I was 13 when I went on my first diet.
I had been struggling with my weight for about six years, and my obsession with how I looked was starting to dominate my life.
I only had two to three shirts that I felt comfortable in. The only thing that mattered was that they didn’t make me “feel fat.” Even those chosen shirts were always under my West 49 sweater, for extra coverage.
The cherry on top of this presentation was my slouched shoulders—a defense mechanism to protect against exposing my “man boobs,” the body part that had dynastic reign for being my biggest insecurity.
The way I viewed my body governed my self-worth.
I felt that my body held me back from enjoying countless moments of my life, and by the ripe age of 13, I decided I was sick of it.
I figured the only way I could change this purgatory was by changing my body.
I started exercising three to four times a day. For my first two meals a day, I drank a sludge of water mixed with “weight loss smoothie powder” (really just a glorified protein shake). Whenever I “cheated,” I punished myself the next day by eating even less or exercising even more.
In about 5 months, I lost 60 lbs. One third of my body weight to be exact.
This was how I spent the summer transitioning from elementary school to high school. Counting calories over making memories.
To no surprise, this was met with endless praise. And it felt good. Scratch that, it felt incredible.
I had experienced both sides now: One where I felt valueless because I was in a fatter body, and one where I felt accepted and prized because I was in a thinner body.
In another version of this story, I might’ve learned something from my newly widened perspective: I might’ve gained empathy, seeing the unfair stigma projected at people in larger bodies. I might’ve gained bravery, advocating for more body acceptance, regardless of someone’s size.
But instead, I participated in the problem.
I built up the identity of being a “former fat person” who is proof that “anybody can lose weight.”
However, as this script typically goes, over the next few years, I gained a lot of the weight back.
This sent me into a depression. I felt like I had lost my value; like I had won the lottery and blew through my fortune.
That was the pattern I repeated for almost 15 years.
Until I stumbled on something called “body neutrality.”
For me, adopting a more body-neutral approach created a paradigm shift—it offered a way to uncouple my appearance with my happiness. It also caused me to ask some deep questions about my body, and the kind of life I wanted.
Questions like:
“Do I want my self worth to be defined by my external appearance?”
“Do I want to continue this cycle—and potentially pass it on to any future kids I might have?”
“What would my life look like if I fought to value myself for who I am as opposed to what I look like?”
My answers weren’t immediately clear. But body neutrality created an opportunity to step off the hamster wheel of chasing aesthetic goals—and finally, truly reflect.
In this article, I’ll walk you through the process of adopting a more body neutral approach to your own self image and self-care.
You’ll learn:
- What body neutrality is
- How to think about your body and your health—in a way that isn’t dependent on appearance
- Five actionable, body neutral strategies you can apply today—if you want to stop letting your weight, size, or shape dictate your happiness
Let’s begin.
What is body neutrality?
Body neutrality is a mindset that encourages you to value how your body functions and feels over how it looks. This perspective helps you develop self-acceptance, while still working to care for yourself in ways that promote overall health.
In practice, this looks like:
 You exercise and eat nutritiously—not because it makes you look a certain way—but because it makes you feel good.
You exercise and eat nutritiously—not because it makes you look a certain way—but because it makes you feel good.
 You still have treats (because life is too short to be deprived of pizza!) but you don’t eat them to excess because they don’t make you feel the best, physically.
You still have treats (because life is too short to be deprived of pizza!) but you don’t eat them to excess because they don’t make you feel the best, physically.
 You wear clothes and celebrate your appearance in ways that feel authentic, but how you “display” yourself isn’t the foundation of your self-worth.
You wear clothes and celebrate your appearance in ways that feel authentic, but how you “display” yourself isn’t the foundation of your self-worth.
 You don’t always love all aspects of your body, but you don’t let that stop you from enjoying your life; Improving your appearance doesn’t “earn” you the right to be happy.
You don’t always love all aspects of your body, but you don’t let that stop you from enjoying your life; Improving your appearance doesn’t “earn” you the right to be happy.
 You might still care about how you look, but you broaden your self-concept so it also includes your values and your inherent worthiness as a human.
You might still care about how you look, but you broaden your self-concept so it also includes your values and your inherent worthiness as a human.
I value seeing friends and family. I value playing rec sports. I value new experiences.
When I’ve been heavier, I’ve neglected these things in favor of isolating myself.
“I’ll do them again when I lose weight” is something I’ve uttered to myself more times than I can count.
Body neutrality helped me realize I still deserved these things—no matter how I looked.
Everyone can benefit from body neutrality.
Body neutrality isn’t just for people in larger, or otherwise marginalized bodies.
It’s also useful for people with “ideal bodies,” who’ve been the recipients of validation and privilege because of the way they look.
“I’ve worked with clients who are fairly satisfied with their appearance, but they still struggle with their body image because their self-worth relies on it,” says Shannon Beer, registered nutritionist and body image coach.
People with idealized bodies sometimes aren’t living the life they want either, because they have to exhaust their energy to maintain an image of “perfection.”
(If you want to know what kind of sacrifices it takes to meet those “ideal” standards, check out: The cost of getting lean: Is it really worth the trade-off?)
“The ‘meh’ is the magic.”
That’s a quote from Jessi Kneeland, body neutrality coach and author of Body Neutral: A Revolutionary Guide to Overcoming Body Image Issues, when they sat down with some PN coaches to talk about body-neutrality.
(Want to listen in on the whole conversation? Watch it here: PN Coaches discuss body neutrality and negative self-talk)
The goal with body neutrality isn’t to love your body and all of its parts all of the time. Nor is it to be so toxically positive that you ignore real—and sometimes negative—feelings about your body.
That just isn’t realistic for most people.
Instead, an underrated goal is to feel sort of… meh.
You’re not overly glorifying or criticizing your body; its appearance just doesn’t hold that much importance.
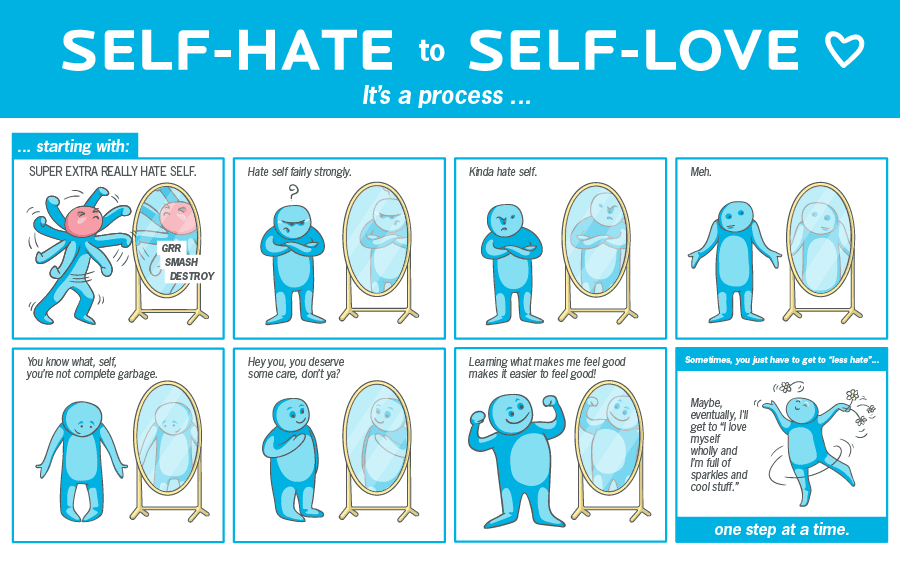
In practice, you may love certain parts about your body—but also feel ambivalent or mildly negative about other parts.
