my clients?
RPE-Eating isn’t for everyone, but might be a good fit for you (or your clients) if:
 You feel dependent on food tracking, but you don’t want to be.
You feel dependent on food tracking, but you don’t want to be.
 Every time you stop tracking, the loss of perceived control freaks you out and drives you right back to tracking.
Every time you stop tracking, the loss of perceived control freaks you out and drives you right back to tracking.
 You want to stop tracking, but you want to have some type of system or guidance in place.
You want to stop tracking, but you want to have some type of system or guidance in place.
 You’re currently tracking (or considering tracking) your food intake, and you have elevated risk factors for developing an eating disorder such as high body dissatisfaction; a history of yo-yo dieting; a history of disordered eating patterns; and/or participation in weight class sports.
You’re currently tracking (or considering tracking) your food intake, and you have elevated risk factors for developing an eating disorder such as high body dissatisfaction; a history of yo-yo dieting; a history of disordered eating patterns; and/or participation in weight class sports.
If you’re a coach looking to use this tool with a client, check out Dr. Fundaro’s resources. Remember this tool may not be for everyone, and how you apply it needs to be flexible.
Note: If you or your client struggles with disordered eating, this tool does not replace working with a health professional who specializes in eating disorders, such as a therapist, doctor, or registered dietician.
How to use RPE- Eating for weight loss or weight gain
According to Dr. Fundaro, the best way to use RPE-Eating is in a weight-neutral setting.
While it could be used for weight modification, she doesn’t recommend treating it as another way to hit your macros or “goal weight.”
“I’m not anti-weight modification,” Dr. Fundaro explains. “I’m pro safe weight modification. I compare weight loss to contact sports. There are inherent risks but they can be mitigated through best practices.”
Dr. Fundaro elaborates: “Since RPE-Eating removes macro-tracking, which can increase risk of disordered eating in some people, and relies on biofeedback and non-hunger triggers, RPE-Eating provides a safety net that macro-tracking alone doesn’t provide.”
But if you do want to use RPE-Eating for intentional weight change, what should you do?
Dr. Fundaro recommends aiming to hover around the ranges that support your goal.
(As a reminder, a 1 to 3 on the RPE-Eating scale is categorized as “inadequate fuel; a 4 to 7 is categorized as “adequate fuel”; and a 8 to 10 is categorized as “excess fuel.”)
 If the goal is weight gain, you’ll likely aim to eat within the 7 to 8 range for most of your meals.
If the goal is weight gain, you’ll likely aim to eat within the 7 to 8 range for most of your meals.
 If the goal is weight loss, you’ll likely aim to eat within the 4 to 5 range for most of your meals.
If the goal is weight loss, you’ll likely aim to eat within the 4 to 5 range for most of your meals.
A key thing to remember is that you would never use RPE-Eating for extreme weight-modification such as for a bodybuilding competition. “That would be like using physio exercises to prepare for a powerlifting competition.” In other words, it’s not the right tool for the job.
Hold up, bro: Isn’t this just feelings over facts?
If you’re skeptical and think this is just eating “based on your feelings,” keep in mind that RPE was once laughed at by lifters, too.
These days, RPE and autoregulation are widely accepted in gym culture and have been studied as a valid method for managing and guiding your training. 1
RPE isn’t perfect, but it’s pretty accurate and incredibly convenient. A lot more convenient than, say, using a velocity loss tracker for every set. 2 3
And while it might seem like it’s all feelings-based, the RPE scale is actually built around practicing the skill of interoceptive awareness—the awareness of internal sensations in your body.
The better you get at the skill of interoceptive awareness, the more you’ll be able to use that awareness to make informed decisions about your training.
RPE-Eating is similar: It builds the skill of sensing into your own body, and lets your internal sensations guide your decisions.
Similar to how the bar slowing down on a squat would indicate you’re getting closer to failure, experiencing the absence of hunger at the end of your meal would indicate you’re closer to being full.
Instead of tracking your glucose levels to validate your perceived hunger, you use internal cues that correlate with lowered blood sugar and coincide with hunger.
And, let’s be real: Being mindful of stomach grumbling or general hunger pangs is much more convenient and accessible than tracking glucose readings.
This process will not be perfect. You may undereat or overeat at first. But over time, with practice, you’ll build the core skills of RPE-Eating.
Are there downsides to RPE-Eating?
While this tool can be helpful, it’s just a tool. A screwdriver is great, but it isn’t useful when you need a hammer.
RPE-Eating can be great for helping you become more aware of your internal hunger cues and build a better relationship with food along the way.
It can also be more laborious. It requires paying real attention to your feelings (physical and emotional), and reflecting on them.
This can be difficult for anyone—but especially people who aren’t able to sit at the table and have a leisurely meal, like parents with small kids, or people with work schedules that require eating on-the-go.
If this is you, just use RPE-Eating when it does work for you—or simply pick and choose specific steps to use in isolation. For example, maybe you try RPE-Eating on the occasional quiet lunch break. Or, maybe you focus solely on developing your awareness of hunger and fullness cues, without trying to change anything else.
If you’ve been tracking macros for a long time, it can be hard to stop.
Tracking macros isn’t inherently bad. It can actually be a helpful tool to teach you more about nutrition. But it’s also not something most people want to do for the rest of their lives.
The problem is, if you’ve depended on tracking your food intake, stopping can feel scary.
In these cases, RPE-Eating can be used as a kind of off-ramp to help transition away from rigid and restrictive macro tracking.
(It can also help loosen the compulsion to “always finish your plate.” Though macros tracking and habitual plate-cleaning may sound different, they’re actually similar: both rely on external cues—such as macro targets or what’s served on your plate—to determine when you’re “done.”)
RPE-Eating won’t take away all the scary feelings that may come with changing ingrained ways of eating.
However, it can provide some structure and language to help you, or your clients, eat with less fear, less stress, and a bit more confidence.
“The goal,” says Dr. Fundaro, “is to know that you’re nourishing yourself—and you don’t need a food tracker to do that.”
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Helms, Eric R., Kedric Kwan, Colby A. Sousa, John B. Cronin, Adam G. Storey, and Michael C. Zourdos. 2020. Methods for Regulating and Monitoring Resistance Training. Journal of Human Kinetics 74 (1): 23–42.
2. Hackett, Daniel A., Nathan A. Johnson, Mark Halaki, and Chin-Moi Chow. 2012. A Novel Scale to Assess Resistance-Exercise Effort. Journal of Sports Sciences 30 (13): 1405–13.
3. Zourdos, Michael C., Alex Klemp, Chad Dolan, Justin M. Quiles, Kyle A. Schau, Edward Jo, Eric Helms, et al. 2016. Novel Resistance Training-Specific Rating of Perceived Exertion Scale Measuring Repetitions in Reserve. Journal of Strength and Conditioning Research 30 (1): 267–75.
The post How to stop tracking macros and trust yourself around food appeared first on Precision Nutrition.
Source: Health1
“I worried that if I stopped tracking macros, I would lose my physique.”
After years of careful macro tracking, Dr. Fundaro finally admitted to herself that the method no longer worked for her. Yet she was afraid to give it up.
If anyone should feel confident in their food choices, it would be Dr. Gabrielle Fundaro. After all, Dr. Fundaro has a PhD in Human Nutrition, a decade-plus of nutrition coaching experience, and six powerlifting competitions under her belt.
Yet, when she was really honest with herself, Dr. Fundaro realized that she felt far from confident around food. For years, she’d used macro counting as a way to stay “on track” with her eating.
And it worked… until it didn’t.
After years of macro tracking, Dr. Fundaro was tired of the whole thing. She was tired of making sure her macros were perfectly in balance. She was sick of not being able to just pick whatever she wanted off a menu and enjoy the meal, trusting that her health and physique wouldn’t go sideways as a result.
Yet the idea of not tracking freaked her out. Every time she quit tracking, she worried:
“What if I don’t eat enough protein, and lose all my muscle?”
“What if I overeat and gain fat?”
“What if I have no idea how to fuel myself without tracking macros? And what does that say about me as an expert in the field of nutrition?”
The more Dr. Fundaro wrestled with macro tracking, the more she wanted to find an alternative.
Something that would support her nutritional goals while also giving her a sense of freedom and peace around food.
Calorie counting wouldn’t do it. That was just as restrictive as counting macros—maybe more.
Intuitive eating didn’t seem like a good fit either. Intuitive eating relies heavily on a person’s ability to tune into internal hunger and fullness cues to guide food choices and amounts. After years of relying on external cues (like her macro targets), Dr. Fundaro didn’t feel trusting enough of her own instincts; she wanted more structure.
Meanwhile, at the gym, Dr. Fundaro began lifting based on the Rate of Perceived Exertion (RPE) scale—a framework that helps individuals quantify the amount of effort they’re putting into a given movement or activity. It’s considered a valuable tool to help people train safely and effectively according to their ability and goals. (More on that soon.)
While using the RPE scale in her training, Dr. Fundaro found she was both getting stronger and recovering better. There was something to this combination of structure and intuition that just worked.
And then, it dawned on Dr. Fundaro like the apple hit Sir Isaac Newton on the head:
If Rate of Perceived Exertion could help her train better, couldn’t a similar framework help her eat better?
With that, the RPE-Eating Scale was born.
Dr. Fundaro has since used this alternative method to help herself and her clients regain confidence and self-trust around food; improve nutritional awareness and competence; and free themselves from food tracking.
(Yup, Dr. Fundaro finally trusts her eating choices—no macro tracker in sight.)
In this article, you’ll learn how she did it, plus:
- What the RPE-Eating scale is
- How to practice RPE-Eating
- How to use RPE-Eating for weight loss or gain
- Whether RPE-Eating is right for you or your clients
- What to keep in mind if you’re skeptical of the concept
What is RPE-Eating?
Invented by Gunnar Borg in the 1960’s, Rate of Perceived Exertion (RPE) is a scale that’s used to measure an individual’s perceived level of effort or exertion during exercise.
Though Borg’s RPE uses a scale that goes from 6 to 20, many modern scales use a 0 to 10 range (which is the range that Dr. Fundaro adapted for her RPE-Eating scale).
Here’s the RPE scale used in fitness.
| Rating | Perceived Exertion Level |
|---|---|
| 0 | No exertion, at rest |
| 1 | Very light |
| 2-3 | Light |
| 4-5 | Moderate, somewhat hard |
| 6-7 | High, vigorous |
| 8-9 | Very hard |
| 10 | Maximum effort, highest possible |
Originally used in physiotherapy settings, the scale is now frequently used in fitness training.
For example, powerlifters might use it to choose how heavy they want to go during a training session. Or, pregnant women might use it to ensure they aren’t over-exerting themselves during a fitness class or strength training session.
Because human experience is highly subjective and individual, the scale allows the exerciser to judge how hard they’re working for themselves. A coach can provide a general guideline, such as “aim for a 7/10 this set,” but it’s up to the client to determine exactly what that means for them.
Dr. Fundaro had used the scale many times with herself, and clients. She always appreciated the sense of autonomy it gave her clients, while still providing some structure.
So, she decided to take the same 1-10 scale and its principles, and apply it to eating.
Here’s what the RPE-Eating Scale looks like:

The goal with RPE-Eating is similar to RPE when training: Develop the skills to determine what is sufficient for you, without having to rely on other external metrics (such as apps or trackers).
How to practice RPE-Eating
If you’ve ever practiced RPE-training, you’ll know it takes some time to get used to. RPE-Eating is the same.
Don’t expect to be in lockstep with all of your body’s internal cues at first, especially if you’ve been ignoring them for a long time.
With this in mind, apply the steps below to practice the RPE-Eating process.
Step #1: Get clear on your goals.
RPE-Eating is not just another diet.
“It’s not about aiming to change your body,” Dr. Fundaro explains. “It’s not about feeling more control over your diet. Nor is it about feeling like you’re eating the ‘optimal’ diet.”
If your priority is maintaining a specific physique (such as staying ultra lean) or changing your body (building muscle or losing fat), this method can be adapted for that, though it isn’t the most efficient one to use.
Instead, RPE-Eating is about sensing into what your body needs and giving yourself appropriate nourishment—while building inner trust and confidence along the way.
“You have to trust that you’ll be able to nourish your body, and that you’ll be okay even though things may change in your body,” says Dr. Fundaro.
Admittedly, this can be challenging to do. It can also be difficult to let go of the expectation that you’ll hit the “right” macros at every meal—which RPE-Eating isn’t specifically designed to do.
However, if your goal is to build more self-trust, RPE-Eating can be a great tool to help you do that.
Step #2: Practice identifying your hunger cues
Before we explore this step, let’s distinguish between two motivators for eating.
First, there’s hunger. Hunger occurs when physical cues in your body (like a general sense of emptiness or rumbling in your stomach, or lightheadedness) tells you that you require energy—known to us mortals as food.
Then, there’s appetite. Appetite is our desire or interest in eating. It can stay peaked even after hunger is quelled, especially if something looks or tastes especially delicious—like a warm, gooey cookie offered after dinner that you feel you have to try, even though you’re technically full.
While it’s normal to eat for both hunger and appetite drives, the two can become mixed up. Especially if we have a history of dieting and tracking food.
The RPE-Eating scale helps you tap back into those true physical hunger cues, and learn the difference between hunger and appetite.
To put this in practice, try this before your next meal:
 Using the RPE-Eating scale mentioned above, identify your current level of hunger. Record the number on paper or the notes app on your phone.
Using the RPE-Eating scale mentioned above, identify your current level of hunger. Record the number on paper or the notes app on your phone.
 Then, eat your meal with as much presence as possible. (Note: This in itself takes practice. It can help to limit distractions, such as eating at the table rather than in front of the TV, and focusing on the flavors and textures of the food you’re eating, and how you feel eating it.)
Then, eat your meal with as much presence as possible. (Note: This in itself takes practice. It can help to limit distractions, such as eating at the table rather than in front of the TV, and focusing on the flavors and textures of the food you’re eating, and how you feel eating it.)
 About halfway through the meal, check in again. Based on the scale, how hungry are you now? As before, record the number.
About halfway through the meal, check in again. Based on the scale, how hungry are you now? As before, record the number.
 If you’re still hungry, finish your meal. When you’re finished, repeat the same process, writing down where you are on the scale.
If you’re still hungry, finish your meal. When you’re finished, repeat the same process, writing down where you are on the scale.
 Once you’re done, take a minute and tune into what your body feels like. What does it feel like to be full? “Download” that feeling into your mind and internalize it in your body, as if you’re updating your phone with the latest software.
Once you’re done, take a minute and tune into what your body feels like. What does it feel like to be full? “Download” that feeling into your mind and internalize it in your body, as if you’re updating your phone with the latest software.
Repeat this for as many meals as you can. Aim to do it for one meal a day for a week or so, or for as long as feels good to you. Don’t worry if you forget: simply repeat the practice when you can.
The more you practice this, the better you’ll become at being attuned with your actual hunger cues. With time, you’ll likely find you develop more trust in your internal compass than what the latest diet tracker says for your needs.
(For more on fully-tuned-in, mindful eating, read: The benefits of slow eating.)
Step #3: Get to know your non-hunger triggers
Have you ever come home after a super stressful day and you’ve basically thrown yourself onto a bag of chips or a carton of ice cream?
We might like to imagine ourselves eating every meal mindfully, using the RPE- Eating system to a tee, but life rarely works like that.
Chances are, there are certain situations that trigger you to eat more quickly, mindlessly, and beyond the point of hunger.
That’s okay.
Dr. Fundaro’s suggestion? Aim to become more aware of the situations that cause you to overeat in the first place.
To do this, you can practice something we use in PN Coaching: Notice and name.
When you find yourself scarfing down food faster than you can blink, simply try to notice what’s going on.
Can you name a feeling—such as anxiety, or sadness?
Can you identify a situation or moment that happened before you started eating—say, an argument with your teenager, or a nasty email from your boss?
Once you’ve identified the feeling, event, or person that’s triggered you to eat compulsively, see if you can also identify what you might really be needing or desiring.
Eating for comfort is normal. However, if it’s the only coping method we have, it can cause more problems than it solves in the long run.
When you find yourself with an urge to eat mindlessly, consider what non-food coping mechanisms might help you feel better. That could be 10 minutes away from your computer to close your eyes and breathe, a walk outside, or a quick call to a friend to rant—or just talk about something completely unrelated.
Getting to know your non-hunger eating triggers—plus widening your repertoire of self-soothing methods—is just as valuable as getting to know your hunger cues. Over time, this awareness will allow you to eat with more intention.
Step #4: Eat for satiety AND satisfaction
Even when you’re “adequately fueled” from a physical perspective, you might still feel unsatisfied from an emotional perspective.
That’s because, according to the RPE-Eating framework, eating should fulfill two criteria:
 Satiety describes the physical sensation of being full; your calorie or fuel needs are met.
Satiety describes the physical sensation of being full; your calorie or fuel needs are met.
 Satisfaction describes a more holistic feeling of being nourished; your calorie needs are met, but your meal also felt pleasurable.
Satisfaction describes a more holistic feeling of being nourished; your calorie needs are met, but your meal also felt pleasurable.
If you ate to satiety only, your calorie needs might be met and your physical hunger quelled, but you might still feel unsatisfied—maybe because chocolate is on your “don’t” list, and even though you’ve eaten everything else in your kitchen that isn’t chocolate, nothing quite “hit the spot.”
In other words, you can eat to satiety at every meal, yet still be “restricting” foods.
You may not be restricting calories per se, but you may have banned entire food groups—baked goods, pizza, or whatever else curls your toes. This can lead to a feeling of constantly needing to police yourself, and doesn’t leave much room for the flexibility and spontaneity that real-life (enjoyable) eating requires.
(Plus, avoiding particular foods tends to work like a pendulum: restrict now; binge later. If you want to learn how to stop those wild swings, read: How to eat junk food: A guide for conflicted humans)
Satisfaction is a key part of eating.
After all, humans don’t just eat for adequate nutrients and energy. We eat for other reasons too: pleasure, novelty, tradition, community, enjoyment.
So, to take your RPE-Eating to the next level, Dr. Fundaro recommends trying it with meals and foods you genuinely enjoy.
If any foods or meals have been “off-limits,” try eating them using the RPE technique. (Macaroni and cheese, anyone?)
Practice using the scale with a variety of meals (including those you may have restricted previously), and notice how you feel over time.
With experience, you’ll get to know what it feels like to adequately fuel yourself with a variety of foods—including those you genuinely enjoy.
How do I know if RPE-Eating is right for me or my clients?
RPE-Eating isn’t for everyone, but might be a good fit for you (or your clients) if:
 You feel dependent on food tracking, but you don’t want to be.
You feel dependent on food tracking, but you don’t want to be.
 Every time you stop tracking, the loss of perceived control freaks you out and drives you right back to tracking.
Every time you stop tracking, the loss of perceived control freaks you out and drives you right back to tracking.
 You want to stop tracking, but you want to have some type of system or guidance in place.
You want to stop tracking, but you want to have some type of system or guidance in place.
 You’re currently tracking (or considering tracking) your food intake, and you have elevated risk factors for developing an eating disorder such as high body dissatisfaction; a history of yo-yo dieting; a history of disordered eating patterns; and/or participation in weight class sports.
You’re currently tracking (or considering tracking) your food intake, and you have elevated risk factors for developing an eating disorder such as high body dissatisfaction; a history of yo-yo dieting; a history of disordered eating patterns; and/or participation in weight class sports.
If you’re a coach looking to use this tool with a client, check out Dr. Fundaro’s resources. Remember this tool may not be for everyone, and how you apply it needs to be flexible.
Note: If you or your client struggles with disordered eating, this tool does not replace working with a health professional who specializes in eating disorders, such as a therapist, doctor, or registered dietician.
How to use RPE- Eating for weight loss or weight gain
According to Dr. Fundaro, the best way to use RPE-Eating is in a weight-neutral setting.
While it could be used for weight modification, she doesn’t recommend treating it as another way to hit your macros or “goal weight.”
“I’m not anti-weight modification,” Dr. Fundaro explains. “I’m pro safe weight modification. I compare weight loss to contact sports. There are inherent risks but they can be mitigated through best practices.”
Dr. Fundaro elaborates: “Since RPE-Eating removes macro-tracking, which can increase risk of disordered eating in some people, and relies on biofeedback and non-hunger triggers, RPE-Eating provides a safety net that macro-tracking alone doesn’t provide.”
But if you do want to use RPE-Eating for intentional weight change, what should you do?
Dr. Fundaro recommends aiming to hover around the ranges that support your goal.
(As a reminder, a 1 to 3 on the RPE-Eating scale is categorized as “inadequate fuel; a 4 to 7 is categorized as “adequate fuel”; and a 8 to 10 is categorized as “excess fuel.”)
 If the goal is weight gain, you’ll likely aim to eat within the 7 to 8 range for most of your meals.
If the goal is weight gain, you’ll likely aim to eat within the 7 to 8 range for most of your meals.
 If the goal is weight loss, you’ll likely aim to eat within the 4 to 5 range for most of your meals.
If the goal is weight loss, you’ll likely aim to eat within the 4 to 5 range for most of your meals.
A key thing to remember is that you would never use RPE-Eating for extreme weight-modification such as for a bodybuilding competition. “That would be like using physio exercises to prepare for a powerlifting competition.” In other words, it’s not the right tool for the job.
Hold up, bro: Isn’t this just feelings over facts?
If you’re skeptical and think this is just eating “based on your feelings,” keep in mind that RPE was once laughed at by lifters, too.
These days, RPE and autoregulation are widely accepted in gym culture and have been studied as a valid method for managing and guiding your training. 1
RPE isn’t perfect, but it’s pretty accurate and incredibly convenient. A lot more convenient than, say, using a velocity loss tracker for every set. 2 3
And while it might seem like it’s all feelings-based, the RPE scale is actually built around practicing the skill of interoceptive awareness—the awareness of internal sensations in your body.
The better you get at the skill of interoceptive awareness, the more you’ll be able to use that awareness to make informed decisions about your training.
RPE-Eating is similar: It builds the skill of sensing into your own body, and lets your internal sensations guide your decisions.
Similar to how the bar slowing down on a squat would indicate you’re getting closer to failure, experiencing the absence of hunger at the end of your meal would indicate you’re closer to being full.
Instead of tracking your glucose levels to validate your perceived hunger, you use internal cues that correlate with lowered blood sugar and coincide with hunger.
And, let’s be real: Being mindful of stomach grumbling or general hunger pangs is much more convenient and accessible than tracking glucose readings.
This process will not be perfect. You may undereat or overeat at first. But over time, with practice, you’ll build the core skills of RPE-Eating.
Are there downsides to RPE-Eating?
While this tool can be helpful, it’s just a tool. A screwdriver is great, but it isn’t useful when you need a hammer.
RPE-Eating can be great for helping you become more aware of your internal hunger cues and build a better relationship with food along the way.
It can also be more laborious. It requires paying real attention to your feelings (physical and emotional), and reflecting on them.
This can be difficult for anyone—but especially people who aren’t able to sit at the table and have a leisurely meal, like parents with small kids, or people with work schedules that require eating on-the-go.
If this is you, just use RPE-Eating when it does work for you—or simply pick and choose specific steps to use in isolation. For example, maybe you try RPE-Eating on the occasional quiet lunch break. Or, maybe you focus solely on developing your awareness of hunger and fullness cues, without trying to change anything else.
If you’ve been tracking macros for a long time, it can be hard to stop.
Tracking macros isn’t inherently bad. It can actually be a helpful tool to teach you more about nutrition. But it’s also not something most people want to do for the rest of their lives.
The problem is, if you’ve depended on tracking your food intake, stopping can feel scary.
In these cases, RPE-Eating can be used as a kind of off-ramp to help transition away from rigid and restrictive macro tracking.
(It can also help loosen the compulsion to “always finish your plate.” Though macros tracking and habitual plate-cleaning may sound different, they’re actually similar: both rely on external cues—such as macro targets or what’s served on your plate—to determine when you’re “done.”)
RPE-Eating won’t take away all the scary feelings that may come with changing ingrained ways of eating.
However, it can provide some structure and language to help you, or your clients, eat with less fear, less stress, and a bit more confidence.
“The goal,” says Dr. Fundaro, “is to know that you’re nourishing yourself—and you don’t need a food tracker to do that.”
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Helms, Eric R., Kedric Kwan, Colby A. Sousa, John B. Cronin, Adam G. Storey, and Michael C. Zourdos. 2020. Methods for Regulating and Monitoring Resistance Training. Journal of Human Kinetics 74 (1): 23–42.
2. Hackett, Daniel A., Nathan A. Johnson, Mark Halaki, and Chin-Moi Chow. 2012. A Novel Scale to Assess Resistance-Exercise Effort. Journal of Sports Sciences 30 (13): 1405–13.
3. Zourdos, Michael C., Alex Klemp, Chad Dolan, Justin M. Quiles, Kyle A. Schau, Edward Jo, Eric Helms, et al. 2016. Novel Resistance Training-Specific Rating of Perceived Exertion Scale Measuring Repetitions in Reserve. Journal of Strength and Conditioning Research 30 (1): 267–75.
The post Private: How to stop tracking macros and trust yourself around food appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD and Helen Kollias, PhD
It’s like my thoughts were under a pile of garbage.
On a Friday night, as my husband and I tried to figure out where to eat, a typical conversation would go like this:
Me: Do you want to go to that restaurant?
Him: What restaurant?
Me: I can’t think of the name. We’ve eaten there before. It’s that place with the peanut shells on the floor? It’s next to… You know… It’s on that road where we used to take the dog to the vet. Do you know the one I’m talking about??
It was as if certain details got lost in a pile of sludge in the deep recesses of my brain. Then, hours later, the details would escape, and I’d shout into an empty room…
“Texas Roadhouse!”
Sludginess with proper nouns is typical for people who are middle-aged and beyond.
However, what seemed to be happening to me, increasingly in my late 40s and early 50s, felt far from typical.
Not only could I never seem to spit out the names of various restaurants or people or books or movies or so many other things, but my brain was also pooping out during the workday.
I’d sit in front of my computer screen, stare at a document, and will myself to do something constructive with my fingertips. Everything seemed hazy, like those first few moments in the morning when you’re awake enough to turn off the alarm but too sleepy to do basic math.
I had my good moments, usually in the morning, when I attempted to pack eight hours of writing into the two or three hours I possessed mental clarity.
On my worst days, however, I awoke with a haze I never managed to shake. Work was a non-starter. Nor did I have enough bandwidth to read, or do much of anything, really.
I sought medical advice.
Three healthcare professionals recommended antidepressants. I tried one, and felt even worse. I tried another. I tried yet another at a higher dose. Still, I felt like a zombie. Another professional gave me a sleeping pill. It left me feeling even more drugged.
Someone tested my thyroid. There was nothing wrong with it. Nor was I anemic. I tried supplements, mushroom coffee, and just about any product with the word “think” somewhere on its label.
Finally, after nearly two years of seeing a revolving door of doctors, I made an appointment with a gynecologist for my yearly exam. I mentioned vaginal dryness. That information triggered her to ask a string of questions that had nothing to do with my undercarriage. How was my sleep? Mood? Energy levels? Was I experiencing hot flashes? How about brain fog?
“Funny you should mention brain fog,” I said in my usual hazy monotone. “I feel like I’m barely alive.”
By the end of the visit, I understood that I’d likely never had depression.
What I “had” was menopause.
My gynecologist sent me home with prescriptions for estradiol and progesterone.
Within days, it was as if someone had flipped a switch.
I could think again. I could type words again. I could follow conversations. I could work past noon.
And, for the first time in years, I could sleep more than two hours without waking.
Now, menopause isn’t a medical condition.
Nor is it a disease.
Instead, like puberty, it’s a life stage—a transitional moment to be precise.
Once you’ve gone 12 consecutive months without a period, you’ve reached menopause. And from that moment onwards, you’re officially “postmenopausal.”
As women approach this transitional moment, hormone levels fluctuate and fall, triggering dozens of symptoms. Weight gain and reduced sex drive get a lot of attention.
However, during and after menopause, roughly 40 percent of women report increased irritability, mood swings, anxiety, fatigue, and trouble concentrating, according to the American College of Obstetricians and Gynecologists.1 2 As the following image shows, it’s also one of the most vulnerable times in a woman’s life to develop depression,3 particularly if they’ve struggled in the past with it before.
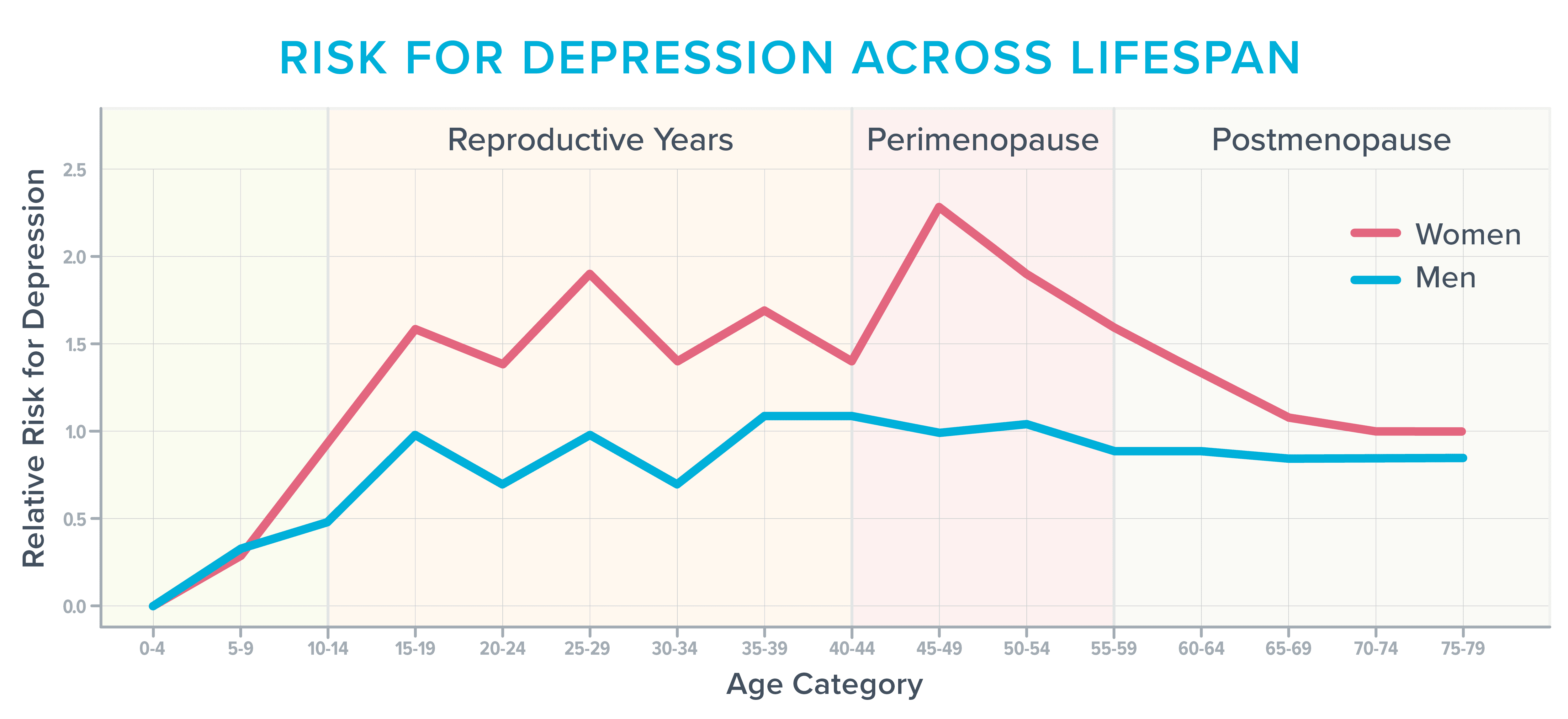
Before starting hormones, I often found myself sobbing for no reason. Other times, the world’s stimuli felt too… stimulating.
Normal everyday sounds—like the buzz of traffic or people at the mall—literally hurt. I was jumpy and irritable and felt anxious about situations that had never bothered me in the past, such as driving over bridges or through construction.
It’s not completely clear what drives these cognitive and emotional symptoms.
Fluctuating hormone levels likely play a role, as do typical age-related changes in the brain.
In addition, during this stage of life, women often deal with several issues that siphon cognitive capacity faster than a thirsty vampire drains a carotid.
During their 40s and 50s, for example, many women have reached the peak of their careers, with responsibilities that follow them home and keep them up at night. They may also be parenting angst-filled teens, caring for aging parents, adjusting to an empty nest, questioning their marriage, or trying to wrap their bank account around the latest statement from the college bursar or hospital billing department.
However, one of the lesser-known and talked about triggers for cognitive discontent has nothing to do with aging or life stress and everything to do with that hallmark menopausal symptom: the hot flash.
Anatomy of a hot flash
Hot flashes, which happen during the day, and night sweats, which occur at night, fall under the category of vasomotor symptoms. (The word “vasomotor” refers to the constriction or dilation of blood vessels which, in turn, can influence everything from blood pressure to sweating.)
During a hot flash or night sweat, norepinephrine and cortisol levels rise. Blood vessels dilate in an attempt to shed heat. Blood pressure and heart rate increase.
Depending on the severity of the hot flash, your skin might redden as sensations of warmth spread through your face, neck, and chest.
You might sweat, experience heart palpitations, or feel anxious, tired, or faint.4
It’s not entirely clear why hot flashes crop up around menopause.
According to one theory, falling estrogen levels affect the hypothalamus, the area of the brain involved in temperature regulation. The brain’s internal thermostat gets wonky and occasionally thinks your body is too hot or cold (when it’s not).
How vasomotor symptoms change the brain
For many years, experts thought of vasomotor symptoms as mere inconveniences or sources of embarrassment.
(To be honest, so did I. During all of those fruitless visits to various healthcare professionals, it never occurred to me to mention them.)
However, an increasing body of research has revealed that hot flashes may do more than make us uncomfortable or force us to change our sheets in the middle of the night.
They may also affect our blood vessels and brains—and not for the better.5 For this reason, an increasing number of experts now consider vasomotor symptoms to be a treatable medical condition.6 7 8
Hot flashes and brain lesions
In one study, researchers asked 226 women to wear monitors that tracked when they were experiencing a hot flash. The women also underwent magnetic resonance imaging (MRI), filled out sleep diaries, and wore smartwatches that recorded how often they woke at night.9
As researchers looked at the brain images obtained from women who experienced the most hot flashes, they noticed an abundance of patchy areas called whole-brain white matter intensities.
These lesions were once thought of as a typical consequence of aging. However, neuroscientists now believe that the presence of whole-brain white matter intensities is predictive of future cognitive decline.
People with an abundance of these brain lesions are twice as likely to get diagnosed with dementia and three times as likely to have a future stroke.10
The blood vessel connection
It’s thought that the increased presence of whole-brain white matter intensities may stem, in part, from changes taking place in the blood vessels that feed the brain.
A three-year study of 492 women supports that theory. It determined that women who experienced frequent hot flashes also tended to experience unhealthy changes in their blood vessels, such as an inability to dilate to accommodate increased blood flow.11
Other research has linked frequent hot flashes with increases in the following:
- Thickening in the carotid arteries that supply blood to the brain, face, and neck12
- Body fat
- Total and LDL cholesterol
- Insulin resistance13 14 15 16
The sleep connection
In addition to directly affecting the blood vessels, frequent hot flashes may also affect the brain by disturbing sleep.17
Interestingly, many women don’t necessarily know that hot flashes are disturbing their sleep.
They may instead—as I did—assume they have insomnia or sleep apnea.
That’s because night sweats aren’t always sweaty.
By the time a surge in cortisol and norepinephrine jolts a woman awake, the hotness of the flash may have dissipated. So, it can feel as if she’s repeatedly waking, over and over and over again, for no discernable reason.
These frequent awakenings may interfere with the brain’s ability to consolidate memories, metabolize toxins, and store all the names, dates, and facts one encounters daily.
It can also lead to lost connectivity in the hippocampus, a part of the brain that’s important for learning and memory.
Sleep loss also means the amygdala, a part of the brain involved in emotion, becomes more reactive, causing people to feel more easily stressed, anxious, irritable, frustrated, or enraged.18 19
All of these brain changes can set in after just days to a week of lost sleep. So, imagine what happens when you’ve been waking over and over again—for years.
Why it can be hard to get help
To diagnose depression, healthcare professionals use a tool called the Patient Health Questionnaire (PHQ-9) depression scale. If you check off four of the nine symptoms on the scale, you’re considered depressed.
However, four of the symptoms on the checklist also overlap with the symptoms of menopause-related sleep deprivation:
- Little interest or pleasure in doing things
- Trouble falling or staying asleep
- Feeling tired or having little energy
- Trouble concentrating on things, such as reading the newspaper or watching television
Check off those four items, and you might be diagnosed with depression, even if what’s really ailing you is the battle with sleep you’ve been waging since you turned 47.
A lack of menopause-specific training
Another problem: On surveys, 80 percent of medical residents admit they feel “barely comfortable” talking about menopause.20 In addition, few residency programs—including ob-gyn residency programs—offer training in it.21
Given the above, it’s no wonder so many healthcare professionals never think to ask about hot flashes or sleep disturbances when people like me show up complaining of fatigue, lack of gumption, and an inability to focus.
In addition, even when it’s clear that vasomotor symptoms are leading to cognitive and emotional symptoms, many healthcare professionals still shy away from prescribing menopausal hormone therapy (also called hormone replacement therapy, or HRT), often telling women that supplemental hormones are “not safe” or “too risky.”
These professionals are practicing what Michigan-based menopause-trained gynecologist Jerrold H. Weinberg, MD, calls “defensive medicine.”
“It’s one of the first reflexes doctors have when they recommend a treatment,” says Dr. Weinberg. “They worry they’re going to get sued.”
What the research actually says about hormone therapy
These worries are based on research done several decades ago that linked the use of certain types of hormones with a slightly increased risk of developing breast cancer or stroke.22
However, according to more recent research, that small increased risk seems to depend on several other factors, such as age, dose, the type of hormonal preparation, and the duration of hormone use.23 24
As long as you’re younger than 60 and have been postmenopausal for fewer than 10 years, many experts now say the benefits outweigh the risks for women with moderate to severe menopausal symptoms.25
It’s also counterbalanced by health benefits such as reduced risk of developing Alzheimer’s disease or osteoporosis, says Dr. Weinberg, who confirms the health benefits of menopause hormone therapy far outweigh the risks for most women.
Because some antidepressants can lift mood, improve sleep, and reduce hot flashes, some healthcare professionals turn to them instead of menopause hormone therapy. As with any medicine, antidepressants have their own list of side effects. However, for someone practicing defensive medicine, they often seem like a safer bet, says Dr. Weinberg.26 27 28
How to advocate for your health
If you or your client are on what seems like a never-ending quest to find a healthcare professional who understands menopause, use the following advice from Dr. Weinberg and Helen Kollias, PhD, an expert on physiology and molecular biology and science advisor at Precision Nutrition and Girls Gone Strong.
 Seek care from a menopause-trained health professional.
Seek care from a menopause-trained health professional.
Usually, these professionals list this training and interest in their bio. For example, they might list “menopause” as an area of focus.
You can also search this database for practitioners who have earned a certification from the Menopause Society.
 Document your symptoms.
Document your symptoms.
Write them down. That way, if you feel foggy or nervous during your appointment, you can lean on your notes.
This information can also help you judge whether MHT or another medicine is working. Based on your symptom data, you and your healthcare professional may decide to switch to a different medicine or change your dose.
Consider tracking:
- How often you get hot flashes
- The number of hours in a typical day you find yourself battling brain fog
- How often you experience fatigue, anxiety, rage, or some other symptom
- How often you wake up at night
 Be as specific as you can during your appointment.
Be as specific as you can during your appointment.
Saying something like “I don’t sleep well,” is less likely to get you the right kind of help than saying, “During the past seven days, I’ve only gotten four uninterrupted hours once. I wake, on average, five times a night. On a typical night, my longest stretch of sleep is three hours.”
If you use a smartwatch, come ready to fire up your health app, so your healthcare professional can see the data.
 Talk about the pros and cons of treatment.
Talk about the pros and cons of treatment.
There’s a concept in medicine known as “shared decision-making.” Part of that process involves frank discussions about the benefits and risks of a given treatment. Then, patients and clinicians work together to make decisions based on those benefits and risks.
Many healthcare networks encourage clinicians to use shared decision-making, as it seems to reduce patient complaints as well as malpractice lawsuits.29 30
For this reason, shared decision-making can help shift a healthcare professional out of the “defensive medicine” mindset.
You might ask questions like:
- “I’m interested in seeing if menopausal hormone therapy might be helpful. Could we discuss if I’m a good candidate?”
- “I’ve read that menopausal hormone therapy could slightly increase my risk of breast cancer. Could you help me understand my personal breast cancer risk based on my family history, age, body weight, and lifestyle?”
- “Osteoporosis runs in my family, as does dementia. I’ve heard that menopausal hormone therapy might help to reduce the risk for both, in addition to helping me sleep. Could you help me weigh the pros and cons?”
How to improve mental and emotional health during menopause: 9 lifestyle strategies
The lifestyle habits that improve mental and emotional health during menopause aren’t terribly different from the lifestyle habits that improve overall health—for any person, at any stage of life.
Other than avoiding caffeine, alcohol, and spicy or hot foods, there’s no special diet for people with vasomotor symptoms. (And by the way, tofu and other soy products don’t seem to help with vasomotor symptoms as much as once thought30—though they’re still nutritious.)
Strategy #1: Lean into fundamental health strategies.
Healthy behaviors don’t necessarily change during middle age.
Nutrition, physical activity, stress management, sleep, social connectedness, and a sense of purpose matter just as much during the menopausal transition as they do when we’re younger. However, these fundamentals are even more important to dial in as life progresses.
So consider:
- Are you setting aside enough time for sleep and rest?
- Are you physically active?
- Are you eating a diet that’s mostly minimally processed and full of brightly colored produce, healthy fats, lean protein, fibrous vegetables, and legumes?
- Do you regularly connect with other humans in ways that help you buffer stress and feel supported?
- Do you find ways to experience awe, joy, curiosity, peace, and purpose?
If you answered “no” to some or all of those questions, consider why that is. What’s stopping you? How might you remove barriers or shore up support to make those fundamentals easier?
Strategy #2: Experiment with creatine.
In addition to helping to blunt age- and hormone-related losses in muscle and bone mass, creatine may also help bolster mood and brain function while reducing mental fatigue.
It also seems to counter some of the negative effects of sleep deprivation. 32 33 Research shows a daily dose of 5 to 7 grams of creatine monohydrate is effective.
Strategy #3: Get regular about light exposure.
In addition to helping you feel alert, sunlight helps to set the internal clock in your brain that makes you sleepy at night and spunky in the morning. Morning and late afternoon light exposure seem particularly potent.
In a study of 103 people, exposure to morning sunlight predicted better sleep quality the following night. When people spent time outdoors in the mornings, they fell asleep more quickly, slept longer, and experienced fewer awakenings the following evening.34
Sunlight may also improve mood and concentration.35
Strategy #4: Go easier at the gym.
If you’re already worn out, long, intense exercise sessions will likely make you feel worse.
For one, injuries crop up much more easily at middle age than during our 20s and 30s. In addition, it takes longer to recover between sessions.36
String too many overly zealous workouts too close together, and you’ll not only likely start to feel achy but also more irritable, tense, and tired.
However, much like a cold shower, short bursts of exercise may help you to feel alert during the day.
If you’re falling asleep at your desk, encourage yourself to take short movement breaks such as a 5- or 10-minute walk outdoors or a quick set of pushups or squats.
In addition, you may find gentle exercise—such as yoga or stretching—helps you relax before bed. Just don’t make it too intense, or you’ll trigger a release of adrenaline.
Whenever you exercise, tune into how your body feels, especially after a particularly bad night of sleep.
We’re not saying you should never exercise vigorously or try to beat your lifting PRs. However, depending on your sleep and recovery, you might want to pare things back, especially if you’ve traditionally hit the gym hard.
You can still do intense sessions—just balance them out with more moderate sessions, as well as proportionate recovery.
Depending on how you feel, you might decide to go all out, as usual.
However, you might also decide to do a zone 2 training session instead of an intense run. Or, if you’re resistance training, you might still do your planned session, but reduce the number of sets, reps, or volume lifted.
Strategy #5: Investigate Cognitive Behavior Therapy for Insomnia (CBT-I).
This research-based therapy for insomnia can help you develop skills and mental reframes that encourage sound sleep.
For example, a CBT-I therapist will help you develop the skill of getting up at the same time every day, regardless of how badly you slept (or didn’t sleep) the night before.
(Read more: Three CBT-I skills that can transform how you sleep.)
Strategy #6: Get real about stress.
You may not have the energy (or desire) to do everything you did when you were younger. (When you were 36, your daily checklist defied time and space.)
As a result, you might benefit from looking critically at your current responsibilities to see which ones you can shrink or downsize. For several days, track how you spend your time and bandwidth. Then, analyze your data.
Ask yourself:
- Is this how you truly want to spend your time and energy?
- Does your current schedule allow you to rest, recover, and tend to your own needs? Or, do you spend nearly all of your time and energy caring for and providing for others?
- What changes could you make to prioritize rest and recovery?
If you’re a coach, use the Wheel of Stress Assessment to help clients identify different dimensions of their life that might be draining their mental and emotional capacity. (When you know specifically where your stress is coming from, you have a better chance of resolving it.)
If it’s demands from other people that prevent you from prioritizing self-care and recovery, you might like to read: How saying “no” can seriously change your life.
Strategy #7: Experiment with cooling technology.
You might find you sleep better and experience fewer night sweats if you sleep in a cooler environment.
Try turning down the thermostat a couple of degrees, using a fan, or investing in an electric cooling mattress pad.
Strategy #8: Take frequent breaks.
When you feel the fog take over your brain, it’s not likely you’ll be doing “your best work” anyway.
So, for a block of time—say, 20 minutes—permit yourself to do nothing. You might:
- Relax with a cold beverage
- Cuddle with a pet
- Gaze out a window
- Sit outdoors while listening to the birds
- Call a friend
If you need a quick “refresh,” you can also try a 5-minute mind-body scan.
Get your body into a comfortable position. For example, you might use the yoga “legs up the wall” pose or lie down and place a pillow under your knees.
Then, close your eyes and bring your attention to physical sensations in your body. Start at your head, and work your way down to your toes.
Don’t judge or rush to change anything. Just observe, like a scientist. You can also scan your mind, for example, by noticing thoughts.
When you’ve completed the scan, consider:
- What are you feeling physically?
- What are you feeling emotionally?
- What are you thinking?
You don’t have to “do” anything with the information you uncover, just notice.
Strategy #9: Follow a diet that promotes healthy circulation.
The foods that protect the blood vessels around your heart can also protect the blood vessels in your brain.
For example, both the MIND and Mediterranean diets are associated with a reduced risk of Alzheimer’s disease and depression.37 38 These eating patterns are rich in vegetables, fruit, whole grains, olives, beans, fish, and other minimally-processed whole foods.
In addition, nitrate-rich foods like beets and dark, leafy greens may help to dilate blood vessels, temporarily improving memory by helping more blood to reach the brain.39 40
(For more on how our diet can support brain function and emotional regulation, read: Nutrition and mental health: What (and how) to eat)
The upside of menopause
It’s frustrating when you feel like you can’t do it all.
Believe me. I know.
However, this stage of life presents a hidden opportunity, forcing you to re-evaluate what’s most important.
Before going on hormones, as my ability to type coherent words and phrases diminished, I was forced to ask an important question:
Do I really need to be doing this?
It was more of an existential question than a career-related one, and it allowed me to reassess how I wanted to spend my limited mental resources.
Given that I was self-employed, I didn’t actually need to be working eight hours a day. That was a gift, wasn’t it?
Maybe I also didn’t need to cook dinner six nights out of seven. Maybe the recipes I chose could be simplified, too.
Finally, maybe saying “no” a lot more often and without regret would allow me to continue to say yes to the things that mattered most.
Things like visiting my aging parents.
And picking up the phone whenever my kid called from college.
Or meeting a friend for a meandering walk around town.
Thanks to the hormones and life tweaks, I now have energy again. I’m also clear-headed most of the time. However, I still tend to end my work day around 3 p.m.
Why?
Because I can, and I want to.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- Mood Changes During Perimenopause Are Real. Here’s What to Know [Internet]. [cited 2024 Nov 1]. Available from: https://www.acog.org/womens-health/experts-and-stories/the-latest/mood-changes-during-perimenopause-are-real-heres-what-to-know
- Gordon JL, Eisenlohr-Moul TA, Rubinow DR, Schrubbe L, Girdler SS. Naturally occurring changes in estradiol concentrations in the menopause transition predict morning cortisol and negative mood in perimenopausal depression. Clin Psychol Sci. 2016 Sep;4(5):919–35.
- N.d. Accessed November 20, 2024. https://nap.nationalacademies.org/read/27757/chapter/8.
- Lugo T, Tetrokalashvili M. Hot flashes. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024.
- Andrews R, Lacey A, Bache K, Kidd EJ. The role of menopausal symptoms on future health and longevity: A systematic scoping review of longitudinal evidence. Maturitas. 2024 Sep 30;190(108130):108130.
- Thurston RC, Chang Y, Wu M, Harrison EM, Aizenstein HJ, Derby CA, et al. Reproductive hormones in relation to white matter hyperintensity volumes among midlife women. Alzheimers Dement. 2024 Sep;20(9):6161–9.
- Thurston RC, Maki P, Chang Y, Wu M, Aizenstein HJ, Derby CA, et al. Menopausal vasomotor symptoms and plasma Alzheimer disease biomarkers. Am J Obstet Gynecol. 2024 Mar 1;230(3):342.e1-342.e8.
- Thurston RC, Wu M, Barinas-Mitchell E, Chang Y, Aizenstein H, Derby CA, et al. Carotid intima media thickness and white matter hyperintensity volume among midlife women. Alzheimers Dement. 2023 Jul;19(7):3129–37.
- Thurston RC, Wu M, Chang Y-F, Aizenstein HJ, Derby CA, Barinas-Mitchell EA, et al. Menopausal vasomotor symptoms and white matter hyperintensities in midlife women. Neurology. 2023 Jan 10;100(2):e133–41.
- Wardlaw JM, Valdés Hernández MC, Muñoz-Maniega S. What are white matter hyperintensities made of? Relevance to vascular cognitive impairment: Relevance to vascular cognitive impairment. J Am Heart Assoc. 2015 Jun 23;4(6):001140.
- Thurston RC, Sutton-Tyrrell K, Everson-Rose SA, Hess R, Matthews KA. Hot flashes and subclinical cardiovascular disease: findings from the Study of Women’s Health Across the Nation Heart Study: Findings from the Study of women’s Health Across the Nation Heart Study. Circulation. 2008 Sep 16;118(12):1234–40.
- Thurston RC, Chang Y, Barinas-Mitchell E, Jennings JR, Landsittel DP, Santoro N, et al. Menopausal Hot Flashes and Carotid Intima Media Thickness Among Midlife Women. Stroke. 2016 Dec;47(12):2910–5.
- Thurston RC, Sowers MR, Sternfeld B, Gold EB, Bromberger J, Chang Y, et al. Gains in body fat and vasomotor symptom reporting over the menopausal transition: the study of women’s health across the nation. Am J Epidemiol. 2009 Sep 15;170(6):766–74.
- Thurston RC, El Khoudary SR, Sutton-Tyrrell K, Crandall CJ, Gold EB, Sternfeld B, et al. Vasomotor Symptoms and Lipid Profiles in Women Transitioning Through Menopause. Obstetrics & Gynecology. 2012 Apr;119(4):753–61.
- Thurston RC, El Khoudary SR, Sutton-Tyrrell K, Crandall CJ, Sternfeld B, Joffe H, et al. Vasomotor Symptoms and Insulin Resistance in the Study of Women’s Health Across the Nation. The Journal of Clinical Endocrinology & Metabolism. 2012 Oct;97(10):3487–94.
- Thurston RC, Chang Y, Barinas-Mitchell E, Jennings JR, von Känel R, Landsittel DP, et al. Physiologically assessed hot flashes and endothelial function among midlife women. Menopause. 2017 Aug;24(8):886–93.
- Thurston RC, Chang Y, Buysse DJ, Hall MH, Matthews KA. Hot flashes and awakenings among midlife women. Sleep [Internet]. 2019 Sep 6 [cited 2024 Oct 31];42(9). Available from: https://pubmed.ncbi.nlm.nih.gov/31152182/
- Roy S. Sleep Deprivation Harms Memory Via Loss of Connectivity Between Hippocampus Neurons [Internet]. Sleep Review. 2016 [cited 2024 Oct 31]. Available from: https://sleepreviewmag.com/sleep-health/demographics/age/sleep-deprivation-harms-memory-via-loss-connectivity-hippocampus-neurons/
- Minkel JD, Banks S, Htaik O, Moreta MC, Jones CW, McGlinchey EL, et al. Sleep deprivation and stressors: evidence for elevated negative affect in response to mild stressors when sleep deprived. Emotion. 2012 Oct;12(5):1015–20.
- Dorr B. Contributor: In the Misdiagnosis of Menopause, What Needs to Change? [Internet]. AJMC. 2022 [cited 2024 Oct 31]. Available from: https://www.ajmc.com/view/contributor-in-the-misdiagnosis-of-menopause-what-needs-to-change-
- Allen JT, Laks S, Zahler-Miller C, Rungruang BJ, Braun K, Goldstein SR, et al. Needs assessment of menopause education in United States obstetrics and gynecology residency training programs. Menopause. 2023 Oct 1;30(10):1002–5.
- Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 2002 Jul 17;288(3):321–33.
- Nerattini M, Jett S, Andy C, Carlton C, Zarate C, Boneu C, et al. Systematic review and meta-analysis of the effects of menopause hormone therapy on risk of Alzheimer’s disease and dementia. Front Aging Neurosci. 2023 Oct 23;15:1260427.
- Gosset A, Pouillès J-M, Trémollieres F. Menopausal hormone therapy for the management of osteoporosis. Best Pract Res Clin Endocrinol Metab. 2021 Dec;35(6):101551.
- Garrison JA. UpToDate. J Med Libr Assoc. 2003;91(1):97.
- Newhouser LM, Maneval M, Rayalam K, Sabeeh G, Varela L. SSRIs vs. SNRIs for vasomotor symptoms of menopause. Am Fam Physician. 2022 Apr;105(4):430–1.
- Wu C-K, Tseng P-T, Wu M-K, Li D-J, Chen T-Y, Kuo F-C, et al. Antidepressants during and after menopausal transition: A systematic review and meta-analysis. Sci Rep. 2020 May 15;10(1):8026.
- Schoenfeld EM, Mader S, Houghton C, Wenger R, Probst MA, Schoenfeld DA, et al. The effect of shared decisionmaking on patients’ likelihood of filing a complaint or lawsuit: A simulation study. Ann Emerg Med. 2019 Jul 3;74(1):126–36.
- US Preventive Services Task Force, Davidson KW, Mangione CM, Barry MJ, Nicholson WK, Cabana MD, et al. Collaboration and shared decision-making between patients and clinicians in preventive health care decisions and US Preventive Services Task Force recommendations. JAMA. 2022 Mar 22;327(12):1171–6.
- Gençtürk N, Bilgiç FŞ, Kaban HU. The effect of soy isoflavones given to women in the climacteric period on menopausal symptoms and quality of life: Systematic review and meta-analysis of randomized controlled trials. Explore (NY). 2024 May 22;20(6):103012.
- Smith-Ryan AE, Cabre HE, Eckerson JM, Candow DG. Creatine Supplementation in Women’s Health: A Lifespan Perspective. Nutrients [Internet]. 2021 Mar 8;13(3).
- Gordji-Nejad A, Matusch A, Kleedörfer S, Jayeshkumar Patel H, Drzezga A, Elmenhorst D, et al. Single dose creatine improves cognitive performance and induces changes in cerebral high energy phosphates during sleep deprivation. Sci Rep. 2024 Feb 28;14(1):4937.
- Anderson AR, Ostermiller L, Lastrapes M, Hales L. Does sunlight exposure predict next-night sleep? A daily diary study among U.S. adults. J Health Psychol. 2024 Jul 30;13591053241262643.
- Burns AC, Windred DP, Rutter MK, Olivier P, Vetter C, Saxena R, et al. Day and night light exposure are associated with psychiatric disorders: an objective light study in >85,000 people. Nat Ment Health. 2023 Oct 9;1(11):853–62.
- Li DCW, Rudloff S, Langer HT, Norman K, Herpich C. Age-Associated Differences in Recovery from Exercise-Induced Muscle Damage. Cells [Internet]. 2024 Jan 30;13(3).
- Agarwal P, Leurgans SE, Agrawal S, Aggarwal NT, Cherian LJ, James BD, et al. Association of Mediterranean-DASH Intervention for Neurodegenerative Delay and Mediterranean diets with Alzheimer disease pathology. Neurology. 2023 May 30;100(22):e2259–68.
- Wightman EL, Haskell-Ramsay CF, Thompson KG, Blackwell JR, Winyard PG, Forster J, et al. Dietary nitrate modulates cerebral blood flow parameters and cognitive performance in humans: A double-blind, placebo-controlled, crossover investigation. Physiol Behav. 2015 Oct 1;149:149–58.
- Ventriglio A, Sancassiani F, Contu MP, Latorre M, Di Salvatore M, Fornaro M, Bhugra D. Mediterranean Diet and its Benefits on Health and Mental Health: A Literature Review. Clin Pract Epidemiol Ment Health. 2020 Jul 30;16(Suppl-1):156–164
- Heiland EG, Lindh F, Regan C, Ekblom Ö, Kjellenberg K, Larsen FJ, et al. A randomised crossover trial of nitrate and breakfast on prefrontal cognitive and haemodynamic response functions. Npj Sci Food. 2024 Sep 13;8(1):64.
The post Menopause and mental health: The science of the menopausal brain appeared first on Precision Nutrition.
Source: Health1
“I work with coaches and other people who know too much.”
Kate Solovieva is a former professor of psychology, a PN master coach, and PN’s director of community engagement.
And the above quote has become one of her taglines.
Though Coach Kate has coached thousands of “regular” clients, her specialty is coaching other coaches.