For example, you may see your stomach and feel ashamed because you don’t like what you see.
This feeling is uncomfortable, but it’s not “right” or “wrong.” You just don’t want that feeling to dictate your behavior. (Such as seeing your stomach and then saying, “Alright, I’m not going out tonight,” or, “Diet starts tomorrow!”)
To give you a personal example:
As a dude living in North America, I feel pretty ‘meh’ about being 5’9” tall.
Would I love to be 6’2”?
Sure.
But I’m not 6’2”—and I can’t change that. My height won’t ruin my day and I surely won’t be depriving myself from the things I enjoy most in this life because of it.
Body neutrality and aesthetic goals
Some people worry that if they adopt a more body neutral approach to their health and fitness, it means they have to relinquish any desire for physical change.
They also might worry that being more body neutral might make them lose certain aspects of their appearance that they like (such as muscular legs or a slim torso).
Here’s the thing: Body neutrality advocates for health.
Being body neutral doesn’t mean your body can’t change.
It just means your self-worth isn’t dependent on that change, and that your whole life isn’t consumed by the pursuit of a physique goal.
If you’ve been starving yourself and overexercising to the point of burnout, body neutral principles will encourage you to disengage from those extreme activities in the pursuit of a specific physique.
If you’ve been overeating and avoiding exercise because you can’t stand your body, body neutral principles will encourage you to tune into your genuine sense of care and love for yourself, and help you choose food and movement that support your body—regardless of its shape.
In this sense, body neutrality can have a balancing effect on health and fitness behaviors, and, according to Beer, is unlikely to take away from physical health, if applied correctly.
Plus…
There’s nothing inherently wrong with having an aesthetic goal.
Body neutrality rejects physical or aesthetic change only if it’s to the detriment of your overall mental, emotional, social, physical, and existential health.
5 things you can do today to be more body neutral
Congratulations: Just setting the intention to step away from an appearance-centric approach to health and fitness is a great start.
But, ultimately, it’s only action that creates deep, lasting change.
So, here are five tangible strategies you can work on immediately to develop a more body neutral approach.
Strategy #1: Do the things you love today.
Stop waiting to achieve the “ideal” body in order to be able to enjoy your life, and start doing more of what you love now.
Start with something easy that you tend to stop yourself from doing when you feel insecure about your appearance.
When I was in my worst spots, I stayed inside too much—even though I love being outside. It might sound silly but even reading outdoors in nice weather was helpful for me.
The point is: It can be that small.
Find one thing you’ve deprived yourself of in the past and do it—even if it’s a small dose, regardless of how you feel. Re-teach yourself that you don’t need a certain body shape or size to allow joy into your life.
(If you want more ideas on how to stop thinking you’re simply [insert thing you think you need] away from being happy, check out: “I’ll be happier when I lose weight” is a recipe for regret. Here’s the counterintuitive solution)
Strategy #2: Set body-neutral goals.
This is a gamechanger in my coaching experience. I’ve seen clients transform their relationship with exercise when they focus more on what they can do as opposed to how they look. “I feel so much better but I haven’t lost any weight,” is a sentence I’ve heard repeatedly.
When you’re overly appearance-centered or focused on weight, you risk missing other indicators of progress—like how good you feel.
If your fitness goals tend to be aesthetic-centric, try setting a goal that has nothing to do with how you look.
This can look like:
 Setting strength and performance goals in fitness (such as beating a deadlift PR, or a sprint time)
Setting strength and performance goals in fitness (such as beating a deadlift PR, or a sprint time)
 Practicing slow, mindful eating at more meals (if you usually inhale your meals in seven minutes tops, see if you can make a meal last 20 minutes, chewing your food well and savoring each bite)
Practicing slow, mindful eating at more meals (if you usually inhale your meals in seven minutes tops, see if you can make a meal last 20 minutes, chewing your food well and savoring each bite)
 Working to develop a new a skill in the gym (like your first pull-up, or a cool Olympic lift, like a clean and jerk)
Working to develop a new a skill in the gym (like your first pull-up, or a cool Olympic lift, like a clean and jerk)
None of these depend on your appearance; They’re all focused on what you can do. (And chances are, you’ll feel more empowered than ever when you start achieving them.)
Strategy #3: Curate your environment.
Take control of the parts of your environment that feed the body-image obsessed wolf. Starve that beast wherever you can.
Here are some ideas:
 Unfollow social media accounts that prey on insecurity or promote unrealistic ideals. Follow more that are body-neutral, or inspire other aspects of your personality (like comedy, or crafting).
Unfollow social media accounts that prey on insecurity or promote unrealistic ideals. Follow more that are body-neutral, or inspire other aspects of your personality (like comedy, or crafting).
 See what it’s like to reduce your exposure to your own appearance. This can look like having fewer mirrors (or covering some up for a period of time), or turning off the self-view on Zoom.
See what it’s like to reduce your exposure to your own appearance. This can look like having fewer mirrors (or covering some up for a period of time), or turning off the self-view on Zoom.
 Consider ditching the scale. Most people struggle to stay “neutral” about whatever number that shows up.
Consider ditching the scale. Most people struggle to stay “neutral” about whatever number that shows up.
 Set boundaries around body talk. Some environments are rife with commentary about body hang ups or goals. If someone begins talking about their new weight loss diet or “disgusting gut,” try changing the topic, or just exit the conversation. Eventually, people will realize you’re not the right audience.
Set boundaries around body talk. Some environments are rife with commentary about body hang ups or goals. If someone begins talking about their new weight loss diet or “disgusting gut,” try changing the topic, or just exit the conversation. Eventually, people will realize you’re not the right audience.
Strategy #4: Find your people.
Body neutrality won’t be the most common approach you’ll run into in the fitness world.
But, intentionally seeking out and surrounding yourself with more body neutral folks can keep you from constantly getting sucked back into an appearance-centric mindset.
There are body neutral, body positive, or HAES (health at every size) community groups all over social media and the internet, and this can be parlayed into finding local groups near you too.
Seeking out these spaces will only provide more support—and positive momentum—as you pursue a more body neutral approach.
Strategy #5: Strive for improvement, not perfection.
You don’t need to be a body-neutral icon or master. The expectation is not that you 100 percent divest from focusing on your appearance.
Body neutrality exists on a continuum.
Assess where you are right now in terms of how appearance-centric you are when it comes to health and fitness. If all your eggs are in the “aesthetics basket,” then even taking one metaphorical egg out (and say, putting it in the “gardening” basket) is progress.
Use the list of suggestions above to set some small goals, and just begin where you can.
You might always care about your appearance (maybe even more than average), but if it’s progress from where you started, you’re winning.
What life on “the other side” looks like
Even after sharing all of this, I won’t sit here and lie to you by saying I’m pure-bred body-neutral, all the time.
But I like to think I’ve grown a lot since my days of hiding out inside during “fat days.”