Through her work as an instructor with PN’s Level 2 Master Health Coaching Certification, a facilitator for PN’s private online coaching communities, and a coach in her own private practice, she gets a front-row view of all the questions and challenges both new and seasoned coaches have.
Coach Kate knows what other coaches are up to.
She’s seen the victories and the blunders of thousands of coaches, and today, she’ll share three common mistakes she sees them making.
If there’s anything Coach Kate wants, it’s to see her peers achieve wild success, so her hope with this article is to help coaches:
- Stop feeling paralyzed by insecurity and doubt—and start growing their business
- Learn to see their clients more objectively, so they can best serve their needs and goals
- Clearly identify their responsibilities as a coach (hint: they’re’ not what many coaches think they are)
- Harness their natural passion and investment in a client’s success—without burning themselves out
We’ll cover three common coaching mistakes, plus the solutions to overcome them. Let’s get into it.
Coaching mistake #1: Focusing on coaching instead of selling
Coach Kate describes a coaching business as a three-legged stool.
- There’s the coaching leg (which is your skills and knowledge as a coach),
- A selling leg (which is your ability to market and attract a flow of clients), and
- An administrative leg (which includes how clients book appointments, make payments, and other organizing tools and systems).
“The vast majority of folks who get into coaching start with the coaching leg,” says Kate.
“They want to become the best coach they can be, which is amazing. However, to become the best coach you can be, information and theory only get you so far.”
As Kate says, “You cannot become the best coach you can be in a vacuum, talking to yourself in your office.”
Which is why she suggests challenging the desire many coaches have to wait until their knowledge is “complete.”
Instead, she suggests, just start selling.
Why?
Coaches who start selling sooner also get to start coaching sooner.
Over time, they’ll have an advantage over the coaches who want to be “the BEST coach they can be” by getting 12 certifications before selling their services.
Meanwhile, the coach who “doesn’t really know what they’re doing” but has started practicing anyway will begin building their business and their coaching experience—and likely improve their odds of overall success.
Solution: Remember to show up as a COACH, not an EXPERT
There’s a natural inclination among aspiring coaches who want to do a good job to get those 12 certifications before they start coaching.
“Sometimes we hold on to this hope that we’ll get to a point where we feel confident enough at fielding any question that ever comes our way,” Kate says.
Because as every coach knows, when you start telling people what you do, they’ll have questions. And often, they’ll have questions you can’t answer, and that can feel uncomfortable… mortifying even.
(You’re supposed to be the expert, right??)
According to Coach Kate, the above belief—that you’re supposed to be an authority with all the answers—is based on an erroneous assumption.
“When I show up to a coaching conversation, my role is not ‘the expert,’” she says.
Yes, coaches have to show up to client interactions with a baseline of nutrition knowledge. (For example, if a client asks you about good sources of protein, you should be able to list some.)
But coaches don’t have to show up with a prepared lecture, or encyclopedic knowledge of nutrition minutia or biochemistry. (You don’t have to feel bad if you can’t recall the ratio of omega 3 to omega 6 in flax oil, or all the steps in the Krebs cycle that produces ATP.)
Even when you know the answer, Kate suggests that not answering right away can actually be more productive.
“If a client asks you about seed oils, you can simply say, ‘That’s a great question. I can get you some information on that if you’d like, but I’m curious, why do you ask?’”
While the expert might respond with a summary of the latest research on seed oil processing and its health effects, the coach will strive to learn more about why the question is meaningful to the client.
For example, after inquiring further, you may learn that your client heard about seed oils from their friend Susan, who changed the fat sources in her diet and lost ten pounds. And the client is curious to see if they might also lose ten pounds if they eliminate seed oils.
With this kind of response, you learn more about what the client is really after (a weight loss solution), which ultimately helps direct you to more effective strategies (which probably have nothing to do with seed oils).
 Takeaway nugget:
Takeaway nugget:
Coaches should have a firm understanding of fitness and nutrition principles.
However, clients often don’t need more information; they need coaching.
When a client asks you a question, consider whether the answer will help them take action.
If it will, offer them what you know. (If you don’t know the answer, you can simply say, “I’m happy to find more information about that for you.”)
If it won’t, consider turning their question into a coaching opportunity. Ask, “Can you tell me why you’re curious about that?” Their answers will likely lead you to a more productive conversation.
Coaching mistake #2: Assuming your clients are exactly like you
Now, maybe it sounds obvious that clients aren’t just clones of us.
That said, especially when we feel all warm and vibe-y with our clients, it can be easy to forget in the moment.
For example, maybe you’re someone who…
- Tracks macros, and feels it’s relatively simple and effective. So you assume this approach will work on most clients (even though many will find it triggering and overwhelmingly complicated).
- Coaches virtually, so your clients are all over the world. You might recommend meeting certain protein targets, without considering that in some communities, protein dense foods might either be hard to access, prohibitively expensive, or both.
- Prioritizes fitness. And for the life of you, you can’t understand why your client would skip a lunch workout because she doesn’t want to mess up her hair and makeup in the middle of a work day.
If you’re a coach, you probably went into this line of work because you value nutrition, exercise, and overall health. And often, we assume our clients hold these same values. But the truth is, that’s not always the case.
Says Kate:
“There’s nothing inherently superior about valuing your health. If you do, yes, you’ll probably experience better health and live longer. But not everyone shares those values. That’s a tough one to swallow.”
Of course, without seeing your clients for the unique people they are—with their own individual preferences, values, and goals—you may find yourself suggesting behaviors that aren’t possible for them, or striving for goals that aren’t meaningful to them.
Over time, this becomes frustrating for your clients and you: They feel like you don’t “get” them, and you feel like a “bad” coach.
Solution: Get a clear picture of the client’s baseline—and determine what actions they’re ready, willing, and able to take
The opposite of assuming (often unconsciously) that clients are like you is, well, assuming nothing.
As best as you can, check your biases and assumptions at the door, and approach each client session with an open, curious mind.
Ask questions, such as:
“What inspired you—or pushed you—to come in today?”
And:
“Why is that goal meaningful to you?”
And:
“What skills do you have today that might help you achieve your goal? What skills do you feel you might be missing?”
Listen.
Withholding assumptions can be particularly difficult when clients share some obvious similarities with you. (Perhaps they’re also a single mom, or they’re also training for a triathlon, or they’re also a cancer survivor.)
But even when clients share similar experiences or goals, their biology, social context, personal history, and many other factors can make their “similar” experiences, in fact, totally different.
Coach Kate says in these cases, you can show that you relate to them, while also inviting them to describe their own experience. She suggests using the following question:
“I know what [insert shared experience] has been like for me, but what has [insert shared experience] been like for you?”
Once you have a clear picture of a client’s values, priorities, and reasons for change, you can assess which actions they’re ready, willing, and able to take. (Again, don’t make assumptions here. Just because you find meal prep quick and easy, doesn’t mean your client will.)
If you want to go through this exercise with your client on paper, use our Ready, Willing, and Able Worksheet.
 Takeaway nugget:
Takeaway nugget:
Remember that clients:
- Aren’t always motivated by the same things as you (for example, they might care more about their next lab test results than how they look in a swimsuit)
- Don’t always enjoy—or hate—the same things (just because you love long sessions of steady state cardio, doesn’t mean they will… or vice versa)
- Don’t always share your values (as mentioned above, not all clients value health above all else; they may instead value pleasure, spontaneity, or something else)
Get to know your unique client, their specific goals, and what actions they can realistically execute (and maybe even get excited about).
Coaching mistake #3: Getting too attached to client results
This is, actually, very natural.
“There’s a reason we go into coaching. It’s because we care and we want to help clients. We want to see them succeed,” says Coach Kate.
But caring can be a double-edged sword.
“With our clients, we carefully decide on the habits and behaviors that need to occur… And then they walk off and either do the thing or don’t do the thing. That’s brutal.”
No matter how sound and foolproof your advice is, how well-thought out your plan, how much you care, ultimately, you have no control over whether a client executes it, and gets results.
Naturally, as a coach, you might feel frustrated, even heartbroken when clients don’t do what they say they’ll do, or when they’re not seeing the outcomes they were hoping to see.
However, according to Kate, this isn’t something coaches should try to avoid completely. It’s part of the job, and it’s often a sign that your work has meaning to you. (It’s a good thing.)
“However, I think there’s a point there where we can start caring more than the client themselves,” she says.
And that’s precisely where to draw to the line.
At PN, we often say that “care units” are the currency of coaching.
Care units are how much time, energy, attention, authenticity, and true “heart” you can bring to helping, serving, and caring about your clients.
Your client also has a certain amount of care units.
How much time, energy, attention, authenticity, and “heart” can they bring to their own change and growth projects?
(Most of the time, not that much. Which is totally normal.)
Our advice: Care one care unit less than your client does.
How do you do that? One approach…
Solution: Clearly separate client and coach responsibilities
So, how do we maintain an appropriate level of emotional investment—but also help clients stay on track?
“This is where I really like to get really clear on what my role is as a coach,” Coach Kate says.
“Because if you are very, very clear on what your role is as a coach, then you can sort of go through the list, and check in with yourself: ‘Did I show up? Did I follow up? Did I coach this person to the best of my ability?’”
For example, as a coach, it’s reasonable to be responsible for:
- Providing guidelines for how to reach out (to ask questions or book appointments) as well as setting expectations for your response times
- Weekly check-ins with clients via email, text, or phone, to assess progress or troubleshoot obstacles
- “Life-proofing” a program as much as possible, by proactively discussing obstacles that could arise in the future, and brainstorming realistic, flexible solutions
Meanwhile, the client is responsible for:
- Whether or not they respond to your check-ins
- Whether or not they actually DO the agreed upon fitness, nutrition, or lifestyle practices that are likely to get them to their goal
- How much they reveal during coaching sessions (for example, whether or not they tell you if they’re struggling with stress eating, or some other issue that makes it hard to stick to the plan)
Ideally, clearly delineating these responsibilities should happen early in the coaching relationship. Some coaches prefer to have an open discussion, while others have actual contracts that outline coach deliverables and client expectations.
This early communication can also be a way of vetting coach-client “fit.”
“When I’m having that initial conversation with a prospective client, I can ask, ‘What does accountability look like to you?’ If the client replies, ‘Well, I want you to text me every morning and night, and I want you to make sure I’ve done my workout, and also ship groceries to my house,’ then I will be the one to say, ‘I don’t think this is a good fit.’”
Coach Kate says this kind of early clarity can also prevent coach-client friction in the future.
Clear boundaries and expectations at the outset means clients are less likely to be disappointed if they assumed their coach was going to “take on” more, and coaches are less likely to burn out from shouldering more than they should.
It even protects the coach-client relationship in extreme (though not uncommon) situations such as when a client “ghosts” before a paid contract is over.
“When somebody doesn’t reply to me, I don’t take it personally. It’s not their job to reply, but it is my job to check in,” Coach Kate says.
“If I don’t hear back, I just check in on Monday, and then again on Monday. And again, and again, and again—trying all the contact methods they’ve provided me—until their coaching contract is over. If we get to that point, they’ll get an email from me saying, ‘Hey, I hope everything’s okay. My door is always open. I hope you’re doing well.’”
 Takeaway nugget:
Takeaway nugget:
Make a list—either for your own reference, or to include in a contract that new clients have to sign—of the accountabilities you have as a coach.
(Hint: These are usually specific actions, like “Text, email, or phone once a week to check in” or “Host monthly virtual lectures on various nutrition topics for group clients.”)
Make sure to have a conversation about expectations and responsibilities with all clients, ideally before beginning to work together, or at least in the first session.
Bonus mistake: Forgetting to give yourself a pat on the back
It’s maybe not the most “coach-y” way to write an article: Point out a list of your mistakes, then hand you solutions to deal with them.
But if you’ve made the above “mistakes,” we want you to hear it from us:
We’re proud of you.
If you’ve gotten sidetracked by the above, it’s likely because you really care. And that’s never going to be a mistake; it’s a strength.
That said, although these “mistakes” are completely normal, and most coaches make them, they can limit your potential as a coach, and as a business.
And we want to see you succeed.
(If you liked this article and want to learn more, listen to the full episode of the Coaches Compass podcast, where the interview with Coach Kate Solovieva was originally conducted.)
In our elite mentorship program, you’ll get personal guidance from our industry-leading coaches—and be able to confidently deliver world-class results for clients of all backgrounds, lifestyles, and needs. Join the top 1% of coaches.
“I skyrocketed my coaching skills and confidence…My impostor syndrome is gone!”– Katya Mohsen, PN Certified Master Health Coach
If you’re ready to level up your coaching skills and feel confident you can guide any client to a lasting health transformation, we’ve got some big news for you:
In April 2025, we’ll open registration for the next cohort of the PN Master Health Coaching Certification, the industry’s most respected practice-based mentorship.
“You cannot be a health or fitness coach without having the tools and techniques that this program brings. It’s a whole different level.”– Katya Mohsen, Lisa Bernier, PN Certified Master Health Coach
Inside the Master Health Coaching Certification, you’ll learn a skill set and be able to earn a credential that will distinguish you as an elite coach:
The ability to use behavior change psychology to help any client achieve sustainable, meaningful change. And the credential of being a Board Certified Health and Wellness Coach.
“This program does an absolutely phenomenal job of addressing how to affect behavior change…something that’s sorely missing in most people’s practices.”– Jeb Stuart Johnson, Founder of Food On The Mind, PN Certified Master Health Coach
It’s the only program in the world where you’ll learn the secrets of behavior change psychology through live mentorship.
Because, while knowing the science of nutrition and fitness is important, it’s not enough. In order to actually create change, you need a deep understanding of behavior change psychology.
We’ve applied this understanding with our coaching programs to help over 150,000 clients achieve lasting health transformations—something nobody else can say.
And now, we’re ready to share our hard-earned wisdom with you.
“This program taught me how to be a better coach and retain clients longer. Before, I had clients staying for a month. Now, it’s six, nine months, even a year.”– Jeff Grogan, PN Certified Master Health Coach
Through real-world coaching scenarios, hands-on assignments, and mentoring sessions with PN’s industry-leading Master Health Coaches, you’ll learn how to prioritize a client’s challenges, help them remove obstacles holding them back, and how to create unique, actionable coaching plans for every client, addressing their:
- Sleep
- Stress management
- Mental health
- Emotional wellbeing
- Recovery
- Diet
- Exercise
This mentorship program is where the world’s best coaches come to take the next steps in their careers.
At the end of your 20-week program, you’ll be a Master Health Coach—confident in your ability to guide any client towards a meaningful, lasting health transformation.
“I now have more knowledge, more confidence and more skill. My clients stay longer and experience better results.”– Jonny Landels, Founder of Next Step Nutrition, PN Certified Master Health Coach
After joining, you’ll:
- Help any client achieve sustainable, meaningful change by leveraging behavior-change psychology.
- Eliminate impostor syndrome and feel more confident in your skills than ever before by integrating proven methods used by the world’s top health and well-being coaches into your coaching practice.
- Become an authority in the health and well-being space. As you learn from PN’s industry-leading coaches and network with some of the sharpest minds in the industry, you’ll build the confidence to share your expertise with anyone, anytime.
- Make more money and achieve financial freedom. Whether you decide to take on the full-time role of “health coach”, or you want to expand on your current work as a health and well-being professional, health coaching is a great way to help more people.
Enrollment is currently closed. Doors will open again in April 2025.
If you’re interested, or just want more information, you should strongly consider signing up for the free no-obligation waitlist below.
And by joining the free Waitlist, you’ll get our best price, exclusive perks, and early access when registration opens.
- Pay less than everyone else. Get our biggest discount off the general public price when you sign up for the waitlist.
- Sign up 10 days before the general public. We only open the PN Master Health Coaching Certification a few times per year. Due to high demand, we expect it to sell out fast. But when you sign up for the waitlist, we’ll give you the opportunity to register 10 days before anyone else.
- Receive our free Enrollment Packet—with success stories, details on Board Certification, info on curriculum, and much more
The post Three mistakes health coaches make—and the immediately actionable solutions to fix them appeared first on Precision Nutrition.
Source: Health1
“I just bought a new BPA-free tupperware set.”
This comment, coming from my friend Anna, caught me off guard.
Anna’s a highly competent law professional. She’s a critical thinker and she fights in the heavyweight division when it comes to cutting through BS.
But the Anna I knew was falling into some painful traps that seemed to be bypassing her inner hawk-like skeptic.
She’s wanted to lose around 15lbs for some time now and came to me to share how stuck she was feeling in this goal.
She brought up an avenue she was exploring: the new BPA-free tupperware set.
“Interesting. What inspired you to focus on that?” I asked.
“Well, I’ve been reading about how microplastics in food containers can mess up our hormones and cause weight gain,” she said.
I squinted.
To backtrack, this is right after she told me how she’d been struggling to be consistent at the gym, had been relying on takeout too often, and had been sacrificing boring old sleep for adrenaline-inducing doom scrolling.
So I asked:
“What about trying to get more consistent with your workouts, or prepping more homemade meals during the week?”
And Anna said:
“Yeah, but I’ve tried that a thousand times. If it were that simple, it would have worked already.”
We’ve all done this before.
Ignored or delayed those hard-but-worthwhile habit changes in favor of some ultra-specific, niche magic bullet that’s supposed to “change everything.”
Spent hours of research on the ultimate, most optimal workout instead of devoting those hours to just doing the basic workout you already know how to do.
Waited to feel more inspired, motivated, or just less busy.
Why do we do this?
Buying new gear or a popular supplement feels like making progress.
Consuming YouTube videos or articles about stuff you can change feels like you’re doing something.
And waiting until the “right time” feels, well, right.
Except, nothing actually changes until we take real, consistent action.
We’re clever, us humans. And we’ve come up with lots of sneaky ways to avoid the basic, unsexy, difficult actions we need to take that actually drive change.
In this article, we’ll explore how to take an honest and compassionate look at why you might be distracting yourself from taking impactful action.
You’ll learn:
- What the most impactful health habits actually are
- Three common barriers to making sustainable progress
- A 4-step process you can apply to start taking positive, productive action
- How to keep yourself consistent—and achieve your goals
The stuff you know you should do (but probably aren’t doing consistently)
We all know what those basic, fundamental health habits are:
 Exercising, ideally 30 minutes a day, putting in moderate-to-vigorous amounts of effort, with a mix of aerobic and resistance training.
Exercising, ideally 30 minutes a day, putting in moderate-to-vigorous amounts of effort, with a mix of aerobic and resistance training.
 Eating mostly nutritious, minimally-processed foods. If 80 percent of your diet comes from whole or minimally-processed foods, you’re doing an excellent job. (Translation: “Perfection” isn’t required; pizza can be part of a healthy diet.)
Eating mostly nutritious, minimally-processed foods. If 80 percent of your diet comes from whole or minimally-processed foods, you’re doing an excellent job. (Translation: “Perfection” isn’t required; pizza can be part of a healthy diet.)
 Eating enough protein to support muscle mass, appetite regulation, and body recomposition goals, if you have them. Aim for about 1.2 to 2.2 grams of protein per kilogram of body weight (for most people, this adds up to about 4-6 palm-sized portions of lean protein per day).
Eating enough protein to support muscle mass, appetite regulation, and body recomposition goals, if you have them. Aim for about 1.2 to 2.2 grams of protein per kilogram of body weight (for most people, this adds up to about 4-6 palm-sized portions of lean protein per day).
 Prioritizing getting seven to eight hours of quality sleep. You can’t always control how well you sleep, but having some wind-down time before bed can help, as can waking up at the same time every day.
Prioritizing getting seven to eight hours of quality sleep. You can’t always control how well you sleep, but having some wind-down time before bed can help, as can waking up at the same time every day.
 Avoiding or at least reducing excessive consumption of alcohol or drugs, including cigarettes. No fun, we know. But it’s for a good cause.
Avoiding or at least reducing excessive consumption of alcohol or drugs, including cigarettes. No fun, we know. But it’s for a good cause.
Easily, we could add stuff like prioritizing positive, nurturing social relationships, managing stress, and probably others, but just the above list is uncommonly met.
In fact, only six percent of Americans perform all five of the following basic health behaviors:1
- Meet physical activity recommendations
- Don’t smoke
- Consume alcohol in moderation (or not at all)
- Sleep at least seven hours
- Maintain a “normal” BMI
If you’re doing the math, that means close to 94 percent of Americans aren’t doing the basics.
Yet, these foundational behaviors also help us achieve a long list of common goals, whether that’s reaching a healthy weight, improving athletic ability, or just living a longer, healthier life.
So why do we struggle so much to do them?
Here are three common barriers we see among clients (and coaches!), plus potential solutions to overcome them.
By the way, ambivalence is normal.
That push-and-pull feeling you have when you think about making a change?
It has a name, and it’s called ambivalence.
Ambivalence describes the mix of feelings you have when you contemplate, say, waking up earlier so your mornings are less stressful, or cutting down on TV time.
We naturally and normally feel ambivalence about change—“I want this, and at the same time, that.”
(For example, wanting to eat healthier, and also wanting to have your favorite treats whenever you want without constraint.)
We also naturally and normally feel resistance towards change—“I want this, and at the same time, not.”
(For example, wanting to stop using your phone as a mindless distraction, but not wanting to deal with the anxiety you get whenever you’re left with your own thoughts.)
These contradictory emotions can seem frustrating, puzzling, or “illogical.” Yet, ambivalence and resistance are fundamental parts of the change process.
The higher the stakes of change, the more likely we are to feel a mix of strong and unexpected emotions, pushback, rebellion, angst, and other types of resistance and ambivalence.
Rather than signaling that the change is a wrong move, strong ambivalence and resistance tend to signal that this change matters to us.
In a sense, it’s good news.
It tells us we care.
Basics Barrier #1: You have ambition overload.
Maybe you’ve decided you want to be healthier. So you declare that, starting Monday, you’re going to exercise for an hour everyday and “eat clean” at every meal and sleep eight hours every night.
(Currently, you don’t have a regular exercise habit, don’t particularly like vegetables, and regularly stay up past midnight.)
Now, let’s be honest: You’re asking yourself to change a lot of stuff at once.
And the last time you created an elaborate plan for overhauling your life…
… Did it work?
Probably not.
(And that’s okay.)
When we feel frustrated or stuck in our current situation, making a plan filled with idealistic dreams can provide us temporary relief.
And our brain has several (normal) cognitive biases that prevent us from judging the future accurately.
We often think we’ll have more time, energy, attention, and motivation in the future than we really do.2 3 4 5
There’s a powerful, instantaneous comfort that comes with overloading our future self. (Because after all, we won’t start the plan until Monday.)
The problem with this is:
Big, complex plans often don’t fit into our already busy, complex lives.
We under-estimate how many smaller tasks are hidden in the bigger plans.
When we (almost inevitably) are unable to execute these ambitious goals, we blame ourselves, our personality traits, our “willpower” or “discipline,” and build a pitiable story about how we “struggle with consistency.” Or how living this way is “impossible”.
Then, sadly, we fulfill that prophecy.
Basics Barrier #2: You think only hardcore, “industry-secret,” or “cutting-edge” stuff works.
This barrier comes from the following common belief:
“If getting healthy just took eating, sleeping, and exercising moderately well, then everyone would be healthy.”
Because everyone knows they should eat their vegetables, get seven to eight hours of sleep per night, and stay active, right?
(We’d agree.)
But let’s go back to the previously mentioned statistic:
Only 6 percent of Americans are consistently performing the most basic health and fitness behaviors.
If we add on slightly more advanced—but still very basic—behaviors like eating five servings of fruits and vegetables every day, optimizing protein intake, and effectively managing stress, that number would shrink significantly.
So, the first thing is to believe that these simple behaviors work. Because they do. It’s just that most people (probably close to 99 percent of us) are not doing them all simultaneously and consistently.
The second thing is to accept that these simple behaviors are a little bit boring. Because they are. Part of the reason we’re attracted to new diets or “magical” supplements is because we just want something more interesting to try.
That’s especially true if we’ve already sort of tried the “eat more vegetables” thing and it didn’t “work” for us in the way we expected.
With something new and cutting-edge, there’s also the possibility of a new outcome, a new us.
And of course, that’s incredibly appealing.
Thing is, most hardcore, “industry secret,” or “cutting edge” tools and strategies are, respectively: unsustainable, inaccessible, or ineffective (or unproven).
They’ll take your effort, your time, and often your money, but without giving you a good return on your investment—all the while distracting you from the stuff that actually works.
Basics Barrier #3: You think your efforts (and your results) have to be perfect.
Another lie in the health and fitness industry is that you have to be “perfect” to maintain great health. You know, eat only organic salads and chia seeds, be able to run a marathon, and wake up at 5 am every day to meditate and write in your gratitude journal.
The truth is, perfection definitely isn’t required.
Depending on how you look at this, this could be a relief to hear, or a disappointment.
On the one hand, it’s nice to know that you don’t have to have it “all together” to be healthy—even above-average healthy.
On the other hand, many of us pursue better health with the belief that our optimal or even “perfect” self will one day, with the right plan or routine, be attainable.
But “perfect” health is an illusion.
Humans, even exceptionally healthy ones, get sick, get weird rashes, have digestive problems, need reading glasses, get into slumps, or just otherwise have a series of bad days.
None of us are “safe” from those life events, and accepting that can feel a little… vulnerable.
It’s much more comfortable to believe that if you just take this powdered algae supplement, or follow this specific morning routine, you’ll be immune to any kind of painful human experience.
The irony is, to achieve your realistic “best self,” you probably have to accommodate your “worst self” too. You know, the one who’d rather watch another episode of Love is Blind than work out, or eat a party-size bag of Doritos and call it dinner.
Because life happens.
Work gets busy.
Or your kid goes through a “phase.”
Or it’s pie season.
Any number of obstacles, distractions, and competing demands make it impossible for perfection to be maintained with any kind of consistency.
Which is why we need to let go of the illusion that a “perfect” self exists—the one who always has the energy, will, and option to make the ideal choice—and support what our real self wants and needs.
We’ve got four steps below to help you.
4 steps to start taking effective (and realistic) action
Now that we know what’s potentially getting in the way of taking productive action, here are four steps to get unstuck.
Step #1: Explore the why before the how.
Before you (or a client) start undertaking something you want to change, it’s helpful to understand your deeper motivations first.
Do a little investigating by asking questions like:
- What about this change is important to you?
- How serious or pressing is this for you?
- Why not continue doing what you’re already doing?
You can also go through one of our favorite motivation-mining exercises, The 5 Whys.
When you know why you want to change something, and you’re clear on the consequences of not taking action, you’ll be more likely to feel that deeper, more sustaining push to keep going, even when things get tough.
Step #2: Prioritize the most effective actions.
We can do all the things!! Really!! We just can’t do all the things… all at once.
Effective change means being able to realistically:
- Identify all the tasks, trade-offs, and commitments involved
- Prioritize what matters for the results you want
- Figure out what to do first
What are the essentials in relation to your goal? Regardless of all goals, they likely include a movement practice, a nutrition practice, and/or a recovery practice.
If you want some guidance on how to select the most effective action for your goal, check out our Skills, Practices, and Daily Actions Cheat Sheet.
Here’s how to use it:
 Start with the domain you’re most interested in improving (such as “Nutrition” or “Stress”).
Start with the domain you’re most interested in improving (such as “Nutrition” or “Stress”).
 Then, get specific about what skill within that domain you’d like to improve (for example, “Eat well intuitively”), plus the practice that most appeals to you within that skill (say, “Eat to satisfied”).
Then, get specific about what skill within that domain you’d like to improve (for example, “Eat well intuitively”), plus the practice that most appeals to you within that skill (say, “Eat to satisfied”).
 Lastly, choose a daily action from the list of examples under your chosen practice. (For example, “Record hunger and fullness levels at the start and end of meals.”)
Lastly, choose a daily action from the list of examples under your chosen practice. (For example, “Record hunger and fullness levels at the start and end of meals.”)
Once you choose your action, make it work for you by following step 3, below.
Step #3: Make sure you can take action, even on your worst day.
“I like to challenge a client to set a pathetic goal. If it’s so pathetic, then obviously you can do it, right?” says Kate Solovieva, PN Super Coach and Director of Community Engagement.
Sound inspiring?
Maybe not.
But if you’ve been struggling with consistency, it’s exactly where to start.
Ask yourself:
- What can I do on my absolutely worst day where everything goes wrong? How much time, effort, or enthusiasm will I realistically have?
Five minutes of walking? 10 push-ups? One extra portion of veggies? Three conscious deep breaths before every meal? Nothing is too small; it just has to be something.
Now you’ve got your floor.
Then ask yourself:
- What can I do on my best day, when I feel on top of the world and circumstances are on my side? How much time, effort, or enthusiasm will I realistically have?
One-hour of all-out effort at the gym? Two hours of meal prep that will feed you and your family for the next three days? A 45-minute guided meditation?
This is your ceiling.
Now that you’ve identified your “floor” and your “ceiling,” you’ve defined a flexible range of actions that can adapt to your fluctuating, unpredictable, real life.
But applying this range requires a paradigm shift:
Your health habits aren’t an “on” or “off” switch; they’re on a dial.
When life is sweet and smooth, you can turn your exercise, nutrition, and sleep dials way up—if you want. Bust through your PRs at the gym, eat all the arugula, meditate like a monk.
But if life gets nuts, you don’t have to switch off completely.
Just turn the dial down a little.
The below is a visual representation of how this might work for exercise, but you can apply this same thinking to your nutrition, sleep, stress management, or whatever you’re working on.
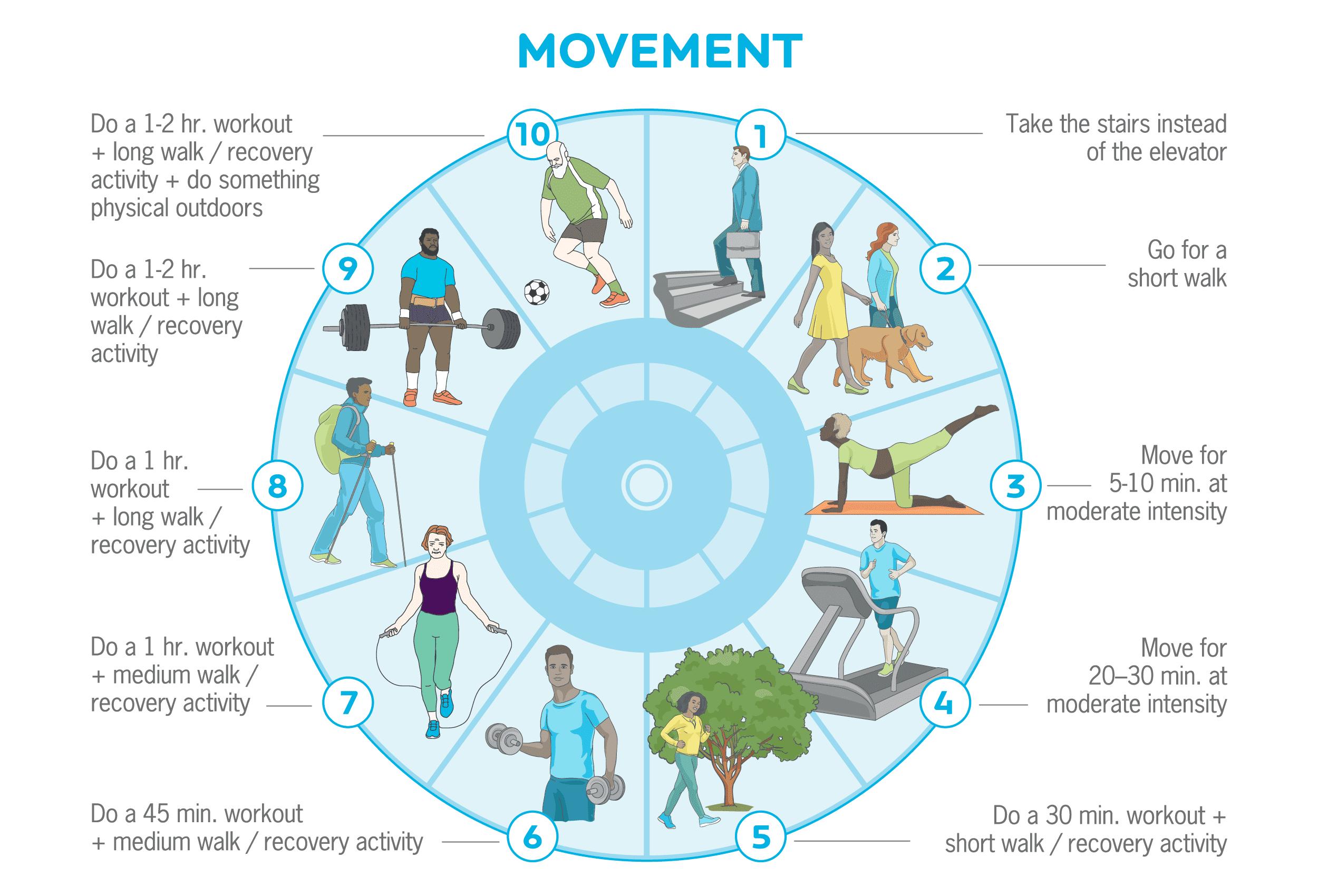
The important part: Even if you do your “floor” or “dial level 1” action—even if it’s for days on end—it still “counts.”
You still get the gold star.
Doing the bare minimum isn’t failing.
It’s succeeding, in the context of a real, messy, beautiful life.
Step #4: Create an ecosystem that supports you.
Health and fitness professionals often forget how different their lives are from their clients.
For example, many coaches work at gyms, enjoy being physically active, and hang out with other active people. Exercising regularly is almost easier to do than not do, because, as Coach Kate says, “they’ve built a life that makes that habit seamless.”
So if you want to make your health goals more likely, Coach Kate offers this advice:
“Build an ecosystem that makes failing nearly impossible.”
When they want to make a change, many people assume that good intentions and willpower will be enough to carry them through. (And when they fail, naturally, they blame themselves for being “bad” or “weak.”)
We often forget about the context and environment that shapes our behaviors—making certain actions more likely or less likely to occur.
A recent review from Nature Reviews Psychology ranked different behavior change strategies and found that access was the number one influencer of people’s behaviors. (People who lived in neighborhoods with affordable grocers close by ate better, just like people who had to drive a long distance to the closest gym were less likely to exercise.6)
Not everyone can change neighborhoods, but most people have some degree of control over their more immediate environments, and can leverage this power to shape desired behaviors.
One example is the “kitchen makeover,” where you make sure foods you want to eat are washed, prepped, and at the front of the fridge, ready to eat on a whim. Meanwhile, foods that don’t support your goals get tossed, or relegated to the highest cupboard. (When you need a stepladder from the basement to reach the cookies, you might find you eat them less.)
(If you want to try it out, check out our Kitchen Set-up Assessment worksheet.)
Think about the goal you want to achieve, and the behaviors that support it. Then, evaluate how you might make small changes to your environment by:
- Using a trigger: Sometimes called a “cue” or a “prompt,” a trigger is simply a reminder to do a desired action. For example, you might block the door of your home office with a kettlebell, reminding you that, every time you leave or enter the office, you have to do ten kettlebell swings. If you’re trying to cut down on mindless phone time, you can install an app that reminds you to shut things down after 20 minutes on social media.
- Decreasing “friction”: Supermarkets put candy next to the checkout, making it easy to slip that chocolate bar into your cart while you’re standing in line, likely bored and hungry. You can be equally sneaky about encouraging positive behaviors too, such as putting fruit on your counter, ready for a quick snack, or packing your gym bag the night before, so it’s ready to grab on your way out the door before you change your mind.
- Constraining available options: Whether it’s deleting time-sucking apps off your phone, removing foods you know you lose control around from your kitchen, or heck, creating a capsule wardrobe so you waste less time in the morning getting dressed, constraint can actually free up a lot of time, brain power, and energy.
Invest your energy building the ecosystem that nudges you to make desired actions the obvious choice. This requires a little more work on the front end, but the payoff will be greater for less overall work.
Embrace C+ effort.
If you’re a perfectionist, or a former straight-A student, that line hurt to read.
(Don’t worry. This C+ won’t result in your parents telling you that they’re disappointed.)
But what all of the above barriers and solutions have in common, is that they recognize and work with our inherent imperfection.
None of us is perfect, and expecting as much often results in failure (or at best, short bursts of success, followed by a crash).
Adopt an attitude of compassion and acceptance towards your human self—who’s most likely trying their hardest—and work with your vulnerabilities, instead of constantly expecting yourself to grit your teeth against them.
There will be times you’re getting “A’s” in fitness. That’s awesome. And you also don’t need to aim for C+. Just don’t think of yourself as a failure when you have to dial it down.
Living a healthy, meaningful life means constantly striving to do our best—while also allowing for flexibility, mistakes, and bad days (or seasons).
You’ll be surprised at how much better “good enough” is than nothing. Especially in the long run.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- Liu, Yong, Janet B. Croft, Anne G. Wheaton, Dafna Kanny, Timothy J. Cunningham, Hua Lu, Stephen Onufrak, Ann M. Malarcher, Kurt J. Greenlund, and Wayne H. Giles. 2016. Clustering of Five Health-Related Behaviors for Chronic Disease Prevention Among Adults, United States, 2013. Preventing Chronic Disease 13 (May): E70.
- Buehler R, Griffin D, Peetz J. Ch 1: The planning fallacy: cognitive, motivational, and social origins. In: Zanna MP, Olson JM, editors. Advances in Experimental Social Psychology. Academic Press; 2010. p. 1–62.
- Kruger J, Evans M. If you don’t want to be late, enumerate: Unpacking reduces the planning fallacy. J Exp Soc Psychol. 2004 Sep 1;40(5):586–98.
- Buehler R, Griffin D, Ross M. Exploring the “planning fallacy”: Why people underestimate their task completion times. J Pers Soc Psychol. 1994;67(3):366–81.
- Buehler R, Griffin D, Ross M. Inside the planning fallacy: The causes and consequences of optimistic time predictions. Heuristics and biases: The psychology of intuitive judgment. 2002;250–70.
- Albarracín D, Fayaz-Farkhad B, Granados Samayoa JA. Determinants of behaviour and their efficacy as targets of behavioural change interventions. Nature Reviews Psychology. 2024 May 3;1–16.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.
The post How to overcome barriers to better health appeared first on Precision Nutrition.
Source: Health1
Reviewed by Helen Kollias, PhD and Brian St. Pierre, MS, RD
At some point in my mid-40s, the scale started climbing.
A pound or two turned into five, then 10, then 20.
It seemed as if I was doing all the right things: Eating less, moving more, rinse, repeat. Yet, the harder I worked, the less the scale seemed to respond.
Had perimenopause destroyed my metabolism?
It sure felt like it.
However, after asking my doctor to run a series of tests, I learned that my metabolism was, in fact, fine. Instead, like the vast majority of midlife women, the true causes of my weight gain stemmed from several subtle issues that I would have sworn, at the time, didn’t apply to me.
If, like me, you or your client are currently stuck in what feels like an eat less, gain more cycle, this article is here to help.
In this story, you’ll discover:
- Several reasons women gain weight at midlife that have nothing to do with a “slower metabolism”
- Why intense exercise and strict diets can backfire after menopause
- 11 crafty ways to get a handle on midlife weight gain
First, what is menopause?
Many women refer to midlife hot flashes and inconsistent menstruation as “being in menopause” or “menopausal.”
However, menopause isn’t a phase as much as a transitional moment that separates menstruation from non-menstruation.
Once you’ve gone 12 consecutive months without a period, you’ve reached menopause. For most people, that moment arrives somewhere between ages 46 and 56.
The hot-and-dewy months and years leading up to that 12th missed period are technically known as “perimenopause.”
Perimenopause means “around menopause.”
Some people refer to this time as the menopause transition. This is when estrogen levels fluctuate. Menstrual cycles lengthen and shorten and, at times, disappear, only to return a few months later. For many people, this marks the beginning of symptoms like hot flashes, sleep issues, vaginal dryness, mood changes, and, yes, creeping weight gain.
(For a thorough overview of the many changes that can happen during this time, read: ‘What’s happening to my body!?’ 6 lifestyle strategies to try after menopause)
How much weight do women gain during menopause?
Many women think of menopause and weight gain the same way many young parents think of two-year-olds and tantrums: Inevitable.
However, not all women gain weight during the menopause transition, explains Helen Kollias, PhD, who is an expert on physiology and molecular biology, and a science advisor at Precision Nutrition and Girls Gone Strong.
On average, in the West, women gain four to six pounds during the three-and-a-half years of perimenopause, or about one to two pounds a year.1 2
That’s double the rate of weight gain in pre-menopausal women, though it’s roughly the same amount men gain at midlife, notes Dr. Kollias.
In other words, the menopause transition may not be solely to blame for those extra pounds on the scale. Aging may play a significant role, as we explore below.
The real reasons the scale climbs
Several factors conspire to add pounds to your frame during the menopause transition.
 You’re not sleeping as well.
You’re not sleeping as well.
Maybe this sounds familiar: You wake repeatedly with sweat pooling under your breasts and sheets that are uncomfortably damp (or soaked).
Even if you don’t have night sweats, plenty of other issues might keep you awake.
First, there’s worry—over aging parents, teenagers with car keys, money needed to replace that leaking roof, some strange bodily sensation you’re worried might be cancer, the colonoscopy or mammogram you don’t want to schedule but also don’t not want to schedule, the sex you’re not having, and so many others.
Plus, if you’re like me and you have osteoarthritis in multiple joints, your body hurts. Or your skin might itch. Or your legs are restless. Or you’re bloated.3 4 5 6
My point: Problems that make sleep uncomfortable can multiply with age.
Because of this, I’ll sometimes wake four or more times a night, as the red sections of this readout from my smartwatch show.
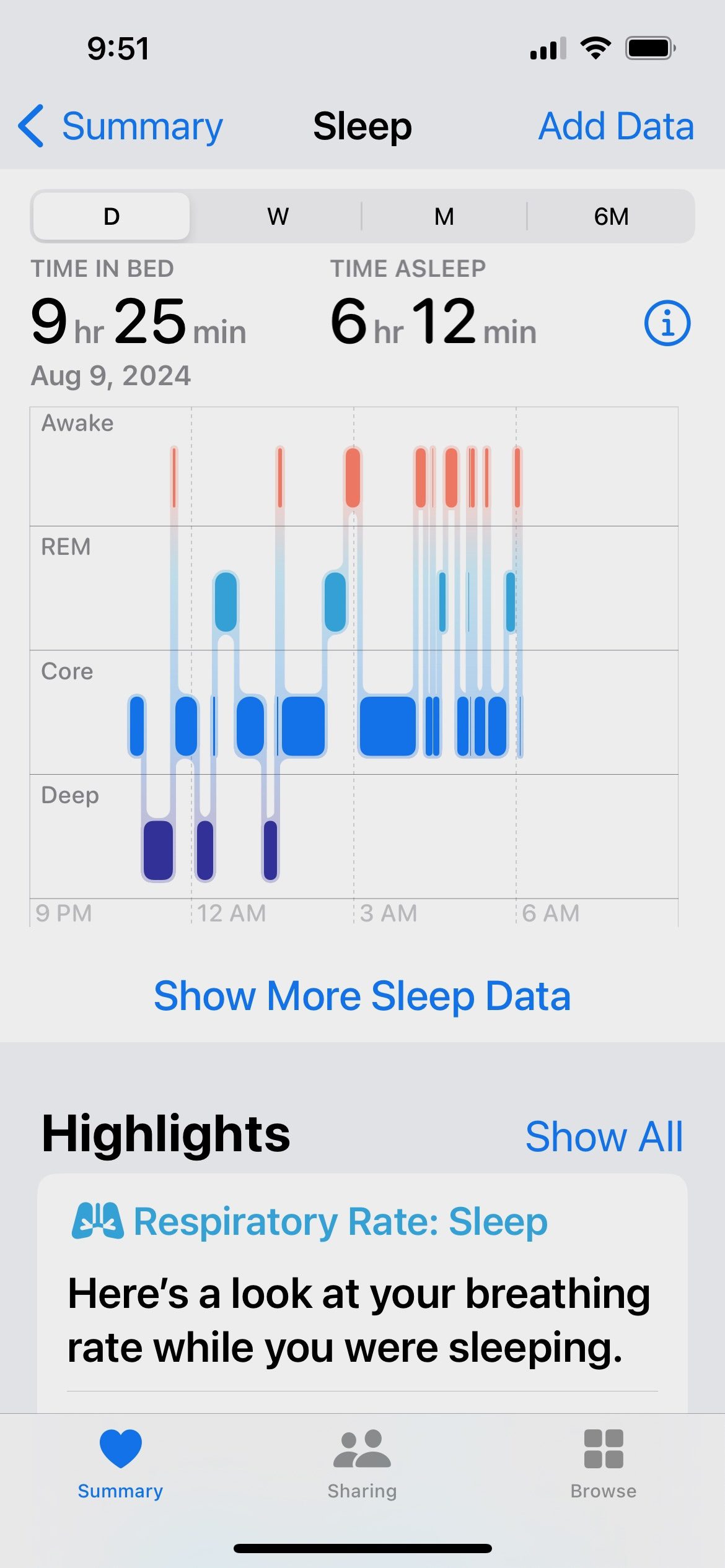
These bad nights often set up a vicious cycle:
The following day, I feel as if I’m two inhales away from death. So, I keep myself going with caffeine, which makes the next night just as bad or worse.
Lack of sleep indirectly adds pounds to your frame in several ways:
- When you’re sleep-deprived, it’s harder to cope with negative emotions, which may mean you turn to food for solace.
- In addition, your decision-making gets compromised, so it’s harder to choose an apple when a chocolate chip cookie is also available.
- Plus, sleep deprivation intensify both appetite and cravings (which we’ll discuss more in the next section)
(Want to get a handle on some of the sleep challenges unique to this transition? Check out: How menopause affects sleep, and what you can do about it)
 You’re hungry, and not for celery.
You’re hungry, and not for celery.
True story: When I was in my early 30s, someone once told me about her intense cravings, and I thought, “Cravings? What are those exactly?”
(Don’t hate me.)
Those days now feel foreign to me. Post-menopause, I spend most of my morning wondering how soon I can eat lunch, what I might have for lunch, whether it’s okay to have a snack now, and, if so, what it should be.
After lunch, I go on to spend the afternoon thinking about dinner.
It’s as if my appetite never flips off.
For the longest time, I thought something was wrong with my brain or metabolism.
It didn’t occur to me that the increased hunger, appetite, and cravings likely stemmed from my repeated awakenings each night.
Until I checked out the research.
In one study, people who were sleep-deprived reported higher levels of hunger and a stronger desire to eat. When provided access to snacks, they consumed twice as much fat compared to days when they weren’t sleep-deprived.7
In another study, when healthy, young study participants slept four hours a night, they consumed 350 more calories the following day.8
The annoying cycle of weight and food preoccupation
Hormonal transitions (puberty, pregnancy, menopause) often cause changes to women’s body shape and size.
Sometimes that’s welcome (“Ooh, a butt!”) and sometimes it’s not (“Darn, a butt!”).
Some women—like me—don’t worry too much about their weight or body shape. Then, we gain unexpected (and unwanted) pounds, and with that, a new (also unwanted) preoccupation with the scale.
Many women also find that as they try to get a handle on the scale, their preoccupation with food may (frustratingly and paradoxically!) shoot upwards—especially if they turn to restrictive diets or food rules for a solution.
Interestingly, this preoccupation with food can occur whether or not someone is actually reducing their calorie intake. In other words, this phenomenon can happen when someone just thinks about reducing their food intake.
The phenomenon has a name: It’s called cognitive dietary restraint (CDR), and it can create a frustrating cycle of body image dissatisfaction, food preoccupation, and stress.
In one study, people who used a low-carb, intermittent fasting protocol to lose weight reported more frequent episodes of binge eating and more intense food cravings.9
In another study, postmenopausal women who scored high in CDR excreted more of the stress hormone cortisol than women who scored lower in this measure.10 Higher levels of CDR in pre- and postmenopausal women were even associated with shorter telomeres, a sign of accelerated aging.11
All this to say, leaning too hard into self-criticism and extreme dieting can backfire. Which is why the strategies we suggest later in this article focus more on adding more nutritious, appetite-regulating foods, and prioritizing things like mindfulness and movement.
With these approaches, you’ll be less likely to feel deprived, and more likely to feel satisfied—and hopefully, empowered.
 You’re moving less.
You’re moving less.
As humans age, we develop chronic low-grade inflammation and weakened immune function. When combined with the crummy sleep we mentioned earlier, along with other biological changes, this can interfere with the body’s ability to recover from intense exercise.
The result: If you do too many vigorous workouts too close together, you’ll start to feel run down, sore, and unmotivated.12 13 14
Other issues that crop up around midlife can also interfere with movement, like chronic injuries or joint pain.
(A personal example: Due to osteoarthritis in my feet and spine, I switched from running to walking. This is easier on my body, but isn’t as efficient at burning calories.)
Finally, due to those pesky time-sucks known as full-time jobs and caregiving responsibilities, you might not be as active in your 40s and 50s as you were during your 20s. Plus, over the past few decades, multiple inventions (hello, binge-watching) have conspired to keep people on the couch and off our feet.
So, can you blame your hormones for anything?
Other than messing with your sleep which, in turn, messes with your appetite and energy levels, fluctuating estrogen and progesterone likely aren’t behind your extra pounds—at least, not directly.
If they were, menopause hormone therapy would help people stop or reverse weight gain. (It doesn’t.15)
However, shifting hormonal levels are responsible for where those extra pounds appear on your body. As estrogen levels drop, body fat tends to migrate away from the thighs and hips and toward the abdomen, even if you don’t gain weight
Old tactics may stop working after menopause
The “Rocky” weight loss method was my go-to when I was younger.
Whenever I wanted to drop a few pounds, I imagined I was a character in one of those “couch potato gets super fit” movies.
In addition to walking and running, I embraced the sweat-til-you-vomit workout du jour. (Remember Tae Bo?) I also cut out foods, food groups, or entire macronutrients. A couple of times a week, I skipped lunch or dinner.
It worked.
Until, of course, it didn’t.
Now, whenever I push too hard in the gym, I either get injured or feel so unbelievably tired that I must take four days off from all forms of movement. If I try to do anything extreme with my diet, I eventually eat every crunchy or sweet thing I can find, including stale crackers.
For these reasons, after midlife and beyond, the countermeasures for weight gain aren’t strict diets (looking at you, intermittent fasting) or barfy workouts.
Instead, to limit weight gain after menopause, you need to get wise about finding ways to tip calorie balance in your favor without triggering overpowering hunger, cravings, and fatigue.
Regardless of age or stage, fundamental nutrition and fitness strategies still apply—and work.
What changes after menopause is how you tackle these fundamentals.
Experiment your way to better results
The best menopause plan will look different for each person.
That’s why experiments are so important.
Precision Nutrition coaches often use experiments to help clients discover essential clues about what they need (and don’t need) to reach their goals. Based on the results you get from each experiment, you can make tiny tweaks, test them, and decide whether they work for you—until you find something that does work for you.
How to run an experiment
Health experiments are no different from the scientific method you learned about in middle school.
- Choose a question to answer, such as, “Would I feel less munchy at night if I ate a protein-rich snack every afternoon?”
- Run an experiment to test your question. In the above example, you’d track your hunger and cravings before adding the snack—to get a baseline—and then continue to track them for a couple weeks after adding the snack.
- Assess what you learned. Did your ratings of hunger and cravings drop? Remain the same? Go up? What about your actual nighttime food consumption? This information can help you determine your next steps.
Below are 11 experiments worth trying during and after menopause. We’ve separated them into three categories: sleep, hunger, and energy.
(And if those 11 options aren’t enough, we’ve got more ideas here: Three diet experiments that can change your eating habits)
Experiments for improved sleep
Below, you’ll find a mere smidge of the many sleep tweaks you can try and test. For more ideas on potential sleep experiments, check out our 14-day-sleep plan and story about cognitive behavior therapy for insomnia.
Experiment #1: Reset your body’s circadian clock
As you age, your body starts to behave like an old clock that continually runs slow.
Even if you used to be a morning person, you might wake groggy, as if your body doesn’t know it’s morning. Or, your body might tell you “time for bed” at weird times, like the middle of the afternoon. Then, after spending several hours fighting the urge to nod off during work meetings, you find that, when it actually is bedtime, you’re staring at the ceiling in the dark.
This is why it’s helpful to experiment with zeitgebers, which are environmental and behavioral time cues that help to set your body’s internal circadian clock.
These experiments might include the following:
- Get up at the same time every day, regardless of how you slept the night before.
- Spend 10-20 minutes in the sunlight as soon as possible after you wake.
- Take a cold shower at the same time each morning or a hot shower or bath at the same time each evening.
- Get outside frequently during the day, especially whenever you feel sleepy.
- Exercise at the same time daily. Try first thing in the morning or 4 to 6 hours before bed. Bonus points if you do it outdoors.
- Eat meals, especially breakfast, at the same time every day.
Experiment #2: Remove “I’m uncomfortable” from your sleep vocabulary
How you run this experiment will depend on what’s causing discomfort. We’ve listed a few possibilities below.
- If you tend to wake feeling uncomfortably hot: Experiment with cooling technology. This might range from the very affordable, such as turning the thermostat a degree or two cooler or using a fan, to the more expensive, such as cooling electric mattress pads.
- If you wake feeling bloated: If you’re constipated, try some prunes, a small daily serving of beans, a little psyllium fiber, or just extra water to get things moving. Or, you might try consuming a smaller meal or avoiding fatty foods in the evening.
- If an uncomfortable “I need to move” sensation creeps into your legs at night: Talk to your doctor about restless legs syndrome, a condition that tends to worsen with age and/or iron deficiency. A physician may also give you ideas to cope if itchy skin or joint pain is keeping you up.
Experiment #3: Time caffeine strategically
We know we’re almost picking a fight with this suggestion. However, it’s worth investigating, especially if you consume caffeine in the afternoon or evening.
If you’re like most people, it will take your body about five hours to clear half the caffeine from your system. That means about half of your 4 p.m. latte is still energizing your system at 9 p.m.
But here’s the thing: Some people metabolize caffeine much more slowly than others, taking roughly twice as long to clear it from their bloodstream.16
Interestingly, even if you had no issues with caffeine when you were younger, you might have issues now, as caffeine clearance tends to slow over time.17
To see if caffeine is a problem, you’ve got a couple of options.
- Try slowly shifting your consumption earlier by 30 to 60 minutes. (If you usually have your last coffee at 4 p.m., cut yourself off at 3 p.m., then 2 p.m., then 1 p.m., then noon.)
- Switch to a lower caffeine source. (Try a bean blend that’s half decaffeinated. Or, you could switch to a lower-caffeine beverage such as green tea or maté.)
(Yet more solutions to common problems: The five top reasons you can’t sleep)
Experiments to reign in hunger
The tactics below likely won’t surprise you. After all, they form the bedrock for solid nutrition and good overall health.
However, before you disregard them with a “been there, done that!” consider: How many of the below are you actually doing consistently?
Experiment #1: Add a protein serving
It may seem counterintuitive to add a serving of food to your meals when you’re trying to eat less.
However, this one tactic may help reign in appetite and hunger.
Protein takes longer to digest than does carbohydrate or fat, so it helps you feel full and satisfied for longer.
In addition, you may find, as I did, that you’re not consuming anywhere near as much protein as you think. (Find out how much you need here: ‘How much protein should I eat?’ Choose the right amount for fat loss, muscle, and health)
Try one or both of the following:
- Consume at least 1 to 2 portions of lean protein at every single meal
- Prioritize snacks that contain protein—hard-boiled eggs, turkey sausage links, Greek yogurt, cottage cheese—instead sweets or chips.
Experiment #2: Choose high-fiber carbohydrates over lower-fiber ones
Fibrous plant foods can help fill you up with fewer calories.
To see the difference, you might monitor how you feel after consuming a near-zero-fiber food, such as your favorite assortment of snack chips. The following day, when it’s time for the same snack or side dish, opt for something with more fiber, such as roasted nuts, a side of beans, a salad, or a piece of fruit. Notice how the fiber-rich option affects your appetite and hunger for the next few hours.
Another experiment worth trying: Include one to two portions of produce with every meal you consume. Track your sensations of hunger to see if they make a dent.
Experiment #3: Log between-meal indulgences
You may be reaching for more snacky foods and beverages than you realize.
These foods don’t need to be 100 percent off-limits; you just want to be intentional about your consumption and portion sizes.
For a couple of weeks, keep track of alcohol, sweets, and treats that you eat between intentional meals and snacks.
Review your notes at the end of each day to see if these more impulsive or less mindful eating episodes align with your memory of what and how much you consumed.
Experiment #4: Move after meals
Increased inflammation coupled with decreased muscle mass, among other factors, leads many people to become more insulin-resistant with age.18 Cells don’t respond as readily to the hormone, which means more glucose stays in the bloodstream rather than entering cells that can use it for energy.
Through a complex set of mechanisms, this can drive up hunger and overall appetite.
Consuming protein- and fiber-rich meals will help, as we mentioned earlier.
So will movement. Walking for as little as two minutes after meals can help your body process the carbohydrates you consumed, improving blood sugar levels, finds research.19 20
In addition, by removing yourself from your kitchen, you create a habit that helps to psychologically shift you away from “eating” and over to “the kitchen is closed.”
Experiments for more energy
To address midlife brain fog and fatigue, you’ll want to do all you can to encourage good sleep. In addition, see if the below suggestions make a difference.
Experiment #1: Prioritize strength training over intense cardio
This was a hard lesson for me because I love intense cardio.
However, now in my 50s, if I try to fit in two weekly strength training sessions and two weekly spin sessions, I feel drugged—as if someone spiked my coffee with tranquilizers.
When my Precision Nutrition health coach suggested I dial back on the cardio for a couple of weeks, I won’t lie. I thought about firing her.
But then I took her advice and rediscovered what it felt like to be alert.
Don’t get me wrong: I still do cardio. But I’m smart about it. I now know that I can’t do everything, at peak intensity, and expect to feel rested and alert daily. There’s a balance.
Strength training is increasingly important at midlife to protect bone strength and maintain muscle mass. Aim for at least two weekly sessions. Then, fit in cardio around those sessions.
If you feel worn out, experiment with doing low- or moderate-intensity cardio (like brisk walking, slow cycling, or swimming) over higher-intensity cardio (like an hour-long spin class).
Or, if you love higher intensities, keep doing them, but shorten your duration.