I’m better at doing the things I love, even when I don’t feel confident in my body.
I’m better at wearing comfortable clothing when I don’t feel good about my body— instead of cramming myself into something that’s too tight and suffering all day.
And, I’ve expanded the way I see fitness for myself and my clients, focusing more on feel and function, rather than achieving a certain look.
For me, this is progress.
Yours might look different.
Be kind to yourself, and acknowledge that you might be working through decades of programming. Body neutrality sure isn’t a quick fix, but the lasting freedom, joy, and genuine sense of self-worth it offers is worth it.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.
The post Too focused on how you look? Body neutrality might be your key to body image freedom appeared first on Precision Nutrition.
Source: Health1
Everyone needs a team.
As a health coach, you can become an expert in multiple areas: nutrition, behavior change psychology, fitness and athletic performance, stress management and recovery, and more.
However, no matter how many certifications you earn, you’ll invariably encounter clients with progress-blocking problems you don’t have the skills, training, expertise, or legal right to solve.
Here’s the thing…
You may not be an expert at fixing marriages, treating GERD, or counseling someone with an eating disorder, but someone else is.
Here’s where a healthy referral network comes in.
By connecting your client with such a person, you get to stay within your scope of practice, give welcome business to respected colleagues, and help your client solve their problem.
(Total. Supercoach. Move.)
All of our certification programs include sections devoted to teaching coaches how to build robust referral networks of professionals skilled at solving common client problems.
In this article, we’ll discuss how to do that—by exploring the top mistakes we see coaches make. Avoid them, and you’ll be able to refer out with confidence.
First, what’s a referral network?
A referral network is a list of supplementary professionals, businesses, and resources that benefit clients.
Your network might include local or virtual:
- Medical doctors, psychologists, registered dietitians, and other professionals with the training and credentials to help clients with problems outside of your scope of practice. (For an in-depth refresher, see our Scope of Practice worksheet.)
- Fellow health coaches and personal trainers with deep knowledge in an area outside your experience. (For example, maybe a client is interested in learning yoga, but you haven’t the faintest idea of how to salute the sun.)
- Workshops, fitness groups, webinars, food services, and other resources that support clients during their behavior change journey.
To confidently refer clients to skilled practitioners with excellent reputations, you’ll want to do some legwork. That brings us to the top mistakes to avoid.
Mistake #1: You build your network before launching your business.
For recently certified health coaches, the task “create a referral network” can double as a procrastination tool, says PN’s Director of Community Engagement Kate Solovieva.
Rather than take on clients, these coaches search for an increasing number of professionals, valiantly trying to be prepared for every potential referral situation. Yet, as much as they continue to work on it, their list is never “complete.”
That’s because…
“We can’t be prepared for everything,” says Solovieva.
The solution
Take on clients as soon as you’re certified.
Yes! That might sound scary, but the best way to figure out your “gaps” is to begin your practice, and see where your clients actually need help beyond what you can offer.
Add folks to your referral network over time as you:
- Connect with professionals on LinkedIn and other virtual networking sites
- Lean into peer networks (such as the Precision Nutrition Facebook communities)
- Mingle with members of your local Chamber of Commerce
- Chat with family, friends, and clients about professionals and resources they love
- Attend health conventions and other local events where a variety of health professionals tend to congregate
- Search for (and try out!) providers based on your own health needs
Who belongs in your referral network?
Use the following resource list as inspiration.
| Resource | Name | Website | Contact information |
| Acupuncturist | |||
| Chiropractor | |||
| Cooking class | |||
| Cycling, hiking, walking, or running club | |||
| Exercise physiologist | |||
| Coach who specializes in plant-based diets / pre- or post-natal fitness / other coaching niche you don’t cater to | |||
| Marriage / family counselor | |||
| Massage therapist | |||
| Meal delivery service | |||
| Mental health professional | |||
| Orthopedist | |||
| Pelvic floor therapist | |||
| Primary care physician | |||
| Physiotherapist | |||
| Registered dietitian | |||
| Stress management class | |||
| Other |
Mistake #2: You assume your referral list will cover all client needs.
As we mentioned above, you’ll never be able to anticipate every referral or client question ahead of time—and that’s okay.
This is especially true if you coach virtually with clients worldwide.
(You might know three fantastic massage therapists where you live in Toronto, Canada, but that knowledge won’t help if your client is based in Wellington, New Zealand.)
Similarly, some professionals or resources might work for some clients, but not others.
(You might, for example, know of several meal delivery options, yet none are suitable for that plant-based client who’s on a strict gluten-free diet.)
The solution
Learn how to help clients find the professionals and resources they need.
You might:
- Ask clients to describe their preferences. (Do they prefer working with a specific gender? Do they want to meet in person or online? Do they like the eagerness and creativity of a newer professional, or the “I’ve seen it all” sageness of a more seasoned pro?)
- Devote a coaching session to searching online for potential professionals and services together.
- Encourage clients to contact three practitioners, ask questions, and use what they learn to pick a winner.
Mistake #3: You let social awkwardness derail networking opportunities.
Reaching out to a stranger requires some bravery. You have to put yourself out there, explain who you are and what your motives are, and risk being ignored or turned down.
This is where many coaches get stuck, says Toni Bauer, PN’s Director of Coaching and Education Operations.
As a result, many coaches may put off the conversation.
The solution
Turn networking into a challenge. Coach Solovieva calls it “Operation 100.”
- Set a goal to contact 100 professionals over 12 months.
- Work toward your goal every week for about 20 minutes.
- Follow up with each non-responder once or twice.
- Instead of expecting a “yes” from every person you approach, understand that only about 10 percent of people will get back to you.
To ease yourself into the challenge, draft your elevator pitch, suggests Bauer.
Don’t overthink this. Your pitch doesn’t have to be a multi-page persuasive essay. Nor does it have to contain magical talking points. Just be yourself.
The elevator pitch: How to introduce yourself to a potential referral
As you work on your elevator pitch, use the examples below for inspiration.
“I’m a health coach who works with corporate executives. However, some of my clients would benefit from someone with your expertise. I would like to recommend you to my clients as those needs arise. Are you open to that?”
Or:
“I’m a health coach who works with athletes. Occasionally, my clients need guidance that I can’t always provide. I admire the work you’re doing, and I’d love to be able to refer people to you. If you’re open to that, could we have a quick 15- or 20-minute meeting to discuss what that arrangement would look like?”
Or simply:
“I’m a health coach and I’m building a referral list of practitioners. I would love to refer clients to you. Are you taking new patients right now?”
Mistake #4: You use dated persuasion tactics.
If you use LinkedIn, then you’ve likely been on the receiving end of old-school cold sales tactics. We’re talking direct messages from strangers who clearly haven’t read anything on your profile and know nothing about you.
These spammy messages are as welcome as a stranger who sidles up to you at a bar and says, “So, wanna come back to my place?”
We’re not here to discourage you from using cold outreach. It has a place. However, to increase your response rate, we’d like to introduce you to a rarely used technique.
The solution
Get to know people before making an online ask, suggests Coach Solovieva.
Follow them, read their content, download and consume their free resources, comment on their posts, congratulate them on career wins, and become a part of their online life.
Do that, and people will remember you. More of them will respond to your messages, too. Plus, the intel you gather by forming a relationship will help you avoid…
Mistake #5: You don’t personally vet referrals.
How do you ensure you refer clients to compassionate professionals who truly know what they’re doing?
It involves more than checking someone’s website or social media profile.
If you only look at someone’s website or social media posts, “You’re just vetting their confidence and copywriting skills,” says Solovieva. “If we’re fortunate, confidence and copywriting go hand in hand with ability, but not always.”
The solution
Try out their services. Take someone’s yoga or Zumba class. Book a massage. Ask a medical professional to look at your creaky knee.
That way, you can see the professional in action.
If you’re thinking, ‘I don’t need some of the services my clients need!’ you’ve got a couple of options:
- Offer to pay a professional to meet with you for 30 to 60 minutes so you can ask some questions, get a sense of their treatment philosophy, and chat about referring clients to them.
- Interact with people in local social networking communities like NextDoor.com. Ask group members if they’ve seen a practitioner and, if so, whether they’d recommend the person.
Mistake #6: You sell clients too hard on your referrals.
When you recommend a professional you’ve personally vetted, it’s natural to want your client to take action.
However, despite your hard work, some clients just won’t make an appointment with the professional in question—and that’s okay.
“Let your clients be adults,” says Coach Bauer.
Clients have their reasons. Maybe their insurance won’t cover the service in question. Or, maybe they decided to see someone else.
“It’s not your responsibility for the relationships to be perfect or to flourish,“ says Bauer.
A cycle of support
Some coaches fear referrals because they see them as “giving business away.”
In reality, however, when you refer clients to solid pros, your clients simply feel like you have their back. (Which means they’ll be more likely to refer friends and family to you.)
Plus, when you send business towards another respected colleague, it also puts you on their radar for a cross-referral.
It’s good for your clients, good for business, and good for your community of health pros at large.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.
The post How to build a referral network with confidence appeared first on Precision Nutrition.
Source: Health1
There’s been a growing shift in the fitness, health, and wellness industry.
The promise of “immediate results” will probably never lose its sparkle.
But, as a good portion of our population (hi, Boomers!) moves into their “silver” years, conversations around optimizing lifespan (how long you live) and healthspan (how long you live with a high quality of life) are also on the rise.
People are more interested than ever in longevity, which, these days, means the combination of a long lifespan and a long healthspan. (Historically, longevity and lifespan were synonymous.)
Trending too is the concept of biological age—essentially, how “old” your cells are, determined by their health and functioning. (Compare this to chronological age, which just refers to how many years you’ve been on this planet.)
Increasingly, people want to improve their overall health—for the long haul.
Of course, the wellness market is responding to this trend with supplements, ultra-specific diet plans, I.V. therapy, cold plunges, and other fringe modalities that promise to reduce or slow biological aging.
While some of these therapies are questionable, the movement that inspired them is great; For many of us in the health and fitness industry, the shift toward holistic health and long-term wellbeing is a welcome one.
At PN, we’ve held and promoted this expanded view of health for a while now.
We call it Deep Health
Deep Health is a “whole-person, whole-life” phenomenon that involves thriving in all dimensions of the human experience.
This framework of health includes six interdependent dimensions that influence and interact with each other.
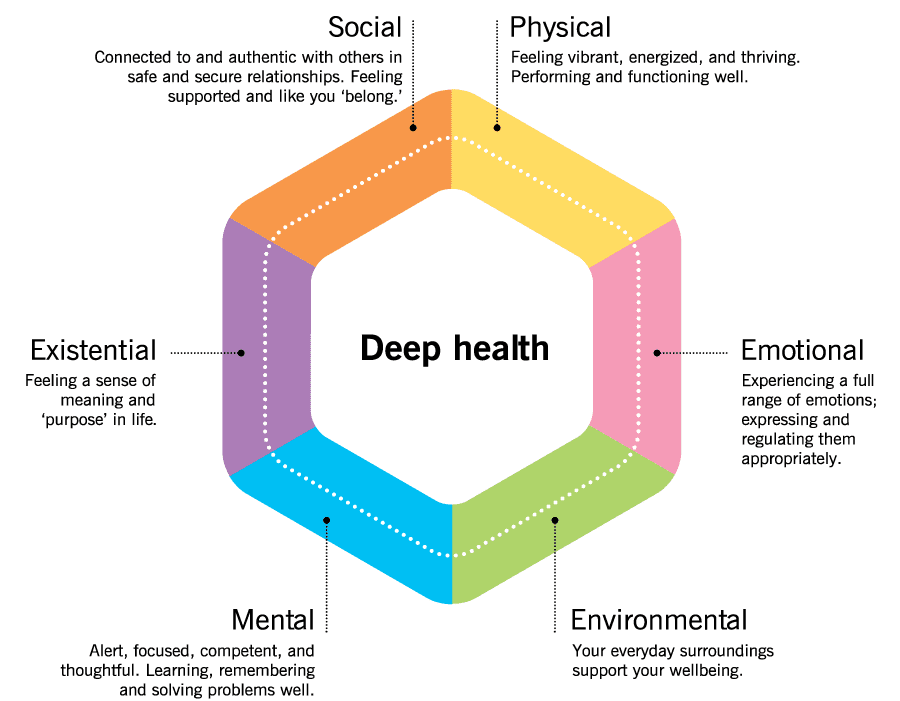
These six dimensions are:
 Physical health
Physical health
The one we all know best, and what people have historically thought of when thinking about health.
This is how your body feels, functions, and performs.
We measure physical health with blood work—such as your cholesterol and hormone levels and your blood pressure—as well as performance metrics like V02 max and demonstrations of strength, and subjective measures like energy and pain levels.
 Emotional health
Emotional health
This is about feeling a full range of emotions, but having more positive than negative feelings.
You can recognize, regulate, and appropriately express your emotions directly, maturely, and honestly. You have the resilience to recover from strong emotions, and calm yourself when you become stressed, anxious, or upset.
 Environmental health
Environmental health
This is about being and feeling safe and secure, as well as being and feeling supported by your everyday surroundings.
You have access to resources (health care, healthy food, clean air and water, nature) that support your goals and wellbeing.
 Mental or cognitive health
Mental or cognitive health
This is related to how well you think, learn, remember, and creatively problem-solve.
Your mind is sharp, and you’re able to be your most productive and do your best thinking.
This dimension also includes your mindset, capacity for insight, and your perspective and outlook on the world.
 Existential or purposeful health
Existential or purposeful health
Some might think of this as spiritual or soul health.
You have a deeper “why” or purpose for your life; you feel part of a “bigger picture.”
You have a strong sense of yourself and your intrinsic self-worth. You work to fulfill your purpose by choosing behaviors that align with your identity and values.
 Social or relational health
Social or relational health
This is about connecting and interacting well with others.
You develop and maintain authentic, fulfilling relationships. You have a sense of belonging, and you feel respected, “seen,” valued, and supported by others.
If you have Deep Health, it’s almost a guarantee…
You’re experiencing a life well-lived. A vibrant, thriving life that’s healthy in every sense of the word.
Not surprisingly, such a life is also statistically more likely to last longer, with more of those years being enjoyable.