Or, just save those vigorous sessions for when you got great sleep the night before.
Experiment #2: Try active recovery
Active recovery can help increase blood circulation and the removal of waste products that may have built up in your muscles during intense exercise sessions.21
This can include light activities such as walking, swimming, yoga, or stretching. You can also try massage, foam rolling, or a long, hot bath.
Experiment #3: Consider creatine
Lots of folks think of creatine monohydrate as something people take to get jacked.
However, more and more evidence points to creatine’s benefits for people in midlife and beyond.
The supplement may be especially helpful for muscle recovery.
In research that pooled the data from 23 studies, study participants who took creatine experienced fewer indicators of muscle damage 48 to 90 hours after intense training than participants who didn’t supplement.22
The supplement may also help you to think clearly, especially after a bad night of sleep, finds other research.23
Finally, by promoting cellular energy throughout the body (including the brain), creatine may help to blunt fatigue and boost mood.24 25
A daily dose of three to five grams works for most people.
The winning midlife mindset
There’s one final experiment that I want to tell you about.
It has to do with embracing a mindset of acceptance.
Think back to other difficult phases of your life. For me, parenting an infant with colic comes to mind. Gosh, I was so tired back then that I likely would have forked over my entire 401k in exchange for one solid night of sleep.
However, I knew that the stage was temporary. That knowledge helped to keep me going.
Midlife can be similar.
You likely won’t weigh at 55 what you did at 25. That’s okay. However, the night sweats, brain fog, and fatigue are all fleeting. You will eventually establish a new normal.
In the meantime, see if you can accept that your body may look and feel different now. Shift your focus away from trying to look and feel like your younger self and toward consistently embracing new behaviors that will help you age with strength, vitality, and contentment.
After all, you have much more control over your behavior than the number on the scale.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- Knight MG, Anekwe C, Washington K, Akam EY, Wang E, Stanford FC. Weight regulation in menopause. Menopause. 2021 May 24;28(8):960–5.
- The Royal Australian College of general Practitioners. Australian Family Physician. [cited 2024 Aug 11]. Obesity and weight management at menopause. Available from: https://www.racgp.org.au/afp/2017/june/obesity-and-weight-management-at-menopause/
- National Institute on Aging [Internet]. [cited 2024 Aug 10]. Sleep Problems and Menopause: What Can I Do? Available from: https://www.nia.nih.gov/health/menopause/sleep-problems-and-menopause-what-can-i-do
- Feng J, Luo J, Yang P, Du J, Kim BS, Hu H. Piezo2 channel-Merkel cell signaling modulates the conversion of touch to itch. Science. 2018 May 4;360(6388):530–3.
- Fourzali KM, Yosipovitch G. Management of Itch in the Elderly: A Review. Dermatol Ther. 2019 Dec;9(4):639–53.
- National Institute of Neurological Disorders and Stroke [Internet]. [cited 2024 Aug 10]. Restless Legs Syndrome. Available from: https://www.ninds.nih.gov/health-information/disorders/restless-legs-syndrome
- Hanlon EC, Tasali E, Leproult R, Stuhr KL, Doncheck E, de Wit H, et al. Sleep Restriction Enhances the Daily Rhythm of Circulating Levels of Endocannabinoid 2-Arachidonoylglycerol. Sleep. 2016 Mar 1;39(3):653–64.
- Covassin N, Singh P, McCrady-Spitzer SK, St Louis EK, Calvin AD, Levine JA, et al. Effects of Experimental Sleep Restriction on Energy Intake, Energy Expenditure, and Visceral Obesity. J Am Coll Cardiol. 2022 Apr 5;79(13):1254–65.
- Colombarolli, Maíra Stivaleti, Jônatas de Oliveira, and Táki Athanássios Cordás. 2022. Craving for Carbs: Food Craving and Disordered Eating in Low-Carb Dieters and Its Association with Intermittent Fasting. Eating and Weight Disorders: EWD 27 (8): 3109–17.
- Rideout CA, et al. High Cognitive Dietary Restraint is Associated with Increased Cortisol Excretion in Postmenopausal Women. The Journals of Gerontology. June 2006; 61 (6):628-633
- Kiefer, Amy, Jue Lin, Elizabeth Blackburn, and Elissa Epel. 2008. Dietary Restraint and Telomere Length in Pre- and Postmenopausal Women. Psychosomatic Medicine 70 (8): 845–49.
- Li DCW, Rudloff S, Langer HT, Norman K, Herpich C. Age-Associated Differences in Recovery from Exercise-Induced Muscle Damage. Cells. 2024 Jan 30;13(3).
- Alfaro-Magallanes VM, Benito PJ, Rael B, Barba-Moreno L, Romero-Parra N, Cupeiro R, et al. Menopause Delays the Typical Recovery of Pre-Exercise Hepcidin Levels after High-Intensity Interval Running Exercise in Endurance-Trained Women. Nutrients. 2020 Dec 17;12(12).
- Harvey PJ, O’Donnell E, Picton P, Morris BL, Notarius CF, Floras JS. After-exercise heart rate variability is attenuated in postmenopausal women and unaffected by estrogen therapy. Menopause. 2016 Apr;23(4):390–5.
- Espeland, M. A., M. L. Stefanick, D. Kritz-Silverstein, S. E. Fineberg, M. A. Waclawiw, M. K. James, and G. A. Greendale. 1997. Effect of Postmenopausal Hormone Therapy on Body Weight and Waist and Hip Girths. Postmenopausal Estrogen-Progestin Interventions Study Investigators. The Journal of Clinical Endocrinology and Metabolism 82 (5): 1549–56.
- Institute of Medicine (US) Committee on Military Nutrition Research. Pharmacology of Caffeine. National Academies Press (US); 2001.
- Nehlig A. Interindividual Differences in Caffeine Metabolism and Factors Driving Caffeine Consumption. Pharmacol Rev. 2018 Apr;70(2):384–411.
- Shou J, Chen PJ, Xiao WH. Mechanism of increased risk of insulin resistance in aging skeletal muscle. Diabetol Metab Syndr. 2020 Feb 11;12:14.
- Nygaard H, Tomten SE, Høstmark AT. Slow postmeal walking reduces postprandial glycemia in middle-aged women. Appl Physiol Nutr Metab. 2009 Dec;34(6):1087–92.
- Bellini A, Nicolò A, Bazzucchi I, Sacchetti M. The Effects of Postprandial Walking on the Glucose Response after Meals with Different Characteristics. Nutrients. 2022 Mar 4;14(5).
- Dupuy O, Douzi W, Theurot D, Bosquet L, Dugué B. An Evidence-Based Approach for Choosing Post-exercise Recovery Techniques to Reduce Markers of Muscle Damage, Soreness, Fatigue, and Inflammation: A Systematic Review With Meta-Analysis. Front Physiol. 2018 Apr 26;9:403.
- Doma K, Ramachandran AK, Boullosa D, Connor J. The Paradoxical Effect of Creatine Monohydrate on Muscle Damage Markers: A Systematic Review and Meta-Analysis. Sports Med. 2022 Jul;52(7):1623–45.
- Gordji-Nejad A, Matusch A, Kleedörfer S, Jayeshkumar Patel H, Drzezga A, Elmenhorst D, et al. Single dose creatine improves cognitive performance and induces changes in cerebral high energy phosphates during sleep deprivation. Sci Rep. 2024 Feb 28;14(1):4937.
- Smith-Ryan AE, Cabre HE, Eckerson JM, Candow DG. Creatine Supplementation in Women’s Health: A Lifespan Perspective. Nutrients. 2021 Mar 8;13(3).
- Rae, Caroline, Alison L. Digney, Sally R. McEwan, and Timothy C. Bates. 2003. Oral Creatine Monohydrate Supplementation Improves Brain Performance: A Double-Blind, Placebo-Controlled, Cross-over Trial. Proceedings. Biological Sciences / The Royal Society 270 (1529): 2147–50.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.
The post Weight gain and menopause: It’s not in your head (but it might not be caused by what you think) appeared first on Precision Nutrition.
Source: Health1
Reviewed by Denise Asafu-Adjei, M.D., MPH
A few years back, PN co-founder John Berardi, PhD, posted a shirtless photo of himself on his 47th birthday.
He called it his “anti-regress pic” and thanked 30 years of squats, deadlifts, presses, and chin-ups—among other exercises—for his chiseled six-pack, pumped chest, and bulging biceps.
The question many commenters posed:
“Are you on testosterone?”
Dr. Berardi explained in a follow-up post that while he wasn’t against testosterone replacement therapy (TRT) for people who needed it, he himself was not on this therapy, and his testosterone levels were boringly “normal.” He also offered some thought-provoking ideas about testosterone and aging. Dr. Berardi’s take is the opposite of what you generally hear, especially these days when…
Dr. Berardi’s take is the opposite of what you generally hear, especially these days when…
- The mainstream opinion seems to be that declining testosterone is a harbinger of aging, frailty, and impotence—not to mention a threat to masculinity.
- Increasing numbers of middle-aged men are ditching traditional medical checkups for men’s-focused telehealth clinics that specialize in testosterone enhancement.1
- Reddit communities have popped up solely to obsess over neuroscientist Andrew Huberman’s supplement recommendations for optimizing testosterone.
- Media outlets pump out story after story about “testosterone boosting” foods to eat and “testosterone lowering” foods to avoid.
Whether you’re a coach who fields the “How do I optimize testosterone?” question from clients—or just a regular dude hoping to age well—it’s easy to feel overwhelmed and confused by the conflicting information.
Are declining testosterone levels normal?
Do testosterone-boosting supplement regimens actually work?
Who benefits from testosterone therapy—and who doesn’t?
In this story, we’ll explore those questions and more.
What is testosterone?
Secreted by the testes, testosterone is the sex hormone responsible for male sexual characteristics such as big muscles, deep voices, and hairy chests. It’s a chemical messenger that plays a key role in various processes throughout the body, including sperm production and bone density.
(In women, who also need testosterone to keep various processes humming, testosterone is secreted by the ovaries and adrenal glands. Their bodies just make much less of it; about 10 to 20 times less than men.)
Possibly because of its relationship with muscle growth and sex drive, a lot of cisgender men think of testosterone in binary terms, with lower testosterone being bad and higher testosterone being good.
However, it’s more accurate to think of the relationship between testosterone and health as a continuum that goes from too low (problematic) to too high (also problematic), with the healthy range falling between the two extremes, says Denise Asafu-Adjei, MD, MPH, urologist, men’s health expert, and assistant professor of urology at Loyola University Chicago-Stritch School of Medicine.
As the chart below shows, the dangers of extremely low testosterone are similar to the risks of extremely high amounts (typically only achievable with the use of anabolic steroids).
| Problems associated with extremely LOW testosterone | Problems associated with extremely HIGH testosterone |
|---|---|
|
|
Low testosterone vs. lower testosterone
Testosterone levels naturally ebb with age, with most men losing about 1 to 2 percent annually starting around age 40. By age 75, most men have 30 percent less of the hormone than they did at age 25.2
(Fun fact: Between ages 25 and 80, men can expect their testicles to shrink 15 percent.3)
However, age-related drops in testosterone are not the same thing as “low testosterone.”
Hypogonadism is the medical term for low testosterone levels, and it affects about 35 percent of men older than 45 and 30 to 50 percent of men who have obesity or type 2 diabetes, according to the Endocrine Society, one of the professional public health organizations that sets hypogonadism treatment guidelines.
Not only can overly low testosterone make you feel fatigued and do a serious number on your sex drive, but it can also harm your bone and cardiovascular health, says Dr. Asafu-Adjei.
“You need testosterone for good bone strength,” says Dr. Asafu-Adjei. “As you get older, you’re already dealing with weaker bones, so having lowered testosterone isn’t going to help.”
Alternatively, bringing levels up to normal seems to offer cardiovascular benefits, she says. (The big caveat here is up to normal—not far above it.)
The importance of referring out
What if you or your client have most of the hallmark symptoms of hypogonadism but still have blood levels of testosterone in the normal range?
“Many men over 30 who feel down or low energy will now automatically blame their testosterone,” says Dr. Asafu-Adjei. “Their symptoms might be related to testosterone, but they also could be related to not sleeping, stress, or some other factor.”
That’s why seeing a healthcare professional specializing in men’s health and testosterone management is so important.
Such a physician can screen you or your client for dozens of other problems (like stress and poor sleep) and conditions (like diabetes, obesity, or sleep apnea) that either mimic the symptoms of hypogonadism or interfere with the production or signaling of testosterone.
In other words, supplemental testosterone is the answer for some men with symptoms of hypogonadism, but not all of them. An extensive workup is required.
“There are overlapping symptoms with low testosterone as well as a lot of nuances around hormone treatment,” says Dr. Asafu-Adjei.
“For example, outside of your total testosterone, we also look at your testosterone-to-estrogen ratio and other related hormones. That’s why it’s so important to go to someone who knows what they’re doing. They’ll take a deeper dive to figure out the root of the problem.”
So, if you specialize in coaching middle-aged and older men, get a urologist or endocrinologist in your referral network.
Testosterone and aggression
Many people assume that, in high amounts, testosterone turns men into pushy, road-rage-fueled jerks. However, the association between the hormone and behavior is much more complex.4
As it turns out, both too much and too little testosterone can lead to irritability.
In addition, the link between testosterone and aggression depends a lot on someone’s personality, upbringing, context, social norms, and more.
For example, in one experiment, researchers asked forty young men to play a video game that involved accepting and rejecting offers from a proposer. If someone deemed the proposal too low, they could reject the offer and punish the person for making such a substandard ask. Alternatively, if they considered the offer beneficial, they could accept it as well as reward the person.5
Researchers injected some of the men with testosterone as they played the game.
As expected, players treated with the hormone were more likely to punish proposers, especially if they considered the offer unfair. However, if they perceived the offer as fair, they rewarded the proposer more generously.
The increased testosterone amplified aggression, but also generosity.
Some researchers refer to this phenomenon as “the male warrior hypothesis,” which holds that testosterone may function to help some men protect and cooperate with their “in group” (such as their family, friends, and coworkers) while simultaneously punishing anyone seen as an outsider.6
7 evidence-based ways to optimize testosterone… naturally
On the Internet, if you look for ways to boost testosterone through lifestyle, you’ll quickly become inundated with supplement recommendations and lists of T-boosting and T-harming foods.
However, research-supported ways to optimize testosterone generally center on the fundamental dietary and lifestyle measures you’ve long heard are good for you.
They include the following:
Testosterone optimizer #1: Make sure you’re eating enough.
Your body prioritizes thinking (your brain) and movement (your muscles) above sex (your reproductive organs).
Think about it this way: If there was a famine, the last thing you’d need is another mouth to feed.
So, when you chronically burn more calories than you consume, hormone levels generally drop. (This is true in both men and women.)
“A lot of men in their 20s and 30s come to me about their low testosterone levels and their low testosterone symptoms,” says Dr. Berardi. “These are mostly guys who prioritize exercise. They work out a lot and watch what they eat. In other words, they are men experiencing mid- to long-term negative energy balance.”
Dr. Berardi’s advice is often not what men expect.
If their eating and exercise routines suggest they’re in a chronic negative energy situation, he simply recommends they eat an extra healthy snack or two a day.
“In situations like this, adding a couple hundred extra calories of high-quality protein and carbohydrate often fixes everything,” he says.
Those added calories could come from a couple scoops of whey protein mixed in milk with a nut butter and banana sandwich on the side, he says.
Another favorite snack of Dr. Berardi’s: A bowl of steel-cut oats with protein powder, cacao powder, dates, raw nuts, and nut butter.
Keep in mind: Eating too much (and gaining fat) can also affect testosterone, as we’ll cover soon. Use our FREE nutrition calculator to ensure you’re consuming the right amount of calories and nutrients to support hormone production.
Testosterone optimizer #2: Prioritize sleep.
Testosterone production has its own circadian rhythm: It’s higher in the morning and lower at the end of the day.
As you sleep, levels rise again, peaking during your first segment of rapid eye movement. This may explain why various sleep disorders—including sleep apnea—are associated with testosterone deficiency.7
A handful of small studies have looked at what happens to hormone levels when men skimp on sleep.8 In one of these studies, participants slept just five hours a night for eight days, resulting in a 10 to 15 percent drop in daytime testosterone levels. 9
The right amount of sleep varies from one person to another. However, if you routinely get fewer than seven hours and wake feeling exhausted, it’s a good bet you’re not getting enough. If you wake unrefreshed or struggle to sleep soundly, our 14-day sleep plan can help.
Testosterone optimizer #3: Maintain healthy body fat levels.
Body fat secretes aromatase, an enzyme that can convert some testosterone into estrogen.
According to some research, men categorized as overweight or obese tend to have slightly higher levels of estrogen, as well as the stress hormone cortisol. 10 11
More research is needed to know whether these slightly higher estrogen levels are enough to contribute to hypogonadism.
In the meantime, however, a healthy body composition is vital for overall good health and may also help to optimize testosterone.
Keep in mind, as we said above, that too little body fat can also negatively affect testosterone levels. To ensure your body fat levels are in the optimal zone, use our FREE body fat calculator.
Testosterone optimizer #4: Get moving.
Regular exercise is associated with elevations in testosterone. It can also help you sleep more restfully and keep body fat in check.
Resistance training offers more of a testosterone boost than endurance exercise. (Two to three sessions a week is a great benchmark.)
However, endurance exercise can also help, providing you exercise at the right intensity, finds research. (That’s 30 minutes of rigorous activity, four to five times a week.12)
Overtraining without enough recovery can lead to the opposite effect though, potentially causing gains to plateau and suppressing testosterone.13
(See our FREE exercise library for 400+ expert how-to videos and a 14-day at-home workout program.)
Testosterone optimizer #5: Consume a well-rounded, healthy diet.
In addition to helping you avoid nutrient deficiencies that can drive down testosterone levels, a healthy diet protects your blood vessels.
That’s crucial for getting erections.
A study of 21,469 men found that those who consumed foods consistent with the Mediterranean diet had a lower risk of developing erectile dysfunction over ten years compared to men who didn’t follow the diet.14
“Mediterranean diets are also known to promote heart health,” says Dr. Asafu-Adjei.
The Mediterranean diet emphasizes fruit, vegetables, whole grains, nuts and legumes, and healthy fats from foods like olive oil, eggs, and fatty fish. It de-emphasizes red and processed meat, sugar-sweetened beverages, and sodium.
However, eating patterns that center on minimally processed whole foods likely offer the same benefits.
Many fruits, veggies, and other minimally processed whole foods are rich sources of flavonoids, a plant chemical that helps to improve blood flow and testosterone production.
(This visual eating guide can help you choose the best foods for your body.)
Testosterone optimizer #6: Avoid chronic emotional stress.
When you’re under stress, your body produces cortisol and other hormones that prepare you to fight, flee, or freeze. As these stress hormones flood your body, they suppress the production of reproductive hormones like testosterone.15
This high-cortisol, low-testosterone phenomenon is a likely consequence of millions of years of evolution.
Early humans who were more interested in mating than fleeing from sharp-clawed wild animals didn’t usually live long enough to pass their genes to the next generation.
However, not all short-term stressors dampen testosterone. Some can raise it temporarily, including exam stress or exercise.16
So, aim for the stress sweet spot where you feel energized and engaged with life but not so busy and harried that you have no time to relax, sleep, or enjoy life.
(Learn more: How to tell the difference between good stress and bad stress.)
Testosterone optimizer #7: Prevent zinc deficiency.
As a certified health coach, it’s out of your scope of practice to recommend supplements to treat a condition like hypogonadism.
In addition, the boost someone might get from a supplement pales in comparison to the six pieces of advice above, or to testosterone therapy.
With that important caveat out of the way…
There is a correlation between low zinc intake and low testosterone levels.17 18
However, to benefit from supplementation, someone must truly be deficient in the mineral. Simply topping off someone’s already adequate zinc stores likely won’t lead to a testosterone boost, and may even cause harm.
Checking for and treating a mineral deficiency requires the expertise of someone trained in medical nutrition therapy. If you lack this training, encourage clients with low testosterone to talk to their healthcare professionals about whether a zinc supplement might help.
Use the Deep Health lens
Let’s circle back to Dr. Berardi’s hypothesis, first mentioned at the beginning of this story:
Some evolutionary biologists have indeed theorized that men evolved to have higher testosterone levels when they’re younger (to encourage mating) and lower levels when they’re older (to encourage parenting).19
However, this is more of a theory than a certainty.
What we can say with certainty is this: There’s no one-size-fits-all protocol for healthy testosterone levels.
When testosterone drops after middle age, some men feel lousy.
Even when they do everything right in the lifestyle department—exercising, eating a healthy diet, sleeping enough, and so on—they’re unable to raise testosterone into the normal range. For these men, a healthcare professional, thorough evaluation, and, if warranted, testosterone therapy can be life-changing.
At the same time, plenty of other men continue to thrive well into (and past!) middle age.
Sure, they may be unable to pack on muscle like they used to. But, if they’re paying attention, suggests Dr. Berardi, they might notice other pluses. Maybe they’re more patient, nurturing, and empathetic, for example.
“Don’t get me wrong. I’d be very unhappy with an inappropriate or clinically significant lowering of my hormone levels,” says Dr. Berardi. “However, if I can stay in the normal range and symptom-free with good lifestyle practices, I don’t think I have too much to worry about.”
Dr. Berardi recently turned 50.
“I’m at this stage where I see an interesting fork in the road,” he said.
“Will I gracefully accept aging and see this as a new season—or will I fight against it? I could color my hair, do hair transplants, top up my T levels, and get Botox injections. Or I could accept that there will be some eventual decline and ask, ‘What am I getting in return?’”
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- Hudnall MT, Ambulkar SS, Lai JD, Pham MN, Fantus RJ, Keeter MK, et al. Characteristics of men who use direct-to-consumer men’s health telemedicine services. Int J Impot Res. 2023 Dec;35(8):753–7.
- Decaroli MC, Rochira V. Aging and sex hormones in males. Virulence. 2017 Jul 4;8(5):545–70.
- Barone B, Napolitano L, Abate M, Cirillo L, Reccia P, Passaro F, et al. The Role of Testosterone in the Elderly: What Do We Know? Int J Mol Sci [Internet]. 2022 Mar 24;23(7).
- Geniole SN, Bird BM, McVittie JS, Purcell RB, Archer J, Carré JM. Is testosterone linked to human aggression? A meta-analytic examination of the relationship between baseline, dynamic, and manipulated testosterone on human aggression. Horm Behav. 2020 Jul;123:104644.
- Dreher JC, Dunne S, Pazderska A, Frodl T, Nolan JJ, O’Doherty JP. Testosterone causes both prosocial and antisocial status-enhancing behaviors in human males. Proc Natl Acad Sci U S A. 2016 Oct 11;113(41):11633–8.
- Muñoz-Reyes JA, Polo P, Valenzuela N, Pavez P, Ramírez-Herrera O, Figueroa O, et al. The Male Warrior Hypothesis: Testosterone-related Cooperation and Aggression in the Context of Intergroup Conflict. Sci Rep. 2020 Jan 15;10(1):375.
- Agrawal P, Singh SM, Able C, Kohn TP, Herati AS. Sleep disorders are associated with testosterone deficiency and erectile dysfunction—a U.S. claims database analysis. Int J Impot Res. 2022 Dec 6;36(1):78–82.
- Su L, Zhang SZ, Zhu J, Wu J, Jiao YZ. Effect of partial and total sleep deprivation on serum testosterone in healthy males: a systematic review and meta-analysis. Sleep Med. 2021 Dec;88:267–73.
- Leproult R, Van Cauter E. Effect of 1 week of sleep restriction on testosterone levels in young healthy men. JAMA. 2011 Jun 1;305(21):2173–4.
- Stárka L, Hill M, Pospíšilová H, Dušková M. Estradiol, obesity and hypogonadism. Physiol Res. 2020 Sep 30;69(Suppl 2):S273–8.
- Wrzosek M, Woźniak J, Włodarek D. The causes of adverse changes of testosterone levels in men. Expert Rev Endocrinol Metab. 2020 Sep;15(5):355–62.
- Riachy R, McKinney K, Tuvdendorj DR. Various Factors May Modulate the Effect of Exercise on Testosterone Levels in Men. J Funct Morphol Kinesiol [Internet]. 2020 Nov 7;5(4).
- Hackney AC. Hypogonadism in Exercising Males: Dysfunction or Adaptive-Regulatory Adjustment? Front Endocrinol. 2020 Jan 31;11:11.
- Bauer SR, Breyer BN, Stampfer MJ, Rimm EB, Giovannucci EL, Kenfield SA. Association of Diet With Erectile Dysfunction Among Men in the Health Professionals Follow-up Study. JAMA Netw Open. 2020 Nov 2;3(11):e2021701.
- Khan SU, Jannat S, Shaukat H, Unab S, Tanzeela, Akram M, et al. Stress Induced Cortisol Release Depresses The Secretion of Testosterone in Patients With Type 2 Diabetes Mellitus. Clin Med Insights Endocrinol Diabetes. 2023 Jan 3;16:11795514221145841.
- Afrisham R, Sadegh-Nejadi S, SoliemaniFar O, Kooti W, Ashtary-Larky D, Alamiri F, et al. Salivary Testosterone Levels Under Psychological Stress and Its Relationship with Rumination and Five Personality Traits in Medical Students. Psychiatry Investig. 2016 Nov;13(6):637–43.
- Te L, Liu J, Ma J, Wang S. Correlation between serum zinc and testosterone: A systematic review. J Trace Elem Med Biol. 2023 Mar;76:127124.
- Hunt CD, Johnson PE, Herbel J, Mullen LK. Effects of dietary zinc depletion on seminal volume and zinc loss, serum testosterone concentrations, and sperm morphology in young men. Am J Clin Nutr. 1992 Jul;56(1):148–57.
- Gray PB. The descent of a man’s testosterone. Proc Natl Acad Sci U S A. 2011 Sep 27;108(39):16141–2.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.
The post The REAL way to optimize testosterone appeared first on Precision Nutrition.
Source: Health1
I was 13 when I went on my first diet.
I had been struggling with my weight for about six years, and my obsession with how I looked was starting to dominate my life.
I only had two to three shirts that I felt comfortable in. The only thing that mattered was that they didn’t make me “feel fat.” Even those chosen shirts were always under my West 49 sweater, for extra coverage.
The cherry on top of this presentation was my slouched shoulders—a defense mechanism to protect against exposing my “man boobs,” the body part that had dynastic reign for being my biggest insecurity.
The way I viewed my body governed my self-worth.
I felt that my body held me back from enjoying countless moments of my life, and by the ripe age of 13, I decided I was sick of it.
I figured the only way I could change this purgatory was by changing my body.
I started exercising three to four times a day. For my first two meals a day, I drank a sludge of water mixed with “weight loss smoothie powder” (really just a glorified protein shake). Whenever I “cheated,” I punished myself the next day by eating even less or exercising even more.
In about 5 months, I lost 60 lbs. One third of my body weight to be exact.
This was how I spent the summer transitioning from elementary school to high school. Counting calories over making memories.
To no surprise, this was met with endless praise. And it felt good. Scratch that, it felt incredible.
I had experienced both sides now: One where I felt valueless because I was in a fatter body, and one where I felt accepted and prized because I was in a thinner body.
In another version of this story, I might’ve learned something from my newly widened perspective: I might’ve gained empathy, seeing the unfair stigma projected at people in larger bodies. I might’ve gained bravery, advocating for more body acceptance, regardless of someone’s size.
But instead, I participated in the problem.
I built up the identity of being a “former fat person” who is proof that “anybody can lose weight.”
However, as this script typically goes, over the next few years, I gained a lot of the weight back.
This sent me into a depression. I felt like I had lost my value; like I had won the lottery and blew through my fortune.
That was the pattern I repeated for almost 15 years.
Until I stumbled on something called “body neutrality.”
For me, adopting a more body-neutral approach created a paradigm shift—it offered a way to uncouple my appearance with my happiness. It also caused me to ask some deep questions about my body, and the kind of life I wanted.
Questions like:
“Do I want my self worth to be defined by my external appearance?”
“Do I want to continue this cycle—and potentially pass it on to any future kids I might have?”
“What would my life look like if I fought to value myself for who I am as opposed to what I look like?”
My answers weren’t immediately clear. But body neutrality created an opportunity to step off the hamster wheel of chasing aesthetic goals—and finally, truly reflect.
In this article, I’ll walk you through the process of adopting a more body neutral approach to your own self image and self-care.
You’ll learn:
- What body neutrality is
- How to think about your body and your health—in a way that isn’t dependent on appearance
- Five actionable, body neutral strategies you can apply today—if you want to stop letting your weight, size, or shape dictate your happiness
Let’s begin.
What is body neutrality?
Body neutrality is a mindset that encourages you to value how your body functions and feels over how it looks. This perspective helps you develop self-acceptance, while still working to care for yourself in ways that promote overall health.
In practice, this looks like:
 You exercise and eat nutritiously—not because it makes you look a certain way—but because it makes you feel good.
You exercise and eat nutritiously—not because it makes you look a certain way—but because it makes you feel good.
 You still have treats (because life is too short to be deprived of pizza!) but you don’t eat them to excess because they don’t make you feel the best, physically.
You still have treats (because life is too short to be deprived of pizza!) but you don’t eat them to excess because they don’t make you feel the best, physically.