(For more on Deep Health, plus how you can use the concept to transform your own—or your clients’—health, read: The “Deep Health” coaching secret)
High-impact habits to boost Deep Health (and by extension healthspan, longevity, and biological age)
While there are many things that can impact healthspan, longevity, and biological age, the following will give you the best return on investment.
These aren’t always the “sexiest” actions, nor are they likely to sound “cutting edge” (partly because they’ve been tested by time and robustly proven by decades of research).
But—if you’re looking to maximize Deep Health for as long as possible—they’re the things worth spending your time on.
The most important thing is being active.
If there’s a “magical panacea” out there, it’s exercise.
Before you start beating yourself up for not being “a gym person”…
…Any activity helps…
…At any dose.
Whether you clean your yard, vacuum, play games with your pets or kids, or just do a little walking, tell yourself, “I’m doing great!”
Because you are. These activities make a positive, measurable difference.
If you want to level up, get in a mix of aerobic or cardiovascular exercise, strength training, and stability work (like yoga, tai chi, or balance-challenging exercises).
Again, these can be in whatever amounts you can, in ways you enjoy.
For quintuple stars, aim for at least 150 minutes per week of moderate aerobic exercise (or 75 minutes of intense aerobic exercise), plus two or more strength and stability training sessions per week. (If you do these activities with friends—bonus!—now you’re boosting social health too.)
In general, the more activity the better. (So long as you enjoy it—and your body is recovering adequately.)
A thoughtful diet—and a mindful approach to other substances—is big, too.
Rather than focus on food you “shouldn’t be eating,” center your attention on the abundance of foods that serve your health and wellbeing.
We’re talking:
- Lean proteins (which can come from animals and/or plants, like fish, chicken, tofu, eggs, tempeh, Greek yogurt)
- A rainbow of fruits and vegetables (fact: different colors provide different nutrients and benefits, so aim to eat all of the colors regularly)
- Minimally-processed carbohydrates (whole grains, beans and lentils, starchy tubers like potatoes and sweet potatoes, and winter squash)
- Healthy fats (from nuts, seeds, avocados, extra virgin olive oil, nut butters, and a little dark chocolate)
For help choosing higher-quality versions and a wide variety of the above categories, check out one of our most popular infographics: ‘What should I eat?!’ Our 3-step guide for choosing the best foods for your body
To stay hydrated, drink plenty of water. For variety, emphasize mostly zero-calorie drinks like unsweetened tea and coffee. (If you’re confused about how much fluid to drink every day, you’ll love the “pee chart” in this article: ‘How much water should I drink?’)
Avoid smoking or chewing tobacco, and if you drink alcohol, do so lightly to moderately.
And of course, getting quality sleep and regulating stress makes everything better.
Get enough quality sleep by prioritizing and protecting the time you rest.
Make your sleeping area as comfortable, quiet, and dark as possible. Figure out when you need to get to bed to get seven to eight hours of sleep, and ideally, start winding down with a relaxing bedtime ritual about half an hour to an hour before that time.
(Want to learn more about why sleep is so important—and how to get more of it? Check out our infographic: The power of sleep)
To build your emotional resilience and stress tolerance, incorporate soothing, self-regulating activities daily.
These activities are somewhat subjective (some people find it relaxing to sit and meditate, while others find it to be an opportunity for restless anxiety to boil over). However, “crowd favorites” include: breathing exercises, time in nature, various forms of self-expression (journaling, art, movement), or just a good soak in the tub.
One of the most important mindsets to adopt to help your mental and emotional health—although it can benefit all areas of life—is a growth mindset.
People with a growth mindset tend to view challenges and adversity as opportunities to grow, evolve, and learn. And turns out, this kind of perspective isn’t just good for your mental and emotional health, it boosts longevity, too.
Research shows that, compared to less optimistic individuals, those with a more positive attitude and a growth mindset about aging had a 43 percent lower risk of dying from any cause, and lived about 7.5 years longer.1 2
Lastly, don’t underestimate the power of finding your people—and a purpose.
Seeking and nurturing positive, supportive relationships is one of the best things you can do for your health.
And not just for your social health. Research shows that people who are satisfied with their relationships have better emotional health,3 cognitive health,4 and even physical health.5
In fact, one of the longest studies on human health—the Harvard Study of Adult Development, which tracked participants for nearly 80 years—showed that feeling happy and satisfied in one’s relationships was one of the best predictors of overall health, happiness, and longevity.6
(Feel like your social health could use a boost? We’ve got three strategies to improve connection in your life, right here: Is social health the secret to total-body health?)
Having a strong sense of purpose bolsters our health and longevity too.7 8
Interestingly, a sense of purpose seems to help people live longer, even when controlling for other markers of psychological well-being. So there’s something uniquely beneficial about having a strong purpose that’s different from, say, being happy.
A purpose can take time to uncover, but you can facilitate that discovery by devoting regular time to the “big questions” in life:
- Who are you, really?
- What do you want your life to be about?
- How do you want to live?
- More practically: What gets you out of bed in the morning? (Is it your family, or showing up for your clients? Or something else?)
But Deep Health isn’t just something you want to achieve—it also serves as a framework to help you make choices.
When you understand how Deep Health works, it can also help you answer the often vague and perplexing question, “How can I feel better?”
Knowing about your own Deep Health can tell you which area of your life to prioritize right now that will make the biggest impact on your overall health.
How to use Deep Health to help you prioritize next actions.
Start by assessing your current Deep Health to get a baseline status. Click on the image below to access your own free assessment.

© Precision Nutrition
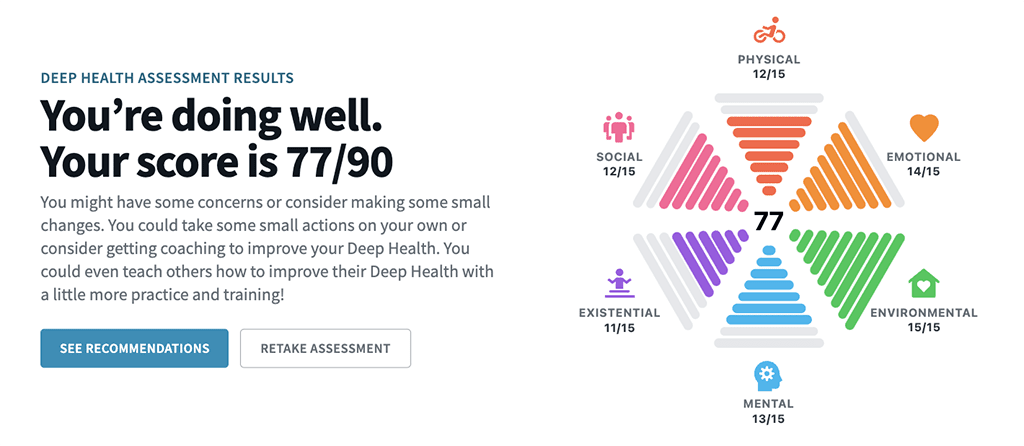
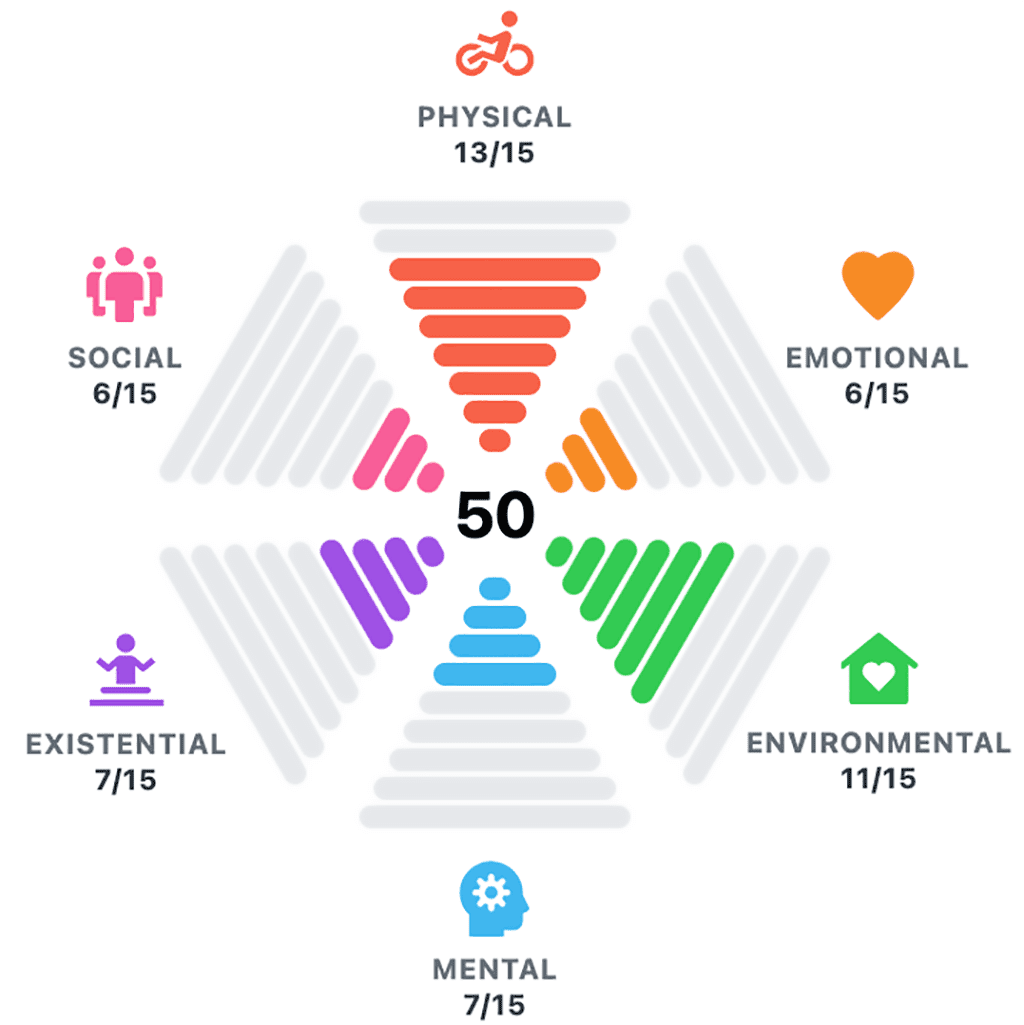
Depending on what’s going on in your life right now, you might get a Deep Health score that looks like this:
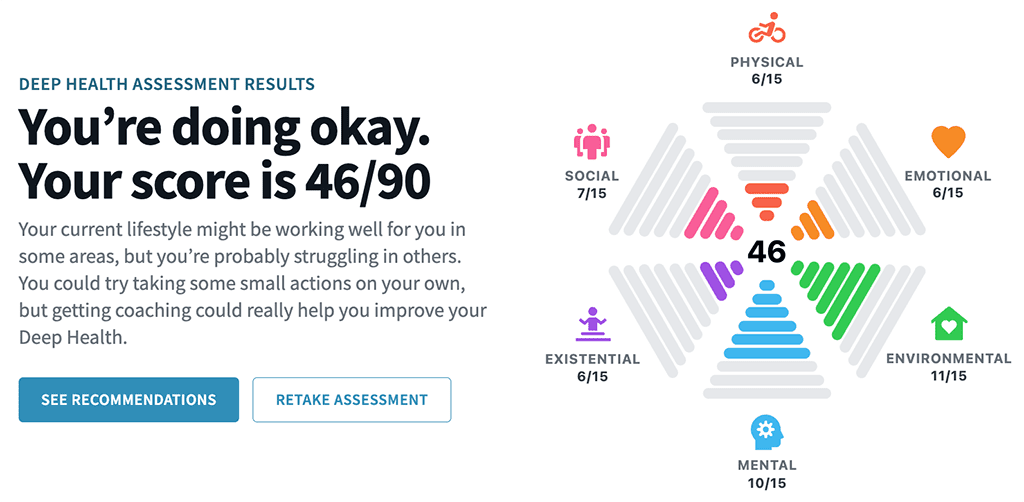
Or like this:
Or this:
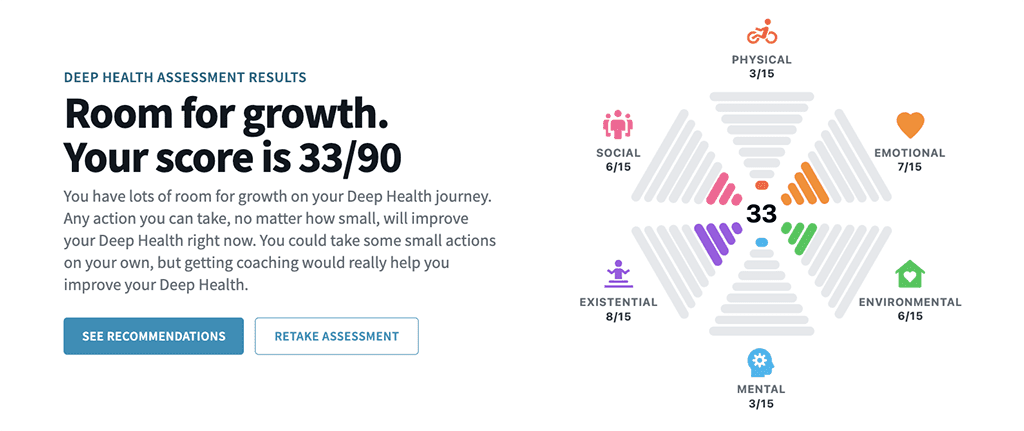
Whatever your results (and no judgment on the numbers), the distribution of your score can tell you:
- Where you’re currently thriving
- Where you have the largest opportunities for growth and improvement
- Where you might be able to make some easy improvements
- Which dimensions, if you improve them, might best help you reach (and sustain) your goals
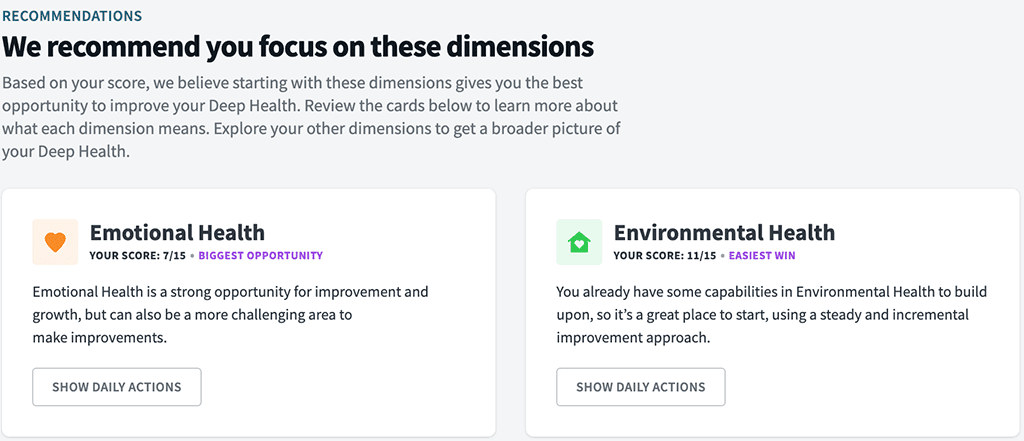
Your personalized assessment will make some suggestions. (The below is a sample screenshot.)