 You wear clothes and celebrate your appearance in ways that feel authentic, but how you “display” yourself isn’t the foundation of your self-worth.
You wear clothes and celebrate your appearance in ways that feel authentic, but how you “display” yourself isn’t the foundation of your self-worth.
 You don’t always love all aspects of your body, but you don’t let that stop you from enjoying your life; Improving your appearance doesn’t “earn” you the right to be happy.
You don’t always love all aspects of your body, but you don’t let that stop you from enjoying your life; Improving your appearance doesn’t “earn” you the right to be happy.
 You might still care about how you look, but you broaden your self-concept so it also includes your values and your inherent worthiness as a human.
You might still care about how you look, but you broaden your self-concept so it also includes your values and your inherent worthiness as a human.
I value seeing friends and family. I value playing rec sports. I value new experiences.
When I’ve been heavier, I’ve neglected these things in favor of isolating myself.
“I’ll do them again when I lose weight” is something I’ve uttered to myself more times than I can count.
Body neutrality helped me realize I still deserved these things—no matter how I looked.
Everyone can benefit from body neutrality.
Body neutrality isn’t just for people in larger, or otherwise marginalized bodies.
It’s also useful for people with “ideal bodies,” who’ve been the recipients of validation and privilege because of the way they look.
“I’ve worked with clients who are fairly satisfied with their appearance, but they still struggle with their body image because their self-worth relies on it,” says Shannon Beer, registered nutritionist and body image coach.
People with idealized bodies sometimes aren’t living the life they want either, because they have to exhaust their energy to maintain an image of “perfection.”
(If you want to know what kind of sacrifices it takes to meet those “ideal” standards, check out: The cost of getting lean: Is it really worth the trade-off?)
“The ‘meh’ is the magic.”
That’s a quote from Jessi Kneeland, body neutrality coach and author of Body Neutral: A Revolutionary Guide to Overcoming Body Image Issues, when they sat down with some PN coaches to talk about body-neutrality.
(Want to listen in on the whole conversation? Watch it here: PN Coaches discuss body neutrality and negative self-talk)
The goal with body neutrality isn’t to love your body and all of its parts all of the time. Nor is it to be so toxically positive that you ignore real—and sometimes negative—feelings about your body.
That just isn’t realistic for most people.
Instead, an underrated goal is to feel sort of… meh.
You’re not overly glorifying or criticizing your body; its appearance just doesn’t hold that much importance.
In practice, you may love certain parts about your body—but also feel ambivalent or mildly negative about other parts.
For example, you may see your stomach and feel ashamed because you don’t like what you see.
This feeling is uncomfortable, but it’s not “right” or “wrong.” You just don’t want that feeling to dictate your behavior. (Such as seeing your stomach and then saying, “Alright, I’m not going out tonight,” or, “Diet starts tomorrow!”)
To give you a personal example:
As a dude living in North America, I feel pretty ‘meh’ about being 5’9” tall.
Would I love to be 6’2”?
Sure.
But I’m not 6’2”—and I can’t change that. My height won’t ruin my day and I surely won’t be depriving myself from the things I enjoy most in this life because of it.
Body neutrality and aesthetic goals
Some people worry that if they adopt a more body neutral approach to their health and fitness, it means they have to relinquish any desire for physical change.
They also might worry that being more body neutral might make them lose certain aspects of their appearance that they like (such as muscular legs or a slim torso).
Here’s the thing: Body neutrality advocates for health.
Being body neutral doesn’t mean your body can’t change.
It just means your self-worth isn’t dependent on that change, and that your whole life isn’t consumed by the pursuit of a physique goal.
If you’ve been starving yourself and overexercising to the point of burnout, body neutral principles will encourage you to disengage from those extreme activities in the pursuit of a specific physique.
If you’ve been overeating and avoiding exercise because you can’t stand your body, body neutral principles will encourage you to tune into your genuine sense of care and love for yourself, and help you choose food and movement that support your body—regardless of its shape.
In this sense, body neutrality can have a balancing effect on health and fitness behaviors, and, according to Beer, is unlikely to take away from physical health, if applied correctly.
Plus…
There’s nothing inherently wrong with having an aesthetic goal.
Body neutrality rejects physical or aesthetic change only if it’s to the detriment of your overall mental, emotional, social, physical, and existential health.
5 things you can do today to be more body neutral
Congratulations: Just setting the intention to step away from an appearance-centric approach to health and fitness is a great start.
But, ultimately, it’s only action that creates deep, lasting change.
So, here are five tangible strategies you can work on immediately to develop a more body neutral approach.
Strategy #1: Do the things you love today.
Stop waiting to achieve the “ideal” body in order to be able to enjoy your life, and start doing more of what you love now.
Start with something easy that you tend to stop yourself from doing when you feel insecure about your appearance.
When I was in my worst spots, I stayed inside too much—even though I love being outside. It might sound silly but even reading outdoors in nice weather was helpful for me.
The point is: It can be that small.
Find one thing you’ve deprived yourself of in the past and do it—even if it’s a small dose, regardless of how you feel. Re-teach yourself that you don’t need a certain body shape or size to allow joy into your life.
(If you want more ideas on how to stop thinking you’re simply [insert thing you think you need] away from being happy, check out: “I’ll be happier when I lose weight” is a recipe for regret. Here’s the counterintuitive solution)
Strategy #2: Set body-neutral goals.
This is a gamechanger in my coaching experience. I’ve seen clients transform their relationship with exercise when they focus more on what they can do as opposed to how they look. “I feel so much better but I haven’t lost any weight,” is a sentence I’ve heard repeatedly.
When you’re overly appearance-centered or focused on weight, you risk missing other indicators of progress—like how good you feel.
If your fitness goals tend to be aesthetic-centric, try setting a goal that has nothing to do with how you look.
This can look like:
 Setting strength and performance goals in fitness (such as beating a deadlift PR, or a sprint time)
Setting strength and performance goals in fitness (such as beating a deadlift PR, or a sprint time)
 Practicing slow, mindful eating at more meals (if you usually inhale your meals in seven minutes tops, see if you can make a meal last 20 minutes, chewing your food well and savoring each bite)
Practicing slow, mindful eating at more meals (if you usually inhale your meals in seven minutes tops, see if you can make a meal last 20 minutes, chewing your food well and savoring each bite)
 Working to develop a new a skill in the gym (like your first pull-up, or a cool Olympic lift, like a clean and jerk)
Working to develop a new a skill in the gym (like your first pull-up, or a cool Olympic lift, like a clean and jerk)
None of these depend on your appearance; They’re all focused on what you can do. (And chances are, you’ll feel more empowered than ever when you start achieving them.)
Strategy #3: Curate your environment.
Take control of the parts of your environment that feed the body-image obsessed wolf. Starve that beast wherever you can.
Here are some ideas:
 Unfollow social media accounts that prey on insecurity or promote unrealistic ideals. Follow more that are body-neutral, or inspire other aspects of your personality (like comedy, or crafting).
Unfollow social media accounts that prey on insecurity or promote unrealistic ideals. Follow more that are body-neutral, or inspire other aspects of your personality (like comedy, or crafting).
 See what it’s like to reduce your exposure to your own appearance. This can look like having fewer mirrors (or covering some up for a period of time), or turning off the self-view on Zoom.
See what it’s like to reduce your exposure to your own appearance. This can look like having fewer mirrors (or covering some up for a period of time), or turning off the self-view on Zoom.
 Consider ditching the scale. Most people struggle to stay “neutral” about whatever number that shows up.
Consider ditching the scale. Most people struggle to stay “neutral” about whatever number that shows up.
 Set boundaries around body talk. Some environments are rife with commentary about body hang ups or goals. If someone begins talking about their new weight loss diet or “disgusting gut,” try changing the topic, or just exit the conversation. Eventually, people will realize you’re not the right audience.
Set boundaries around body talk. Some environments are rife with commentary about body hang ups or goals. If someone begins talking about their new weight loss diet or “disgusting gut,” try changing the topic, or just exit the conversation. Eventually, people will realize you’re not the right audience.
Strategy #4: Find your people.
Body neutrality won’t be the most common approach you’ll run into in the fitness world.
But, intentionally seeking out and surrounding yourself with more body neutral folks can keep you from constantly getting sucked back into an appearance-centric mindset.
There are body neutral, body positive, or HAES (health at every size) community groups all over social media and the internet, and this can be parlayed into finding local groups near you too.
Seeking out these spaces will only provide more support—and positive momentum—as you pursue a more body neutral approach.
Strategy #5: Strive for improvement, not perfection.
You don’t need to be a body-neutral icon or master. The expectation is not that you 100 percent divest from focusing on your appearance.
Body neutrality exists on a continuum.
Assess where you are right now in terms of how appearance-centric you are when it comes to health and fitness. If all your eggs are in the “aesthetics basket,” then even taking one metaphorical egg out (and say, putting it in the “gardening” basket) is progress.
Use the list of suggestions above to set some small goals, and just begin where you can.
You might always care about your appearance (maybe even more than average), but if it’s progress from where you started, you’re winning.
What life on “the other side” looks like
Even after sharing all of this, I won’t sit here and lie to you by saying I’m pure-bred body-neutral, all the time.
But I like to think I’ve grown a lot since my days of hiding out inside during “fat days.”
I’m better at doing the things I love, even when I don’t feel confident in my body.
I’m better at wearing comfortable clothing when I don’t feel good about my body— instead of cramming myself into something that’s too tight and suffering all day.
And, I’ve expanded the way I see fitness for myself and my clients, focusing more on feel and function, rather than achieving a certain look.
For me, this is progress.
Yours might look different.
Be kind to yourself, and acknowledge that you might be working through decades of programming. Body neutrality sure isn’t a quick fix, but the lasting freedom, joy, and genuine sense of self-worth it offers is worth it.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.
The post Too focused on how you look? Body neutrality might be your key to body image freedom appeared first on Precision Nutrition.
Source: Health1
Everyone needs a team.
As a health coach, you can become an expert in multiple areas: nutrition, behavior change psychology, fitness and athletic performance, stress management and recovery, and more.
However, no matter how many certifications you earn, you’ll invariably encounter clients with progress-blocking problems you don’t have the skills, training, expertise, or legal right to solve.
Here’s the thing…
You may not be an expert at fixing marriages, treating GERD, or counseling someone with an eating disorder, but someone else is.
Here’s where a healthy referral network comes in.
By connecting your client with such a person, you get to stay within your scope of practice, give welcome business to respected colleagues, and help your client solve their problem.
(Total. Supercoach. Move.)
All of our certification programs include sections devoted to teaching coaches how to build robust referral networks of professionals skilled at solving common client problems.
In this article, we’ll discuss how to do that—by exploring the top mistakes we see coaches make. Avoid them, and you’ll be able to refer out with confidence.
First, what’s a referral network?
A referral network is a list of supplementary professionals, businesses, and resources that benefit clients.
Your network might include local or virtual:
- Medical doctors, psychologists, registered dietitians, and other professionals with the training and credentials to help clients with problems outside of your scope of practice. (For an in-depth refresher, see our Scope of Practice worksheet.)
- Fellow health coaches and personal trainers with deep knowledge in an area outside your experience. (For example, maybe a client is interested in learning yoga, but you haven’t the faintest idea of how to salute the sun.)
- Workshops, fitness groups, webinars, food services, and other resources that support clients during their behavior change journey.
To confidently refer clients to skilled practitioners with excellent reputations, you’ll want to do some legwork. That brings us to the top mistakes to avoid.
Mistake #1: You build your network before launching your business.
For recently certified health coaches, the task “create a referral network” can double as a procrastination tool, says PN’s Director of Community Engagement Kate Solovieva.
Rather than take on clients, these coaches search for an increasing number of professionals, valiantly trying to be prepared for every potential referral situation. Yet, as much as they continue to work on it, their list is never “complete.”
That’s because…
“We can’t be prepared for everything,” says Solovieva.
The solution
Take on clients as soon as you’re certified.
Yes! That might sound scary, but the best way to figure out your “gaps” is to begin your practice, and see where your clients actually need help beyond what you can offer.
Add folks to your referral network over time as you:
- Connect with professionals on LinkedIn and other virtual networking sites
- Lean into peer networks (such as the Precision Nutrition Facebook communities)
- Mingle with members of your local Chamber of Commerce
- Chat with family, friends, and clients about professionals and resources they love
- Attend health conventions and other local events where a variety of health professionals tend to congregate
- Search for (and try out!) providers based on your own health needs
Who belongs in your referral network?
Use the following resource list as inspiration.
| Resource | Name | Website | Contact information |
| Acupuncturist | |||
| Chiropractor | |||
| Cooking class | |||
| Cycling, hiking, walking, or running club | |||
| Exercise physiologist | |||
| Coach who specializes in plant-based diets / pre- or post-natal fitness / other coaching niche you don’t cater to | |||
| Marriage / family counselor | |||
| Massage therapist | |||
| Meal delivery service | |||
| Mental health professional | |||
| Orthopedist | |||
| Pelvic floor therapist | |||
| Primary care physician | |||
| Physiotherapist | |||
| Registered dietitian | |||
| Stress management class | |||
| Other |
Mistake #2: You assume your referral list will cover all client needs.
As we mentioned above, you’ll never be able to anticipate every referral or client question ahead of time—and that’s okay.
This is especially true if you coach virtually with clients worldwide.
(You might know three fantastic massage therapists where you live in Toronto, Canada, but that knowledge won’t help if your client is based in Wellington, New Zealand.)
Similarly, some professionals or resources might work for some clients, but not others.
(You might, for example, know of several meal delivery options, yet none are suitable for that plant-based client who’s on a strict gluten-free diet.)
The solution
Learn how to help clients find the professionals and resources they need.
You might:
- Ask clients to describe their preferences. (Do they prefer working with a specific gender? Do they want to meet in person or online? Do they like the eagerness and creativity of a newer professional, or the “I’ve seen it all” sageness of a more seasoned pro?)
- Devote a coaching session to searching online for potential professionals and services together.
- Encourage clients to contact three practitioners, ask questions, and use what they learn to pick a winner.
Mistake #3: You let social awkwardness derail networking opportunities.
Reaching out to a stranger requires some bravery. You have to put yourself out there, explain who you are and what your motives are, and risk being ignored or turned down.
This is where many coaches get stuck, says Toni Bauer, PN’s Director of Coaching and Education Operations.
As a result, many coaches may put off the conversation.
The solution
Turn networking into a challenge. Coach Solovieva calls it “Operation 100.”
- Set a goal to contact 100 professionals over 12 months.
- Work toward your goal every week for about 20 minutes.
- Follow up with each non-responder once or twice.
- Instead of expecting a “yes” from every person you approach, understand that only about 10 percent of people will get back to you.
To ease yourself into the challenge, draft your elevator pitch, suggests Bauer.
Don’t overthink this. Your pitch doesn’t have to be a multi-page persuasive essay. Nor does it have to contain magical talking points. Just be yourself.
The elevator pitch: How to introduce yourself to a potential referral
As you work on your elevator pitch, use the examples below for inspiration.
“I’m a health coach who works with corporate executives. However, some of my clients would benefit from someone with your expertise. I would like to recommend you to my clients as those needs arise. Are you open to that?”
Or:
“I’m a health coach who works with athletes. Occasionally, my clients need guidance that I can’t always provide. I admire the work you’re doing, and I’d love to be able to refer people to you. If you’re open to that, could we have a quick 15- or 20-minute meeting to discuss what that arrangement would look like?”
Or simply:
“I’m a health coach and I’m building a referral list of practitioners. I would love to refer clients to you. Are you taking new patients right now?”
Mistake #4: You use dated persuasion tactics.
If you use LinkedIn, then you’ve likely been on the receiving end of old-school cold sales tactics. We’re talking direct messages from strangers who clearly haven’t read anything on your profile and know nothing about you.
These spammy messages are as welcome as a stranger who sidles up to you at a bar and says, “So, wanna come back to my place?”
We’re not here to discourage you from using cold outreach. It has a place. However, to increase your response rate, we’d like to introduce you to a rarely used technique.
The solution
Get to know people before making an online ask, suggests Coach Solovieva.
Follow them, read their content, download and consume their free resources, comment on their posts, congratulate them on career wins, and become a part of their online life.
Do that, and people will remember you. More of them will respond to your messages, too. Plus, the intel you gather by forming a relationship will help you avoid…
Mistake #5: You don’t personally vet referrals.
How do you ensure you refer clients to compassionate professionals who truly know what they’re doing?
It involves more than checking someone’s website or social media profile.
If you only look at someone’s website or social media posts, “You’re just vetting their confidence and copywriting skills,” says Solovieva. “If we’re fortunate, confidence and copywriting go hand in hand with ability, but not always.”
The solution
Try out their services. Take someone’s yoga or Zumba class. Book a massage. Ask a medical professional to look at your creaky knee.
That way, you can see the professional in action.
If you’re thinking, ‘I don’t need some of the services my clients need!’ you’ve got a couple of options:
- Offer to pay a professional to meet with you for 30 to 60 minutes so you can ask some questions, get a sense of their treatment philosophy, and chat about referring clients to them.
- Interact with people in local social networking communities like NextDoor.com. Ask group members if they’ve seen a practitioner and, if so, whether they’d recommend the person.
Mistake #6: You sell clients too hard on your referrals.
When you recommend a professional you’ve personally vetted, it’s natural to want your client to take action.
However, despite your hard work, some clients just won’t make an appointment with the professional in question—and that’s okay.
“Let your clients be adults,” says Coach Bauer.
Clients have their reasons. Maybe their insurance won’t cover the service in question. Or, maybe they decided to see someone else.
“It’s not your responsibility for the relationships to be perfect or to flourish,“ says Bauer.
A cycle of support
Some coaches fear referrals because they see them as “giving business away.”
In reality, however, when you refer clients to solid pros, your clients simply feel like you have their back. (Which means they’ll be more likely to refer friends and family to you.)
Plus, when you send business towards another respected colleague, it also puts you on their radar for a cross-referral.
It’s good for your clients, good for business, and good for your community of health pros at large.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.
The post How to build a referral network with confidence appeared first on Precision Nutrition.
Source: Health1
There’s been a growing shift in the fitness, health, and wellness industry.
The promise of “immediate results” will probably never lose its sparkle.
But, as a good portion of our population (hi, Boomers!) moves into their “silver” years, conversations around optimizing lifespan (how long you live) and healthspan (how long you live with a high quality of life) are also on the rise.
People are more interested than ever in longevity, which, these days, means the combination of a long lifespan and a long healthspan. (Historically, longevity and lifespan were synonymous.)
Trending too is the concept of biological age—essentially, how “old” your cells are, determined by their health and functioning. (Compare this to chronological age, which just refers to how many years you’ve been on this planet.)
Increasingly, people want to improve their overall health—for the long haul.
Of course, the wellness market is responding to this trend with supplements, ultra-specific diet plans, I.V. therapy, cold plunges, and other fringe modalities that promise to reduce or slow biological aging.
While some of these therapies are questionable, the movement that inspired them is great; For many of us in the health and fitness industry, the shift toward holistic health and long-term wellbeing is a welcome one.
At PN, we’ve held and promoted this expanded view of health for a while now.
We call it Deep Health
Deep Health is a “whole-person, whole-life” phenomenon that involves thriving in all dimensions of the human experience.
This framework of health includes six interdependent dimensions that influence and interact with each other.
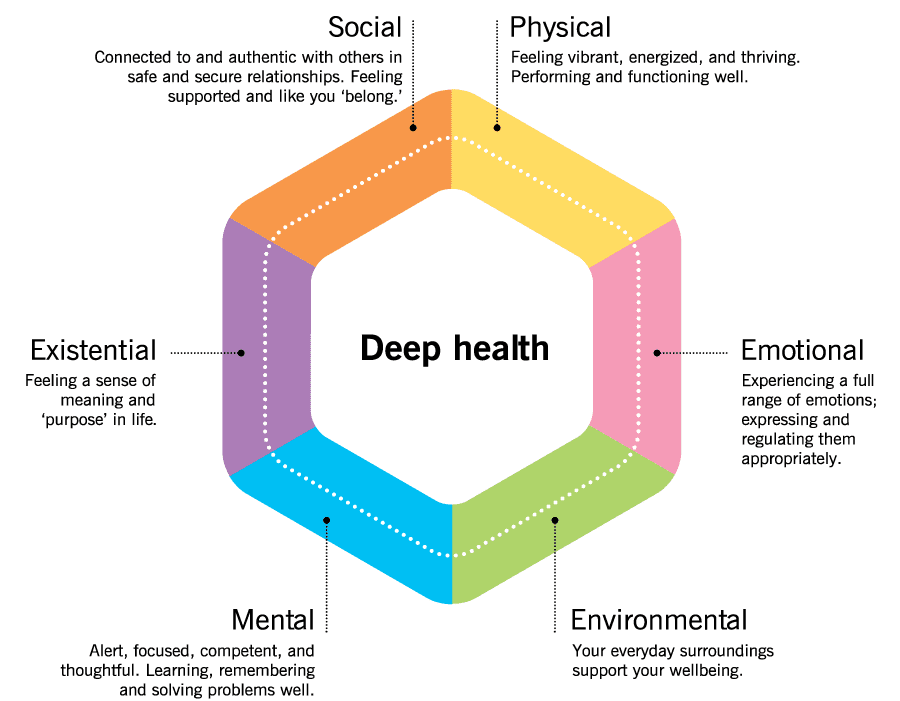
These six dimensions are:
 Physical health
Physical health
The one we all know best, and what people have historically thought of when thinking about health.
This is how your body feels, functions, and performs.
We measure physical health with blood work—such as your cholesterol and hormone levels and your blood pressure—as well as performance metrics like V02 max and demonstrations of strength, and subjective measures like energy and pain levels.
 Emotional health
Emotional health
This is about feeling a full range of emotions, but having more positive than negative feelings.
You can recognize, regulate, and appropriately express your emotions directly, maturely, and honestly. You have the resilience to recover from strong emotions, and calm yourself when you become stressed, anxious, or upset.
 Environmental health
Environmental health
This is about being and feeling safe and secure, as well as being and feeling supported by your everyday surroundings.
You have access to resources (health care, healthy food, clean air and water, nature) that support your goals and wellbeing.
 Mental or cognitive health
Mental or cognitive health
This is related to how well you think, learn, remember, and creatively problem-solve.
Your mind is sharp, and you’re able to be your most productive and do your best thinking.
This dimension also includes your mindset, capacity for insight, and your perspective and outlook on the world.
 Existential or purposeful health
Existential or purposeful health
Some might think of this as spiritual or soul health.
You have a deeper “why” or purpose for your life; you feel part of a “bigger picture.”
You have a strong sense of yourself and your intrinsic self-worth. You work to fulfill your purpose by choosing behaviors that align with your identity and values.
 Social or relational health
Social or relational health
This is about connecting and interacting well with others.
You develop and maintain authentic, fulfilling relationships. You have a sense of belonging, and you feel respected, “seen,” valued, and supported by others.
If you have Deep Health, it’s almost a guarantee…
You’re experiencing a life well-lived. A vibrant, thriving life that’s healthy in every sense of the word.
Not surprisingly, such a life is also statistically more likely to last longer, with more of those years being enjoyable.
(For more on Deep Health, plus how you can use the concept to transform your own—or your clients’—health, read: The “Deep Health” coaching secret)
High-impact habits to boost Deep Health (and by extension healthspan, longevity, and biological age)
While there are many things that can impact healthspan, longevity, and biological age, the following will give you the best return on investment.
These aren’t always the “sexiest” actions, nor are they likely to sound “cutting edge” (partly because they’ve been tested by time and robustly proven by decades of research).
But—if you’re looking to maximize Deep Health for as long as possible—they’re the things worth spending your time on.
The most important thing is being active.
If there’s a “magical panacea” out there, it’s exercise.
Before you start beating yourself up for not being “a gym person”…
…Any activity helps…
…At any dose.
Whether you clean your yard, vacuum, play games with your pets or kids, or just do a little walking, tell yourself, “I’m doing great!”
Because you are. These activities make a positive, measurable difference.
If you want to level up, get in a mix of aerobic or cardiovascular exercise, strength training, and stability work (like yoga, tai chi, or balance-challenging exercises).
Again, these can be in whatever amounts you can, in ways you enjoy.
For quintuple stars, aim for at least 150 minutes per week of moderate aerobic exercise (or 75 minutes of intense aerobic exercise), plus two or more strength and stability training sessions per week. (If you do these activities with friends—bonus!—now you’re boosting social health too.)
In general, the more activity the better. (So long as you enjoy it—and your body is recovering adequately.)
A thoughtful diet—and a mindful approach to other substances—is big, too.
Rather than focus on food you “shouldn’t be eating,” center your attention on the abundance of foods that serve your health and wellbeing.
We’re talking:
- Lean proteins (which can come from animals and/or plants, like fish, chicken, tofu, eggs, tempeh, Greek yogurt)
- A rainbow of fruits and vegetables (fact: different colors provide different nutrients and benefits, so aim to eat all of the colors regularly)
- Minimally-processed carbohydrates (whole grains, beans and lentils, starchy tubers like potatoes and sweet potatoes, and winter squash)
- Healthy fats (from nuts, seeds, avocados, extra virgin olive oil, nut butters, and a little dark chocolate)
For help choosing higher-quality versions and a wide variety of the above categories, check out one of our most popular infographics: ‘What should I eat?!’ Our 3-step guide for choosing the best foods for your body
To stay hydrated, drink plenty of water. For variety, emphasize mostly zero-calorie drinks like unsweetened tea and coffee. (If you’re confused about how much fluid to drink every day, you’ll love the “pee chart” in this article: ‘How much water should I drink?’)
Avoid smoking or chewing tobacco, and if you drink alcohol, do so lightly to moderately.
And of course, getting quality sleep and regulating stress makes everything better.
Get enough quality sleep by prioritizing and protecting the time you rest.
Make your sleeping area as comfortable, quiet, and dark as possible. Figure out when you need to get to bed to get seven to eight hours of sleep, and ideally, start winding down with a relaxing bedtime ritual about half an hour to an hour before that time.
(Want to learn more about why sleep is so important—and how to get more of it? Check out our infographic: The power of sleep)
To build your emotional resilience and stress tolerance, incorporate soothing, self-regulating activities daily.
These activities are somewhat subjective (some people find it relaxing to sit and meditate, while others find it to be an opportunity for restless anxiety to boil over). However, “crowd favorites” include: breathing exercises, time in nature, various forms of self-expression (journaling, art, movement), or just a good soak in the tub.
One of the most important mindsets to adopt to help your mental and emotional health—although it can benefit all areas of life—is a growth mindset.
People with a growth mindset tend to view challenges and adversity as opportunities to grow, evolve, and learn. And turns out, this kind of perspective isn’t just good for your mental and emotional health, it boosts longevity, too.
Research shows that, compared to less optimistic individuals, those with a more positive attitude and a growth mindset about aging had a 43 percent lower risk of dying from any cause, and lived about 7.5 years longer.1 2
Lastly, don’t underestimate the power of finding your people—and a purpose.
Seeking and nurturing positive, supportive relationships is one of the best things you can do for your health.
And not just for your social health. Research shows that people who are satisfied with their relationships have better emotional health,3 cognitive health,4 and even physical health.5
In fact, one of the longest studies on human health—the Harvard Study of Adult Development, which tracked participants for nearly 80 years—showed that feeling happy and satisfied in one’s relationships was one of the best predictors of overall health, happiness, and longevity.6
(Feel like your social health could use a boost? We’ve got three strategies to improve connection in your life, right here: Is social health the secret to total-body health?)
Having a strong sense of purpose bolsters our health and longevity too.7 8
Interestingly, a sense of purpose seems to help people live longer, even when controlling for other markers of psychological well-being. So there’s something uniquely beneficial about having a strong purpose that’s different from, say, being happy.
A purpose can take time to uncover, but you can facilitate that discovery by devoting regular time to the “big questions” in life:
- Who are you, really?
- What do you want your life to be about?
- How do you want to live?
- More practically: What gets you out of bed in the morning? (Is it your family, or showing up for your clients? Or something else?)
But Deep Health isn’t just something you want to achieve—it also serves as a framework to help you make choices.
When you understand how Deep Health works, it can also help you answer the often vague and perplexing question, “How can I feel better?”
Knowing about your own Deep Health can tell you which area of your life to prioritize right now that will make the biggest impact on your overall health.
How to use Deep Health to help you prioritize next actions.
Start by assessing your current Deep Health to get a baseline status. Click on the image below to access your own free assessment.