But of course, it’s entirely up to you where you decide to focus, and what actions you choose to take next—if any.
Let’s walk through an example
Let’s say you’ve recently become interested in optimizing health and longevity.
You’ve been listening to podcasts, you’ve read the articles about people “reversing” their biological age, and you feel fired up about it.
You haven’t felt so passionate or inspired about your health in a long time, and you’re excited to try some of the strategies recommended in those podcasts and articles. (You want to be 27 again! At least, your cells do.)
At the beginning of this journey, let’s imagine your Deep Health looks like this:
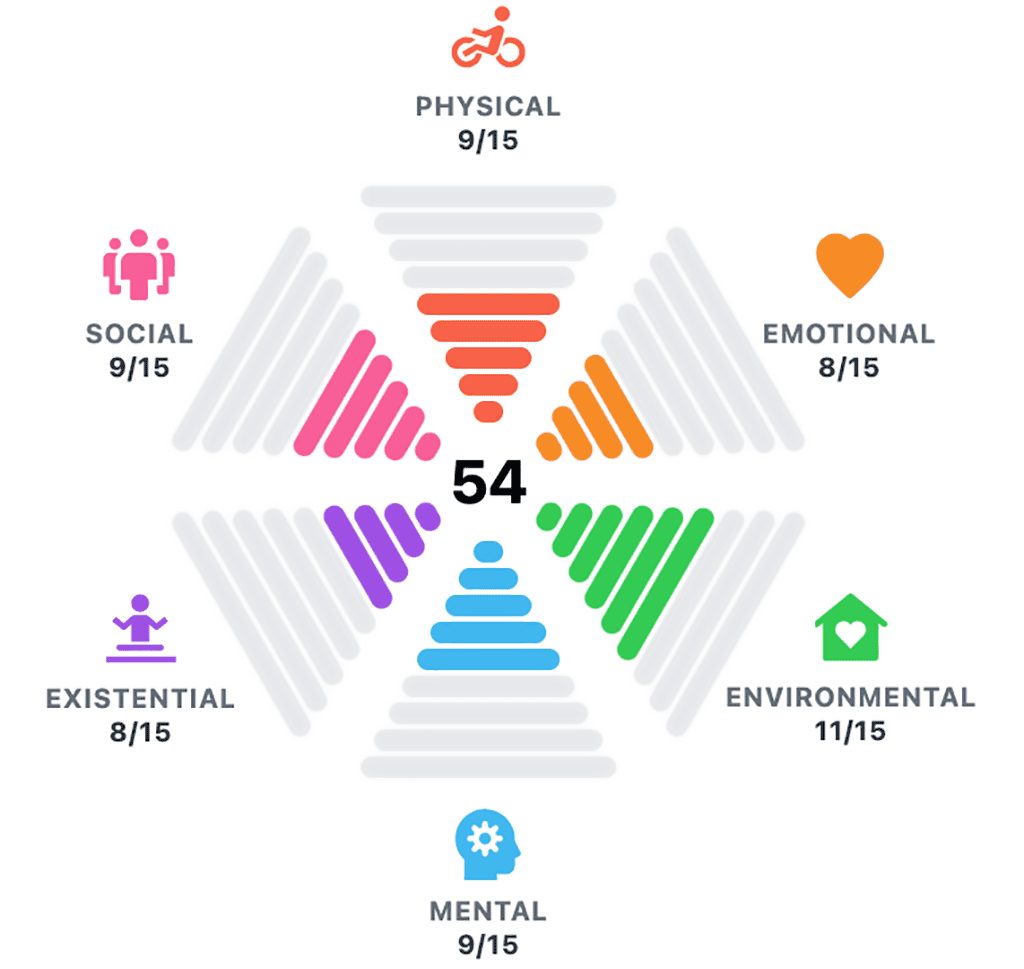
Kind of “so-so” all around. Definitely, there’s room for improvement.
Of course, in reality, there’s infinite pathways you could take. But let’s imagine two scenarios…
Scenario A: Biohack like a beast
After seeing your Deep Health score, you decide to simply tackle everything at once:
- You subscribe to a longevity-boosting supplement program, that has you taking about 20 different tablets and powdered elixirs per day.
- You start practicing 16:8 fasting (in each 24-hour cycle, you fast for 16 hours, and eat within an 8 hour window), eating only two meals per day.
- You start eating fully plant-based, getting in tons of veggies, fruits, and legumes, and start tracking your macros meticulously.
- You incorporate four 45-minute zone 2 cardio workouts a week (you heard that’s the amount needed to see significant benefit to your mitochondria).
- You also add two 60-minute resistance training sessions a week.
- You start taking cold plunges at the gym multiple times per week, and are even considering buying a cold plunge tank for your home.
For two weeks, you feel on top of the world.
Then, not so much. (You’ve actually grown to hate that green sludgy stuff you drink every morning.)
You continue to show up anyway with a gritty determination, and for months, follow your protocol as best as you can.
You forego social events, finding yourself grouchy and irritable. (When everyone else is munching on buttery canapés, you’re counting down the hours until your next feeding window.)
Every day feels like a Sisyphean effort, and you begin to wonder what the point of all of it is. You can’t imagine doing this for the rest of your life, which you’re (now ironically) trying to extend.
Eventually, all this white-knuckling in pursuit of optimal health starts to take a toll. On you, your marriage, your social life, and your mental and emotional wellbeing. And you want to know if all of this effort and suffering are worth it.
After several grueling months, you gather some data.
Your blood work looks awesome. You’re definitely leaner. And your biological age test tells you your rate of aging has slowed and your cells have gotten younger.
You’re… winning?
You decide to reassess your Deep Health, and it looks like this:
Your physical health has gone way up, but your emotional, social, mental, and existential health have all gone down. Overall, your Deep Health is somehow worse! (Argh!)
It becomes clear to you: While your “do all the things” protocol might help you live longer—it’s definitely not helping you live better.
Scenario B: Dig deep for Deep Health
In this scenario, you take a different approach.
Seeing your Deep Health starting point, you consider that list of “high impact habits” above.
You’re not sure which one to start with though, so you take some time to think about why you’re really interested in this whole longevity thing.