© Precision Nutrition
Depending on what’s going on in your life right now, you might get a Deep Health score that looks like this:
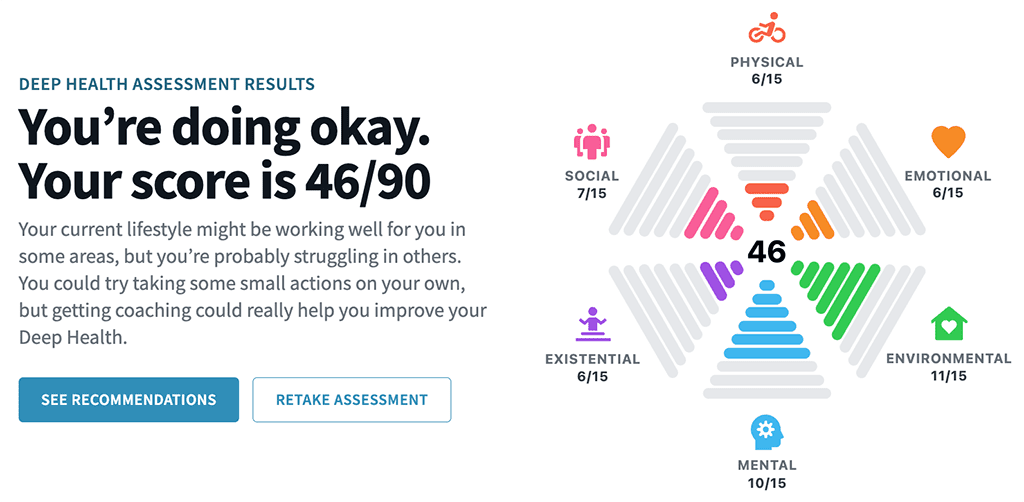
Or like this:
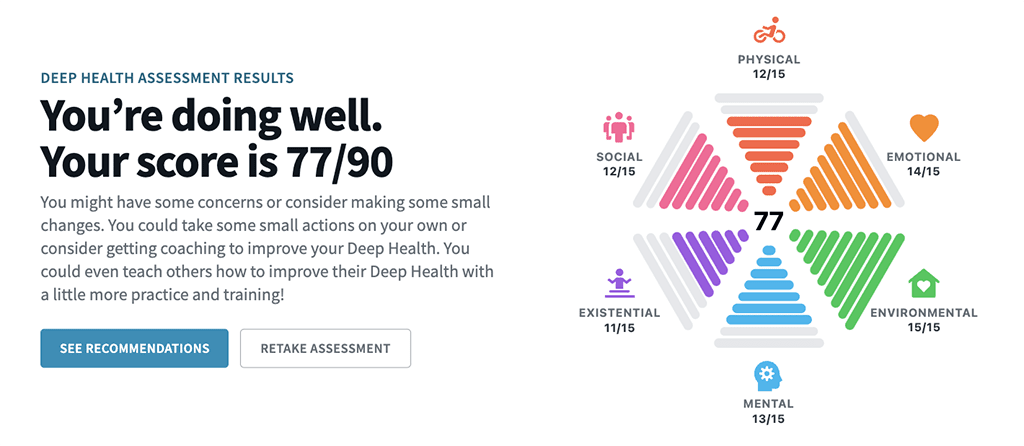
Or this:
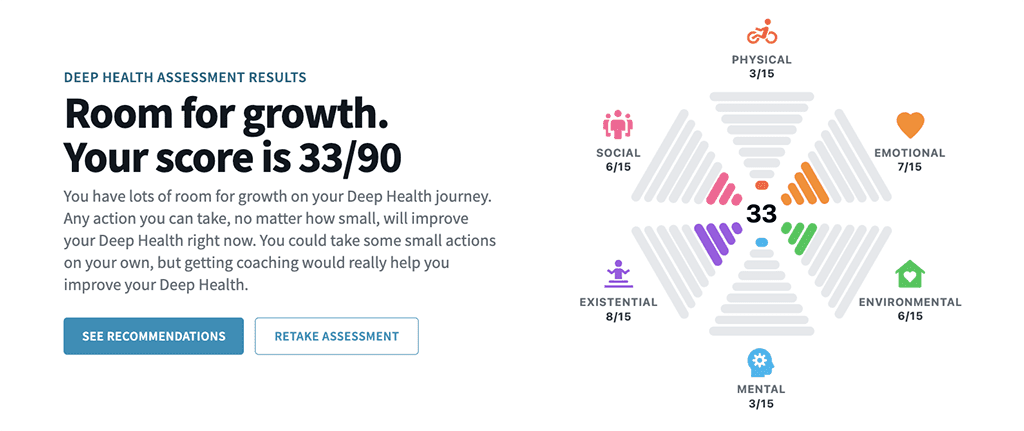
Whatever your results (and no judgment on the numbers), the distribution of your score can tell you:
- Where you’re currently thriving
- Where you have the largest opportunities for growth and improvement
- Where you might be able to make some easy improvements
- Which dimensions, if you improve them, might best help you reach (and sustain) your goals
Your personalized assessment will make some suggestions. (The below is a sample screenshot.)
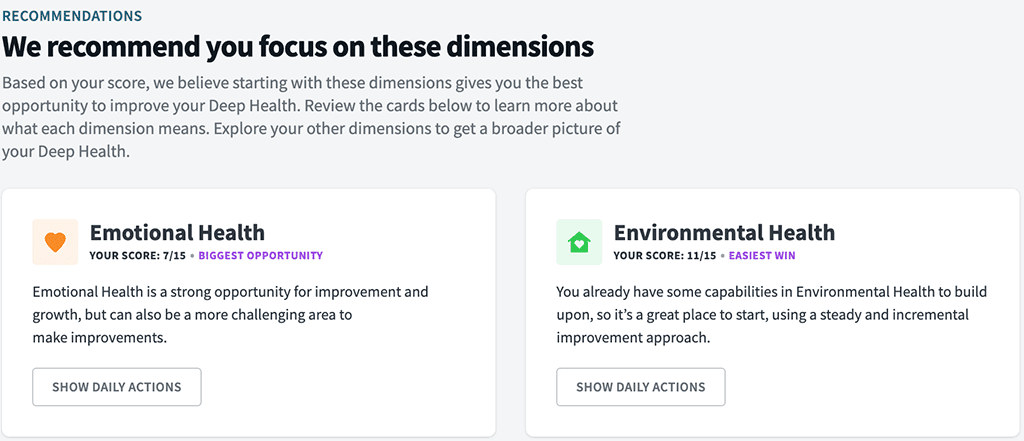
But of course, it’s entirely up to you where you decide to focus, and what actions you choose to take next—if any.
Let’s walk through an example
Let’s say you’ve recently become interested in optimizing health and longevity.
You’ve been listening to podcasts, you’ve read the articles about people “reversing” their biological age, and you feel fired up about it.
You haven’t felt so passionate or inspired about your health in a long time, and you’re excited to try some of the strategies recommended in those podcasts and articles. (You want to be 27 again! At least, your cells do.)
At the beginning of this journey, let’s imagine your Deep Health looks like this:
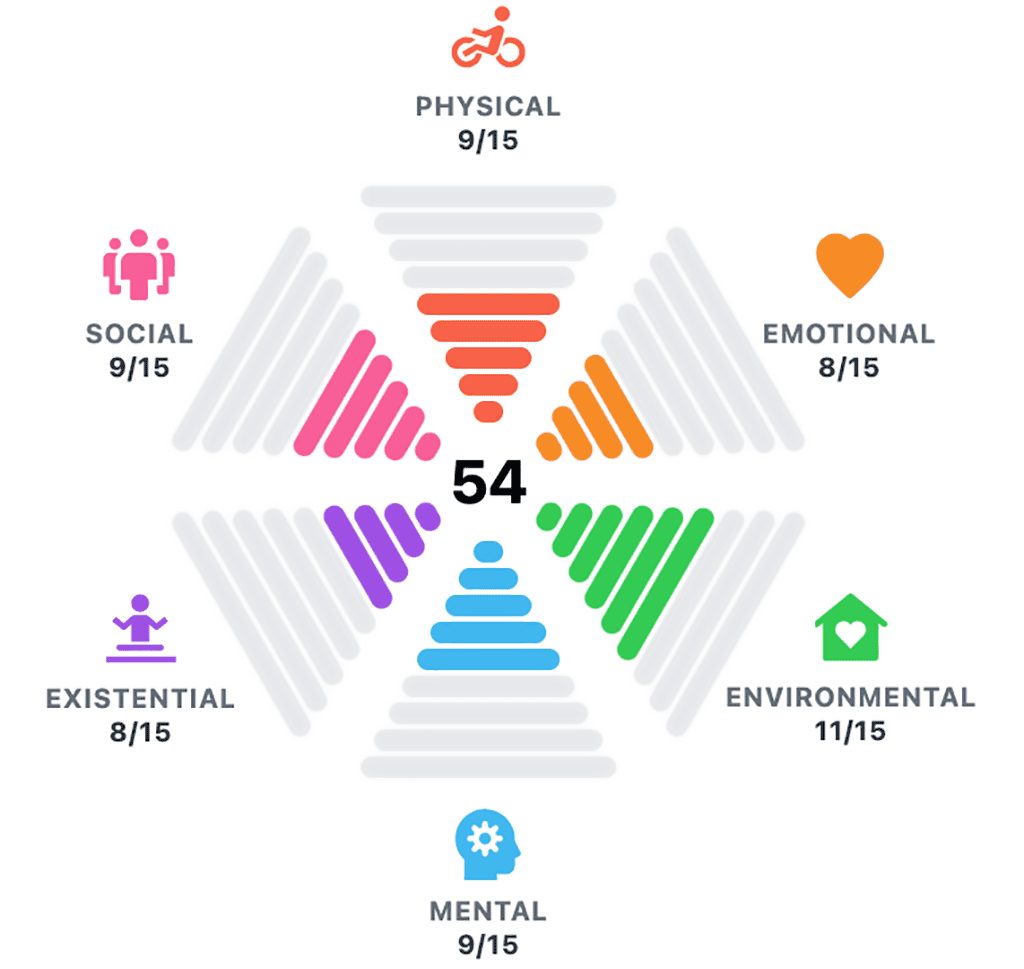
Kind of “so-so” all around. Definitely, there’s room for improvement.
Of course, in reality, there’s infinite pathways you could take. But let’s imagine two scenarios…
Scenario A: Biohack like a beast
After seeing your Deep Health score, you decide to simply tackle everything at once:
- You subscribe to a longevity-boosting supplement program, that has you taking about 20 different tablets and powdered elixirs per day.
- You start practicing 16:8 fasting (in each 24-hour cycle, you fast for 16 hours, and eat within an 8 hour window), eating only two meals per day.
- You start eating fully plant-based, getting in tons of veggies, fruits, and legumes, and start tracking your macros meticulously.
- You incorporate four 45-minute zone 2 cardio workouts a week (you heard that’s the amount needed to see significant benefit to your mitochondria).
- You also add two 60-minute resistance training sessions a week.
- You start taking cold plunges at the gym multiple times per week, and are even considering buying a cold plunge tank for your home.
For two weeks, you feel on top of the world.
Then, not so much. (You’ve actually grown to hate that green sludgy stuff you drink every morning.)
You continue to show up anyway with a gritty determination, and for months, follow your protocol as best as you can.
You forego social events, finding yourself grouchy and irritable. (When everyone else is munching on buttery canapés, you’re counting down the hours until your next feeding window.)
Every day feels like a Sisyphean effort, and you begin to wonder what the point of all of it is. You can’t imagine doing this for the rest of your life, which you’re (now ironically) trying to extend.
Eventually, all this white-knuckling in pursuit of optimal health starts to take a toll. On you, your marriage, your social life, and your mental and emotional wellbeing. And you want to know if all of this effort and suffering are worth it.
After several grueling months, you gather some data.
Your blood work looks awesome. You’re definitely leaner. And your biological age test tells you your rate of aging has slowed and your cells have gotten younger.
You’re… winning?
You decide to reassess your Deep Health, and it looks like this:
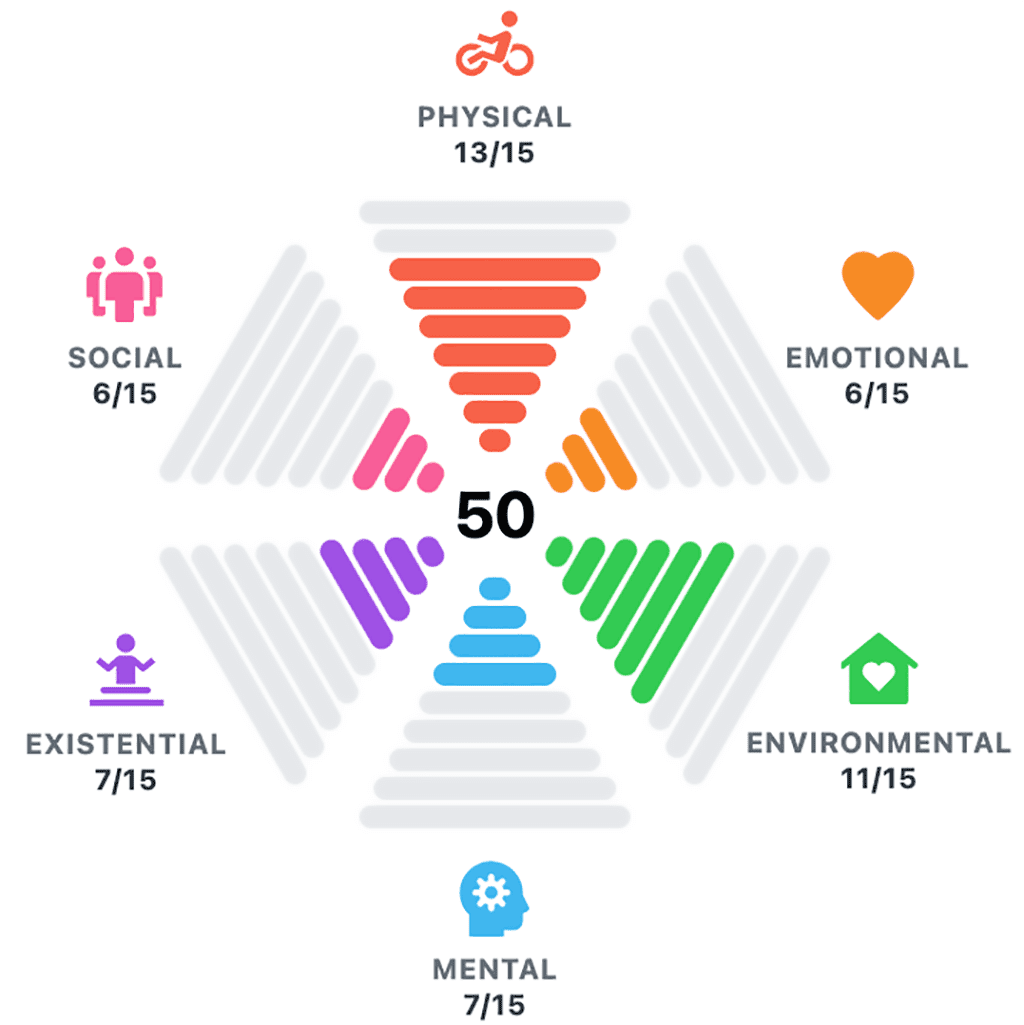
Your physical health has gone way up, but your emotional, social, mental, and existential health have all gone down. Overall, your Deep Health is somehow worse! (Argh!)
It becomes clear to you: While your “do all the things” protocol might help you live longer—it’s definitely not helping you live better.
Scenario B: Dig deep for Deep Health
In this scenario, you take a different approach.
Seeing your Deep Health starting point, you consider that list of “high impact habits” above.
You’re not sure which one to start with though, so you take some time to think about why you’re really interested in this whole longevity thing.
What’s your deeper purpose for wanting to live a longer, healthier life?
You think about your family, and tears come to your eyes when you conjure up the thought of your children having children, and imagining yourself tumbling around with a bunch of rambunctious grandkids. You want to be healthy, strong, and capable of playing with them.
This deep purpose aligns with your identity too. You’ve always been a “family guy,” and now you add a new layer on top of that: You decide to become the kind of person who makes their health and wellbeing a priority, so they can be there for their family for as long as possible.
With this new, revised identity and a clear purpose in mind, you begin to make some changes over time.
- You focus on eating protein at most every meal, and up your fruit and vegetable game too.
- You practice self-compassion when you can’t or just don’t get in as much protein or produce as you’d like. You also work on viewing your choices on a continuum—rather than simply “good” or “bad.” This flexibility helps you feel a sense of freedom in your diet, and feels a little more realistic, long-term.
- Instead of going for the “perfect” four cardio sessions, you aim for two a week, for as long as you can fit in (which sometimes is only 20 minutes, but you do your best). Any extra sessions are a bonus.
- You’re diligent with your resistance training, but you cap them at 30-45 minutes, twice per week (occasionally you only have 20 minutes for these sessions too, but you focus on consistency over perfection).
- You begin going for outdoor walks after dinner with your partner—sometimes inviting a few neighborhood friends, too—and enjoy the deep yet fun conversations you have about work, family, and life (and, let’s be honest, some good neighborhood gossip).
After several satisfying months, you gather some data.
Your blood work has improved. You’ve leaned out a touch too. Your rate of aging has also slowed and your biological age has decreased, seemingly just as much as Scenario A.
But the biggest difference: You enjoyed this process.
You found it not only physically beneficial, but also socially enriching, mentally and emotionally enlightening, and deeply meaningful.
You reassess your Deep Health, and it looks like this:
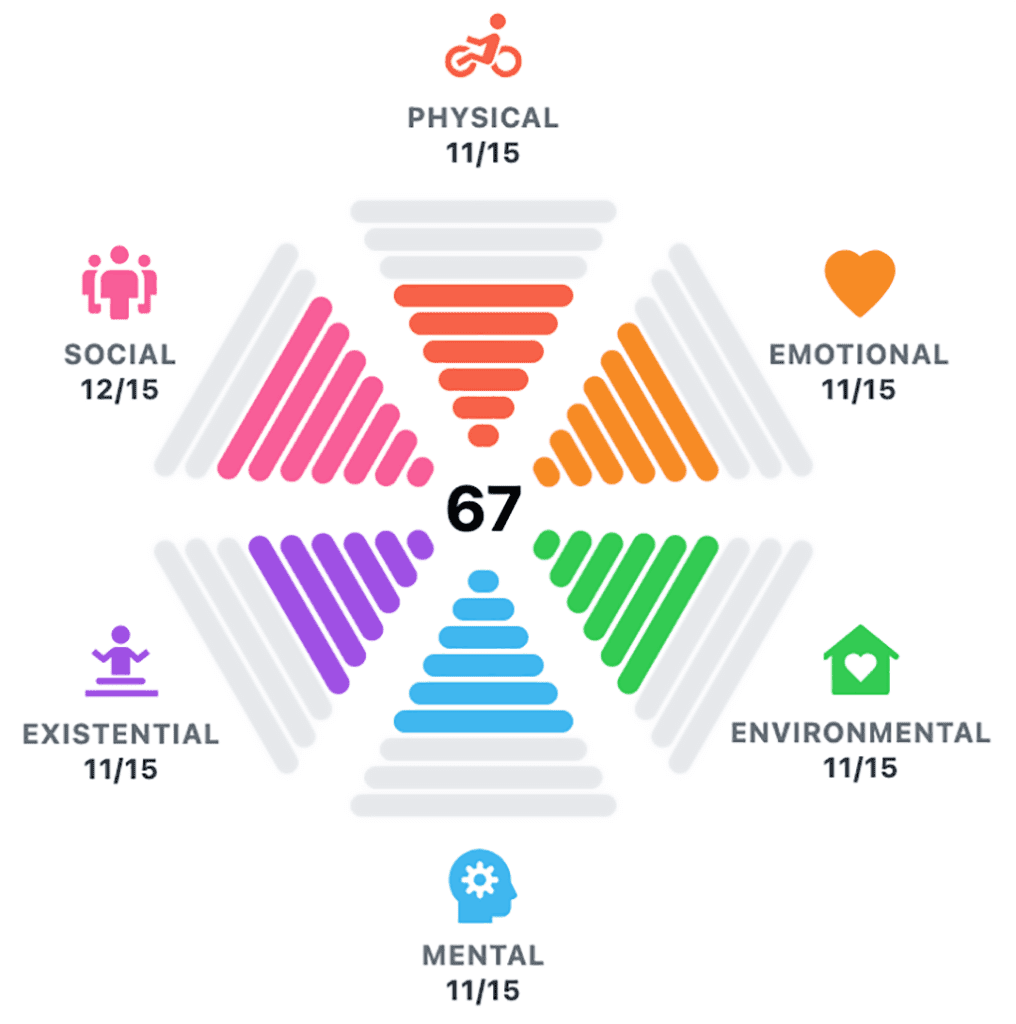
Your physical health has gone up (though not quite as high as Scenario A), and so has your emotional, social, mental, and existential health. Your overall Deep Health is now undeniably, significantly up.
The funny thing: It didn’t even seem that hard.
Moreover, you feel more inspired and energized than ever to take even more steps to further invest in your health and wellbeing.
This is the power of Deep Health.
It’s not just about improving your biological age or increasing your healthspan (which mostly center on physical health metrics).
Striving for Deep Health means working to thrive in ALL areas of your life—not just the physical. Because no single aspect of your health functions alone.
With the push towards longevity and healthspan, and the focus on things like biological age and “biohacking” for optimal aging, it can be easy to forget that we already know the fundamentals of what it means to experience a life well lived.
The truth is, scientists don’t know everything that improves our biological age. Or even the best ways to measure it.
However, if you’re thriving in all dimensions of your health and wellbeing—in other words, achieving Deep Health—you can bet you’re doing all of the things that matter most in living a long, healthy, rewarding life.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Nakamura, Julia S., Joanna H. Hong, Jacqui Smith, William J. Chopik, Ying Chen, Tyler J. VanderWeele, and Eric S. Kim. 2022. “Associations between Satisfaction with Aging and Health and Well-Being Outcomes among Older US Adults.” JAMA Network Open 5 (2): e2147797.
2. Levy, Becca R., Martin D. Slade, Suzanne R. Kunkel, and Stanislav V. Kasl. 2002. “Longevity Increased by Positive Self-Perceptions of Aging.” Journal of Personality and Social Psychology 83 (2): 261–70.
3. Block, Victoria J., Elisa Haller, Jeanette Villanueva, Andrea Meyer, Charles Benoy, Marc Walter, Undine E. Lang, and Andrew T. Gloster. 2022. “Meaningful Relationships in Community and Clinical Samples: Their Importance for Mental Health.” Frontiers in Psychology 13 (May): 832520.
4. Cook Maher, Amanda, Stephanie Kielb, Emmaleigh Loyer, Maureen Connelley, Alfred Rademaker, M-Marsel Mesulam, Sandra Weintraub, Dan McAdams, Regina Logan, and Emily Rogalski. 2017. “Psychological Well-Being in Elderly Adults with Extraordinary Episodic Memory.” PloS One 12 (10): e0186413.
5. Holt-Lunstad, Julianne, Timothy B. Smith, and J. Bradley Layton. 2010. “Social Relationships and Mortality Risk: A Meta-Analytic Review.” PLoS Medicine 7 (7): e1000316.
6. “Harvard Second Generation Study.” n.d. Harvardstudy. Accessed May 16, 2024. https://www.adultdevelopmentstudy.org/
7. Shiba, Koichiro, Laura D. Kubzansky, David R. Williams, Tyler J. VanderWeele, and Eric S. Kim. 2022. “Purpose in Life and 8-Year Mortality by Gender and Race/Ethnicity among Older Adults in the U.S.” Preventive Medicine 164 (107310): 107310.
8. Hill, Patrick L., and Nicholas A. Turiano. 2014. “Purpose in Life as a Predictor of Mortality across Adulthood.” Psychological Science 25 (7): 1482–86.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.
The post The PN framework that improves healthspan, longevity, and quality of life appeared first on Precision Nutrition.
Source: Health1
If you live in a larger body, sometimes it feels like you can’t win.
If you don’t lose weight, people will criticize you for being “lazy,” “unhealthy,” or “lacking willpower.”
But if you take medication to help you, you’ll be criticized for “cheating” or “taking the easy way out,” even if you’ve tried for decades to manage your weight through diet, exercise, and lifestyle changes (sometimes extreme ones).
In this article, we’ll be talking about a highly contentious group of medicines—GLP-1 receptor agonist drugs such as semaglutide (Ozempic, Wegovy, Rybelsus) or tirzepatide (Mounjaro, Zepbound).
And people have lots of opinions about them.
But the opinion that matters most? Yours.
At PN, we’re medication agnostic.
We’re not here to judge whether a person should or should not take medication for weight loss. Ultimately, that’s a choice left up to you, with the guidance of your primary care physician.
Either way, we’re here to support our clients and elevate their results.
Whether you take medication or not, a coach can help you optimize nutrition and satiety with the right foods, find exercises that work with your changing body, and help you navigate the emotional ups and downs that come when you attempt to tackle a big, meaningful, long-term goal.
However, we also understand that if you’re debating the pros and cons of beginning (or continuing) medication, you might have mixed feelings.
If you’re not sure if these new medicines are right for you, we have your back. In the following article, we’ll give you the honest, science-backed information you need to make a confident decision.
You’ll learn…
- Why it’s so hard to lose (and keep off) fat
- Why taking medication isn’t “cheating,” nor is it the “easy way out”
- How GLP-1 drugs work, and the health benefits they can have (aside from weight loss)
- How to determine if you’re at a “healthy weight” (it’s not just about BMI)
- What actions you can take to minimize side effects and maximize long-term health, if you do decide to take these medications
Let’s begin.
First, why is it so hard to lose fat?
Fat loss is hard. Period.
But for some people, it’s harder still—because of environmental, genetic, physiological, social, cultural, and/or behavioral factors that work against them.
Here are a few of the contributing factors that can make fat loss so challenging.
We live in an environment that encourages a caloric surplus.
Imagine life 150 years ago, before cars and public transit were invented. To get from point A to point B, you had to walk, pedal a bicycle, or ride a horse.
Food was often in short supply, too. You had to expend calories to get it, and meals would just satisfy you (but not leave you “full”).
Today, however…
“We live in an obesogenic environment that’s filled with cheap, highly-palatable, energy-dense foods [that make overeating calories easy, often unconsciously],” says Karl Nadolsky, MD, an endocrinologist and weight loss specialist at Holland Hospital and co-host of the Docs Who Lift podcast.
“We also have countless conveniences that reduce our physical activity.”
Of course, even in such an environment, we have people in lean bodies, just as we have people who struggle to stop the scale from continuously creeping up.
Why?
Genetically, some people are more predisposed to obesity.
Some genes can lead to severe obesity at a very early age. However, those are pretty rare.
Much more common is polygenic obesity—when two or more genes work together to predispose you to weight gain, especially when you’re exposed to the obesogenic environment mentioned earlier.
People who inherit one or more of these so-called obesity genes tend to have particularly persistent “I’m hungry” and “I’m not full yet” signals, says Dr. Nadolsky.
Obesity genes also seem to cause some people to experience what’s colloquially known as “food noise.”
They feel obsessed with food, continually thinking, “What am I going to eat next? When is my next meal? Can I eat now?”
Physiologically, bodies tend to resist fat loss.
If you gain a lot of fat, the hormones in your gut, fat cells, and brain can change how you experience hunger and fullness.
“It’s like a thermostat in a house, but now it’s broken,” says Dr. Nadolsky. “So when people cut calories and weight goes down, these physiologic factors work against them.”
After losing weight, your gut may continually send out the “I’m hungry” signal, even if you’ve recently eaten, and even if you have more than enough body fat to serve as a calorie reserve. It also might take more food for you to feel full than, say, someone else who’s never been at a higher weight.
Being in a larger body often means being the recipient of fat stigma and discriminatory treatment.
Until you’ve lived in a larger body, it’s hard to believe how different the world might treat you.
Our clients have told us stories about being bullied at the gym, openly judged or lectured at the grocery store, and otherwise being subjected to innumerable comments and assumptions about their body shape, health, and even worth.
Even in medical settings, people with obesity are more likely to receive poor treatment.1, 2 Healthcare providers may overlook or downplay symptoms, attributing health concerns solely to weight. This can lead to delayed- or missed diagnoses or just plain old inadequate care.
All of this combined can add up to an incredibly pervasive and ongoing source of stress.
This stress—in addition to being socially isolating and psychologically damaging—can further contribute to increased appetite and pleasure from high-calorie foods, decreased activity, and poorer sleep quality.3
Which is why…
Taking medication isn’t an “easy way out.”
In 2013, the American Medical Association categorized obesity as a disease.
And yet, many people still don’t treat it as such, and rather consider obesity as a willpower problem, and the consequence of simply eating too much and moving too little. (The remedy: “Just try harder.”)
In reality, people with obesity have as much willpower as anyone else.
However, for them, fat loss is harder—for all the reasons mentioned above, and more.
So, just like chemotherapy or insulin isn’t “the easy way out” of cancer or type 1 diabetes, medication isn’t “the easy way out” of obesity.
Rather, medication is a tool, ideally used alongside healthy lifestyle behaviors, that can help offset some of the genetic and physiological variances that people with obesity may have, and have little individual control over otherwise.
What you need to know about GLP-1 drugs
In 2017, semaglutide (a synthentic GLP-1 agonist) was approved in the US as an antidiabetic and anti-obesity medication.
With the emergence of this class of drugs, science offered people with obesity a relatively safe and accessible way to lose weight long-term, so long as they continued the medication.
How Ozempic and other obesity medicines work
Current weight loss medications work primarily by mimicking the function of glucagon-like peptide 1 (GLP-1), a hormone that performs several functions:
- In the pancreas, it triggers insulin secretion, which helps regulate blood sugar (and also helps you feel full).
- In the gut, it slows gastric emptying, affecting your sensation of fullness.
- In the brain, it reduces cravings (the desire for specific foods) and food noise (intrusive thoughts about food).
In people with obesity, the body quickly breaks down endogenous (natural) GLP-1, making it less effective. As a result, it takes longer to feel full, meals offer less staying power, and food noise becomes a near-constant companion, says Dr. Nadolsky.
Semaglutide and similar medicines flood the body with synthetically made GLP-1 that lasts much longer than the GLP-1 the body produces. This long-lasting effect helps increase feelings of fullness, reduce between-meal hunger, and muffle cravings and food noise.
Interestingly, by calming down the brain’s reward center (the part of the brain that drives cravings and even addictions), these medicines may also help people reduce addictive behaviors like compulsive drinking and gambling, says Dr. Nadolsky.
Note: Newer weight loss medicines, for example tirzepatide, mimic not only GLP-1, but also another hormone called gastric inhibitory polypeptide (GIP). Like GLP-1, GIP also stimulates post-meal insulin secretion and reduces appetite, partly by decreasing gastrointestinal activity. Other drugs soon to come on the market, like retatrutide, mimic a third hormone, glucagon.
How effective are GLP-1 drugs?
Researchers measure a weight loss medicine’s success based on the percentage of people who reach key weight loss milestones of 5, 10, 15, or 20 percent of their weight.
These medicines are still evolving, but so far, they have shown to be quite effective:
About 86 percent of people who take GLP-1 drugs like Ozempic, Rybelsus, and Wegovy lose at least five percent of their body weight, with about a third of them losing more than 20 percent of their body weight.4, 5
And newer generation versions of these medications—such as tirzepatide, and the not-yet-FDA-approved retatrutide—are only getting better, with up to 57 percent of people losing more than 20 percent of their body weight.6, 7
How do weight loss medications compare to lifestyle interventions?
In the past, weight loss interventions have focused on lifestyle modifications like calorie or macronutrient manipulation, exercise, and sometimes counseling.
Rather than pitting lifestyle changes against weight loss medicines or surgery, it’s more helpful to think of them all as compatible players.
With lifestyle modifications and coaching, the average person can expect to lose about five to 13 percent of their body weight.
When you add FDA-approved versions of GLP-1 and other weight-loss drugs to lifestyle and coaching, average weight loss jumps up another ten percent or more. 8, 9, 10, 11
Fat loss often comes with powerful health benefits
For years, the medical community has told folks that losing 5 to 10 percent of their body weight was good enough.
Partly, this message was designed to right-set people’s expectations, as few lose much more than that (and keep it off) with lifestyle changes alone.
In addition, this modest weight loss also leads to measurable health improvements. Lose 5 to 10 percent of your total weight, and you’ll start to see blood sugar, cholesterol, and pressure drop.12
However, losing 15 to 20 percent of your weight, as people tend to do when they combine lifestyle changes with second-generation GLP-1s, and you do much more than improve your health. You can go into remission for several health problems, including:
- High blood pressure
- Diabetes
- Fatty liver disease
- Sleep apnea
That means, by taking a GLP-1 medicine, you might be able eventually to stop taking several other drugs, says Dr. Nadolsky.
Experts suspect GLP-1s may improve health even when no weight loss occurs.
“The medicines seem to offer additive benefits beyond just weight reduction,” says Dr. Nadolsky.
Research indicates that GLP-1s may reduce the risk of major cardiovascular events (heart attacks and strokes) in people with diabetes or heart disease.13, 14, 15 In people with diabetes, they seem to improve kidney function, too.16
The theory is that organs throughout the body have GLP-1 receptors on their cells. When the GLP-1s attach to these receptors in the kidneys and heart, they seem to protect these organs from damage.
For this reason, in 2023, the American Heart Association listed GLP-1 receptor agonists as one of the year’s top advances in cardiovascular disease.
What even is a “healthy body weight”?
Many people say, “I just want to be at a healthy weight.”
But what does that even mean?
At PN, we believe your healthiest body composition / weight is one that:
- Has relatively more lean mass (from muscle and healthy, dense bones), and relatively less body fat
- Emerges from doing foundational, sustainable health-promoting behaviors (like being active and eating well), rather than “crash diets” or other extreme measures
- Is relatively easy to maintain with a handful of consistent lifestyle choices, without undue sacrifices to overall well-being (or what we call Deep Health)
- Allows you to do the activities you want and enjoy, with as few limitations as possible
- Keeps your health markers (like blood pressure, cholesterol, and blood sugar) in safe and healthy ranges as much as is reasonably possible
- Feels good to you
This is not a specific size, shape, look, body fat percentage, or category on a BMI chart; A “healthy” body composition and/or weight will vary from person to person.
… Which can be both freeing and frustrating to hear.
Without a specific number to aim for, it’s harder to know if you’ve “arrived” at your healthiest weight or body composition.
However, we like this way of qualifying what a healthy weight is because it takes the pressure off a number on the scale, and puts the focus on behaviors you have more control over, and more importantly, how your life feels.
7 strategies to make weight loss medicines more effective—and improve long-term health
Here’s what we believe:
Weight loss medicines don’t render lifestyle changes obsolete; they make them more critical.
When GLP-1 medicines muffle food noise and hunger, many find it easier to prioritize lean protein, fruits and veggies, whole grains, and other minimally processed foods. Similarly, as the scale goes down, people often feel better, so they’re more likely to embrace weight lifting and other forms of exercise.
Indeed, according to a 2024 consumer trends survey, 41 percent of GLP-1 medicine users reported that their exercise frequency increased since going on the medication. The majority of them also reported an improvement in diet quality, choosing to eat more protein, as well as fruits and vegetables.17
This is great news, because it further reinforces the idea that medication isn’t simply “the easy way out.”
(Of course, sometimes drugs are used as “the easy way out”; After going on medication, people can continue to eat poor quality food—just less of it. This increases the risk of losing critical muscle and bone, and losing less—or even no—body fat.)
When used correctly, weight loss medication is a tool that, as mentioned above, can make healthy lifestyle changes easier to accomplish, making both the drugs and the lifestyle changes more effective, and enhancing both short- and long-term success.
If you do decide to take weight loss drugs, use these strategies to get the most out of them—and preserve your long-term health.
Strategy #1: Find ways to eat nutritiously despite side effects.
The slowed stomach emptying caused by GLP-1 drugs can trigger nausea and constipation.
Fortunately, for most people, these GI woes tend to resolve within several weeks.
However, if you’re experiencing a lot of nausea, you’re not likely going to welcome salads into your life with open arms. (Think of how you feel when you have the stomach flu. A bowl of roughage doesn’t seem like it’ll “go down easy.”)
So, try to find more palatable ways to consume nutritious foods. (For example, fruits and vegetables in the form of a smoothie or pureed soup might be easier.)
Dr. Nadolsky also suggests people avoid the following common offenders:
- Big portions of any kind
- Greasy, fatty foods
- Highly processed foods
- Any strong food smells that trigger your gag reflex
- Sugar alcohols (like xylitol, erythritol, maltitol, and sorbitol, often found in diet sodas, chewing gum, and low-sugar protein bars), which can trigger diarrhea in some
Strategy #2: Prioritize strength training.
When people take GLP-1 weight loss medicines, about 30 to 40 percent of the weight they lose can come from lean mass.18, 19, 20
Put another way: For every 10 pounds someone loses, about six to seven come from fat and three to four from muscle, bone, and other non-fat tissues.
However, there’s two important caveats to this statistic:
1. People with severe obesity generally have more muscle and bone mass than others. (Carrying around an extra 100+ pounds of body weight means muscles have to adapt by getting bigger and stronger.)
2. Muscle and bone loss aren’t inevitable. (As Dr. Nadolsky puts it, “Muscle loss isn’t a reason to avoid treating obesity [with medication]. It’s a reason to do more exercise.”)
To preserve muscle and bone mass, aim for at least two full-body resistance training sessions a week.
In addition, move around as much as you can. Walking and other forms of physical activity are vital for keeping metabolism healthy—and can help to move food through the gut to ease digestion.21, 22
(Need inspiration for strength training? Check out our free exercise video library.)
Strategy #3: Lean into lean protein.
In addition to strength training, adequate protein consumption is vital for helping to protect muscle mass.
You can use our free macros calculator to determine the right amount of protein for you. (Spoiler: Most people will need 1 to 2 palm-sized protein portions per meal, or about 0.5 to 1 gram of protein per pound of body weight per day.)
Strategy #4: Fill your plate with fruit and veggies.
Besides being good for your overall health, whole, fresh, and frozen produce fuels you with critical nutrients that can help drive down levels of inflammation.
In addition to raising your risk for disease, chronic inflammation can block protein synthesis, making it harder to maintain muscle mass.
(Didn’t know managing inflammation matters when it comes to preserving muscle? Find out more muscle-supporting strategies here: How to build muscle strength, size, and power)
Strategy #5: Choose high-fiber carbs over low-fiber carbs.
Beans, lentils, whole grains, and starchy tubers like potatoes and sweet potatoes do a better job of helping you feel full and managing blood sugar than lower-fiber, more highly processed options.
(Read more about the drawbacks—and occasional benefits—of processed foods here: Minimally processed vs. highly processed foods)
Strategy #6: Choose healthy fats.
Healthy fats can help you feel full between meals and protect your overall health.
Gravitate toward fats from whole foods like avocado, seeds, nuts, and olive oil, as well as fatty fish (which is a protein too!)—using them to replace less healthy fats from highly-processed foods (like chips or donuts).
(Not sure which fats are healthy? Use our 3-step guide for choosing the best foods for your body)
Strategy #7: Consider coaching.
It may go without saying, but the above suggestions are just the start.
(There’s also: quality sleep, social support, stress management, and more.)
While many people choose to tackle these strategies on their own, many others find that the support, guidance, and creative problem-solving that a good coach can provide makes the whole process a lot easier—not to mention more enjoyable and more likely to stick.
And that’s the real gift of coaching: A coach doesn’t just help you figure out what to eat and how to move; They help you remove barriers, build skills, and create systems and routines so that habits become so natural and automatic that it’s hard to imagine not doing them.
Then, if you do want to stop taking medication, your ingrained lifestyle habits (that coaching reinforced, and medication perhaps made easier to adopt) will make it more likely that you maintain your results.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Phelan, S. M., D. J. Burgess, M. W. Yeazel, W. L. Hellerstedt, J. M. Griffin, and M. van Ryn. 2015. “Impact of Weight Bias and Stigma on Quality of Care and Outcomes for Patients with Obesity.” Obesity Reviews: An Official Journal of the International Association for the Study of Obesity 16 (4): 319–26.
2. Tomiyama, A. Janet, Deborah Carr, Ellen M. Granberg, Brenda Major, Eric Robinson, Angelina R. Sutin, and Alexandra Brewis. 2018. “How and Why Weight Stigma Drives the Obesity ‘Epidemic’ and Harms Health.” BMC Medicine 16 (1).
3. Tomiyama, A. Janet. 2019. “Stress and Obesity.” Annual Review of Psychology 70 (1): 703–18.
4. Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021 Mar 18;384(11):989–1002
5. Garvey WT, Batterham RL, Bhatta M, Buscemi S, Christensen LN, Frias JP, et al. Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial. Nat Med. 2022 Oct;28(10):2083–91.
6. le Roux CW, Zhang S, Aronne LJ, Kushner RF, Chao AM, Machineni S, et al. Tirzepatide for the treatment of obesity: Rationale and design of the SURMOUNT clinical development program. Obesity. 2023 Jan;31(1):96–110.
7. Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022 Jul 21;387(3):205–16..
8. Leung, Alice W. Y., Ruth S. M. Chan, Mandy M. M. Sea, and Jean Woo. 2017. “An Overview of Factors Associated with Adherence to Lifestyle Modification Programs for Weight Management in Adults.” International Journal of Environmental Research and Public Health 14 (8).
9. Jastreboff, Ania M., Louis J. Aronne, Nadia N. Ahmad, Sean Wharton, Lisa Connery, Breno Alves, Arihiro Kiyosue, et al. 2022. “Tirzepatide Once Weekly for the Treatment of Obesity.” The New England Journal of Medicine 387 (3): 205–16.
10. Jastreboff, Ania M., Lee M. Kaplan, Juan P. Frías, Qiwei Wu, Yu Du, Sirel Gurbuz, Tamer Coskun, Axel Haupt, Zvonko Milicevic, and Mark L. Hartman. 2023. “Triple–Hormone-Receptor Agonist Retatrutide for Obesity — A Phase 2 Trial.” The New England Journal of Medicine 389 (6): 514–26.
11. Maciejewski, Matthew L., David E. Arterburn, Lynn Van Scoyoc, Valerie A. Smith, William S. Yancy Jr, Hollis J. Weidenbacher, Edward H. Livingston, and Maren K. Olsen. 2016. “Bariatric Surgery and Long-Term Durability of Weight Loss.” JAMA Surgery 151 (11): 1046–55.
12. Ryan DH, Yockey SR. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr Obes Rep. 2017 Jun;6(2):187–94.
13. Marx N, Husain M, Lehrke M, Verma S, Sattar N. GLP-1 Receptor Agonists for the Reduction of Atherosclerotic Cardiovascular Risk in Patients With Type 2 Diabetes. Circulation. 2022 Dec 13;146(24):1882–94.
14. Lincoff AM, Brown-Frandsen K, Colhoun HM, Deanfield J, Emerson SS, Esbjerg S, et al. Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes. N Engl J Med. 2023 Dec 14;389(24):2221–32.
15. Kosiborod MN, Abildstrøm SZ, Borlaug BA, Butler J, Rasmussen S, Davies M, et al. Semaglutide in Patients with Heart Failure with Preserved Ejection Fraction and Obesity. N Engl J Med. 2023 Sep 21;389(12):1069–84.
16. Karakasis P, Patoulias D, Fragakis N, Klisic A, Rizzo M. Effect of tirzepatide on albuminuria levels and renal function in patients with type 2 diabetes mellitus: A systematic review and multilevel meta-analysis. Diabetes Obes Metab [Internet]. 2023 Dec 20
17. N.d. Accessed May 21, 2024. https://newconsumer.com/wp-content/uploads/2024/03/Consumer-Trends-2024-Food-Wellness-Special.pdf
18. Ida S, Kaneko R, Imataka K, Okubo K, Shirakura Y, Azuma K, et al. Effects of Antidiabetic Drugs on Muscle Mass in Type 2 Diabetes Mellitus. Curr Diabetes Rev. 2021;17(3):293–303.
19. Wilding JPH, Batterham RL, Calanna S, Van Gaal LF, McGowan BM, Rosenstock J, et al. Impact of Semaglutide on Body Composition in Adults With Overweight or Obesity: Exploratory Analysis of the STEP 1 Study. J Endocr Soc. 2021 May 3;5(Supplement_1):A16–7.
20. Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021 Mar 18;384(11):989–1002.
21. Gorgojo-Martínez JJ, Mezquita-Raya P, Carretero-Gómez J, Castro A, Cebrián-Cuenca A, de Torres-Sánchez A, et al. Clinical Recommendations to Manage Gastrointestinal Adverse Events in Patients Treated with Glp-1 Receptor Agonists: A Multidisciplinary Expert Consensus. J Clin Med Res [Internet]. 2022 Dec 24;12(1).
22. Tantawy SA, Kamel DM, Abdelbasset WK, Elgohary HM. Effects of a proposed physical activity and diet control to manage constipation in middle-aged obese women. Diabetes Metab Syndr Obes. 2017 Dec 14;10:513–9.
The post Considering (or currently taking) weight loss drugs? Here’s what you need to know appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
We all make thousands of decisions every day, large and small.
What to have for breakfast. Whether or not to exercise—or when. Which project to tackle first at work. More coffee or not.
After a while, it’s only natural that decision fatigue sets in.
Decision fatigue can happen to anyone—but it’s especially disruptive when you’re trying to change old habits and make new (healthier) choices, but you lose steam by 10 AM.
Let’s take a closer look at what decision fatigue is, what causes it, and how to shake it off so you can continue to make good, intentional choices ongoing.
What is decision fatigue, anyway?
Decision fatigue refers to the deteriorating quality of decisions made after a prolonged period of decision-making. Decision fatigue can also happen when faced with an overwhelming number of choices.
When working toward wellness goals, the mental exhaustion from constant decision-making can hinder your ability to make positive choices, especially in areas like exercise and nutrition. The constant evaluation of your workout schedules, meal choices, and other aspects of your lifestyle and routine can lead to decision fatigue.
Signs of decision fatigue
Decision fatigue can manifest in several ways. It might last days, weeks, or longer.
Here are six common signs that you might be experiencing it.
Sign #1: Procrastination and avoiding decisions
One of the primary signs of decision fatigue is procrastination and the tendency to avoid making choices. As decision fatigue sets in, you may find it increasingly challenging to initiate or conclude decision-making processes, leading to delays and lack of action.
Sign #2: Impulsivity
On the other hand, decision fatigue can also manifest as impulsivity. In an effort to expedite decision-making and alleviate mental strain, you may resort to impulsive choices, increasing the likelihood of taking less thoughtful actions.
Sign #3: Exhaustion
Decision fatigue often leads to mental exhaustion. You may feel tired and mentally drained, which may affect your overall cognitive functioning and energy levels.
Sign #4: Brain fog
A common symptom of decision fatigue is the sensation of “brain fog.” This mental cloudiness can hinder clarity of thought, making it difficult for individuals to focus, process information, and make wise choices.
Sign #5: Overwhelm
As decision fatigue accumulates, individuals may become easily overwhelmed by even minor choices. Tasks that would typically be manageable may seem daunting, contributing to heightened stress levels.
Sign #6: Irritability
Decision fatigue can lead to increased irritability and emotional sensitivity. The mental strain from continuous decision-making may impact an individual’s patience and tolerance, resulting in reactive emotional responses.
What causes decision fatigue?
A combination of factors can contribute to decision fatigue.
Cause #1: You’re always making decisions.
When you find yourself constantly making numerous decisions throughout the day, from choosing what to wear to deciding on work-related tasks, you may be prone to decision fatigue.
The cumulative effect of these daily choices can overwhelm your cognitive resources, making subsequent decisions more challenging.
Cause #2: You make a lot of decisions that impact other people.
Decisions that have a significant impact on others can contribute to decision fatigue.
When your choices carry weight and affect those around you, the mental burden intensifies. Balancing personal and professional responsibilities that influence others can lead to a heightened sense of responsibility and decision-related stress.
Cause #3: You make stressful or complex decisions.
Engaging in decision-making that is particularly stressful or complex can accelerate the onset of decision fatigue.
Evaluating intricate scenarios, especially under pressure, demands more cognitive resources, expediting mental exhaustion. High-stake decisions amplify the toll on your mental energy, making subsequent choices more taxing.
Cause #4: You’re experiencing a difficult or uncertain life situation.
Life situations characterized by difficulty or uncertainty can exacerbate decision fatigue.
Coping with unusually stressful challenges, whether personal or professional, consumes mental bandwidth. Navigating through uncertainty heightens decision-related stress, intensifying the impact of decision fatigue.
How does decision fatigue relate to your health and wellness?
Decisions related to diet, exercise, and overall health management can be overwhelming.
Constantly evaluating food choices, workout routines, and health-related decisions can challenge cognitive resources, exacerbating decision fatigue.
Further, when experiencing decision fatigue, your ability to make thoughtful, proactive health decisions diminishes. Fatigue may lead to impulsive choices, such as impulsive eating or skipping workouts, impacting your progress toward your goals.
How to overcome decision fatigue
Overcoming decision fatigue may not happen instantly, but by following these tips, you can significantly reduce its effect on your health and well-being.
All it takes is some careful planning and learning to let go.
Strategy #1: Remove choice from areas of your life where you can.
The intentional simplification of daily decisions not only streamlines your life but also enhances your cognitive capacity for more meaningful and impactful choices.
One approach is to establish routines to set some aspects of your daily life in stone—no decisions necessary. This deliberate structuring (such as predetermining what days/times you do your workouts) serves to reduce the ongoing need for decision-making in these areas.
Implementing routines also provides a psychological framework that turns repetitive decisions into automatic actions. For instance, adopting a regular weekly meal prep ritual.
Of course, this strategy is particularly beneficial for recurring activities, where predetermined choices can be consistently applied. This act of intentionally removing choices can give you back a sense of control and predictability in your daily life.
Strategy #2: Delegate where you can.
Whether in the workplace or at home, delegating decisions to others not only lightens your cognitive (and practical) burden but also promotes collaboration.
Distributing tasks at work fosters a sense of shared responsibility—and of course lightens your workload. By involving team members in decision-making processes, you not only benefit from diverse perspectives but also empower others to contribute their expertise.
Similarly, within the family or household, delegating responsibilities not only shares the cognitive load but also promotes a more supportive environment. This practice allows each family member to contribute their unique strengths, creating a more balanced distribution of decision-making responsibilities.
Strategy #4: Prioritize relaxation activities.
Relaxation activities are particularly effective in combating the effects of decision fatigue.
Quality sleep rejuvenates cognitive functions and replenishes mental energy. When you’re well-rested, you’re better equipped to face the challenges of decision-making.
In addition to sleep, try engaging in mindfulness practices, such as meditation or deep breathing exercises.
Exercise, too, not only promotes better sleep but also releases endorphins, which elevate mood and improve cognitive function.
Strategy #5: Manage stress and practice self-care.
Stress and decision fatigue are connected, so learning to manage the former will help alleviate symptoms of the latter.
Many of the relaxation techniques we previously mentioned are also great stress management tactics.
Try establishing a consistent self-care routine, like reading, taking a warm bath, or spending quality time with loved ones. These activities can provide a mental break and contribute to a positive mindset, which, in turn, helps prevent and reduce decision fatigue.
Strategy #6: Work with a coach.
By hiring a coach, you effectively delegate certain decisions to an expert.
By leveraging their knowledge, you not only streamline decision-making but also gain valuable insights and support on your journey to optimal health.
A health coach provides guidance on fitness, nutrition, sleep, stress, and recovery, and can design tailored plans to help you improve each of these areas.
Moreover, a health coach assists in establishing routines, contributing to the removal of unnecessary decisions from your daily life.
Working with a coach offers personalized support, helping you navigate health-related decisions while also enhancing accountability and motivation.
We’re here to help you reach your goals
At Precision Nutrition, our coaches are certified experts who can help you make positive decisions to improve your life. Decision fatigue ends with us, as every client receives a personalized, tailored plan designed to work with their personal preferences, lifestyle, and goals.
Learn more about how the coaches at Precision Nutrition can help you learn to live the healthier, more well-balanced life you deserve.
The post How to navigate decision fatigue when working toward your fitness goals appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
Once you decide you want to work with a health coach, finding the right one goes beyond checking off a list of qualifications.
How do you know if you’ve found the best health coach for you? What are the qualities of a good coach besides the obvious credentials?
We’ve listed some traits to look out for when choosing a health coach.
Essentially, it all boils down to how the two of you “vibe.” You should find someone you get along with and trust, someone who seems to truly “get” you and is as invested in your success as you are.
Let’s dive deeper into what all that means.
Why is it important to find a good health coach?
A skilled health coach serves as a personalized guide.
They’ll help you achieve your goals with tailored advice, motivation, custom nutrition plans, and exercise routines designed specifically for you.
They won’t just give you generalized or generic advice about diet and exercise. This individualized approach ensures that you maximize your full potential and make the most of your fitness journey.
7 signs you’ve found a good coach
What are the qualities of a good coach?
How do you know when you’ve found one?
These seven qualities are by no means an exhaustive list, but they can help you narrow down your options.
1. They can walk you through their process.
A good health coach should possess the skill to clearly explain the steps, strategies, and milestones integral to their approach.
This not only demonstrates their expertise but also shows that they have a structured process to help you succeed.
Even more than that, they should also be able to draw on insights gained from practical experience. Articulating lessons learned from working with other clients like you shows understanding for the issues or preferences you might have. They’ve proven that they know how to address challenges similar to yours.
2. They can provide references and testimonials.
A hallmark of a good coach is their openness to share references and testimonials without hesitation. Transparency not only reflects confidence in their ability but also underscores their commitment to client satisfaction.
Ideally, these references should be from clients in your demographic with similar goals. If you have a particular injury, for example, a good coach will have testimonials from clients they’ve worked with in the past who experienced a similar injury or physical limitation. A good coach understands the value of real-world feedback and recognizes that the experiences of past clients can speak volumes.
Moreover, the ability to connect with past clients demonstrates a coach’s confidence in the relationships they’ve built. If a coach avoids providing references, that should raise concerns about their client interactions and the impact of their coaching.
Testimonials, in particular, offer insights into the tangible benefits clients have experienced under a coach’s guidance. Positive testimonials not only validate the coach’s skills but also provide you with a glimpse of the potential results you can expect.
3. They ask you questions.
A coach’s interest in your story is a reflection of their commitment to your success. They should ask you questions—lots of them. A quality coaching relationship is built on a foundation of understanding, and effective coaches recognize the importance of delving into your unique circumstances.
Rather than simply presenting a pre-packaged solution, a good coach should be genuinely interested in your “why.” They should want to understand your motivations, challenges, and specific goals. The questions they ask should help them tailor their coaching plan to your particular preferences and lifestyle.
4. They listen to you.
Another quality of a good coach is the ability to integrate your thoughts and feedback into the coaching process. Remember, this is a two-way, collaborative relationship.
Listening extends beyond the spoken word; it involves deciphering the nuances and subtleties of your communication. A good coach is attuned to not only what you say but how you say it.
A coach’s responsiveness to your feedback should foster an environment of trust. If you express concerns or suggest modifications to the plan, a good coach listens, understands, and adapts the program. This flexibility ensures that the coaching process remains dynamic, adjusting to your evolving needs and circumstances.
5. They communicate openly and often.
As we said, transparent and open communication is a two-way street. This element is fundamental to your success and includes how and when you and your coach touch base.
Effective coaches establish clear expectations regarding communication from the outset. Whether it’s setting regular check-ins, defining response times, or outlining preferred communication channels, a good coach is accessible to you and reliable in responding. You should feel comfortable reaching out, knowing that your coach is receptive to any questions or concerns you have.
6. They consider your health holistically.
Your well-being extends beyond isolated facets like exercise and nutrition. You’ll know you’ve found a good health coach when they also take into account your sleep quality, stress levels, past injuries, and exercise experience. They know how these factors work together and influence one another.
For instance, understanding your nutritional habits allows a coach to develop a diet plan that improves on your current eating habits, without being unrealistic. Acknowledging past injuries or exercise experiences informs workout routines that prioritize safety and effectiveness. The consideration of sleep patterns and stress levels further refines the approach, promoting overall well-being.
This holistic, multi-faceted view of well-being is called “Deep Health.” And when a Deep Health approach is applied, it means you’re more likely to create positive habits that affect every aspect of your life—for the long term.
7. They can adjust your program to fit your needs.
A good coach will adjust your program to fit your changing needs as you work to achieve your goals.
Whether you have specific dietary requirements, time constraints, or preferences in workout styles, a coach tailors the program to ensure it not only helps you make progress but also integrates seamlessly into your lifestyle—and can adapt as necessary.
Tips for finding a good health coach
Finding a good health coach goes beyond looking up online reviews or asking friends for recommendations (though those are good ways to get started).
Here are some more tips to keep in mind as you look for a health coach.
Identify your goals
Before seeking a coach, take a moment for introspection.
Ask yourself why you want to work with a health coach and what specific outcomes you aim to achieve.
Whether it’s weight loss, improved fitness, better sleep, or overall well-being, clarity on your objectives serves as a guiding compass in selecting the right coach.
However, it’s also okay not to have a specific goal, or if your goal is something general like, “I want to be healthier.” Helping you clarify and refine your goals is part of a health coach’s job. They can engage you in meaningful conversations to understand your aspirations, challenges, and motivations until the two of you shape a tailored plan together.
Talk to prospective health coaches
Once you’ve identified three to five potential health coaches, take time to meet with each one-on-one.
Prepare a list of questions and talking points to guide these discussions. Your questions should focus on things like their coaching philosophy, past experiences, and success stories. Understanding how their approach aligns with your goals is essential to making sure you truly “get” one another.
During these conversations, also pay attention to the coach’s communication style and demeanor. Consider whether you feel comfortable and genuinely heard during the conversation.
Day-to-day logistics are important as well. As you get to know each coach, ask them about their availability, preferred communication channels, and the structure of the coaching sessions. This will ensure a smooth and manageable collaboration.
Evaluate the “vibe”
Coaching is, at its core, a relationship-based service, and the personal connection you establish with your coach can profoundly impact your motivation and commitment to your health goals. A positive and supportive connection fosters a sense of trust, making the coaching relationship more enjoyable and effective.
However, recognize that there’s no “perfect” coach.
Instead, focus on finding a coach who’s “good enough” for you—someone whose approach aligns with your preferences and understands your unique circumstances. While there might be a coach who, on paper, seems to fit all your criteria, less tangible elements like a coach’s personality, communication style, and general energy are paramount. Trust your instincts and choose a coach with whom you genuinely connect.
We’re here to help you reach your goals
The health coaches at Precision Nutrition are experts in their fields. They take the time to understand your behavior and habits as they design a plan to fit your unique goals and lifestyle.
Our coaches don’t just give you advice about diet and exercise. They work closely with you so you can learn healthier, sustainable habits that will help you feel better long term.
Try our 1:1 coaching program now and achieve the results you deserve.
The post How to know you’ve found a good health coach appeared first on Precision Nutrition.
Source: Health1