What’s your deeper purpose for wanting to live a longer, healthier life?
You think about your family, and tears come to your eyes when you conjure up the thought of your children having children, and imagining yourself tumbling around with a bunch of rambunctious grandkids. You want to be healthy, strong, and capable of playing with them.
This deep purpose aligns with your identity too. You’ve always been a “family guy,” and now you add a new layer on top of that: You decide to become the kind of person who makes their health and wellbeing a priority, so they can be there for their family for as long as possible.
With this new, revised identity and a clear purpose in mind, you begin to make some changes over time.
- You focus on eating protein at most every meal, and up your fruit and vegetable game too.
- You practice self-compassion when you can’t or just don’t get in as much protein or produce as you’d like. You also work on viewing your choices on a continuum—rather than simply “good” or “bad.” This flexibility helps you feel a sense of freedom in your diet, and feels a little more realistic, long-term.
- Instead of going for the “perfect” four cardio sessions, you aim for two a week, for as long as you can fit in (which sometimes is only 20 minutes, but you do your best). Any extra sessions are a bonus.
- You’re diligent with your resistance training, but you cap them at 30-45 minutes, twice per week (occasionally you only have 20 minutes for these sessions too, but you focus on consistency over perfection).
- You begin going for outdoor walks after dinner with your partner—sometimes inviting a few neighborhood friends, too—and enjoy the deep yet fun conversations you have about work, family, and life (and, let’s be honest, some good neighborhood gossip).
After several satisfying months, you gather some data.
Your blood work has improved. You’ve leaned out a touch too. Your rate of aging has also slowed and your biological age has decreased, seemingly just as much as Scenario A.
But the biggest difference: You enjoyed this process.
You found it not only physically beneficial, but also socially enriching, mentally and emotionally enlightening, and deeply meaningful.
You reassess your Deep Health, and it looks like this:
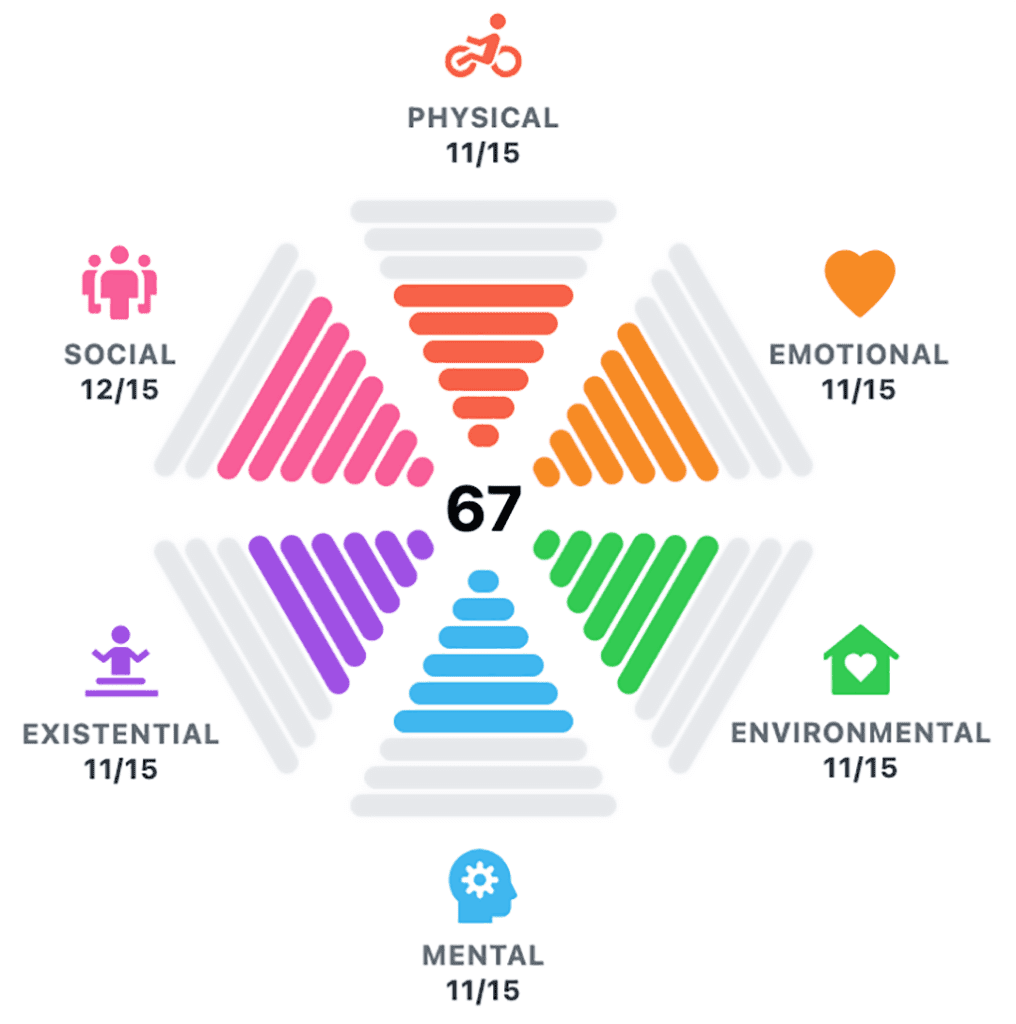
Your physical health has gone up (though not quite as high as Scenario A), and so has your emotional, social, mental, and existential health. Your overall Deep Health is now undeniably, significantly up.
The funny thing: It didn’t even seem that hard.
Moreover, you feel more inspired and energized than ever to take even more steps to further invest in your health and wellbeing.
This is the power of Deep Health.
It’s not just about improving your biological age or increasing your healthspan (which mostly center on physical health metrics).
Striving for Deep Health means working to thrive in ALL areas of your life—not just the physical. Because no single aspect of your health functions alone.
With the push towards longevity and healthspan, and the focus on things like biological age and “biohacking” for optimal aging, it can be easy to forget that we already know the fundamentals of what it means to experience a life well lived.
The truth is, scientists don’t know everything that improves our biological age. Or even the best ways to measure it.
However, if you’re thriving in all dimensions of your health and wellbeing—in other words, achieving Deep Health—you can bet you’re doing all of the things that matter most in living a long, healthy, rewarding life.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Nakamura, Julia S., Joanna H. Hong, Jacqui Smith, William J. Chopik, Ying Chen, Tyler J. VanderWeele, and Eric S. Kim. 2022. “Associations between Satisfaction with Aging and Health and Well-Being Outcomes among Older US Adults.” JAMA Network Open 5 (2): e2147797.
2. Levy, Becca R., Martin D. Slade, Suzanne R. Kunkel, and Stanislav V. Kasl. 2002. “Longevity Increased by Positive Self-Perceptions of Aging.” Journal of Personality and Social Psychology 83 (2): 261–70.
3. Block, Victoria J., Elisa Haller, Jeanette Villanueva, Andrea Meyer, Charles Benoy, Marc Walter, Undine E. Lang, and Andrew T. Gloster. 2022. “Meaningful Relationships in Community and Clinical Samples: Their Importance for Mental Health.” Frontiers in Psychology 13 (May): 832520.
4. Cook Maher, Amanda, Stephanie Kielb, Emmaleigh Loyer, Maureen Connelley, Alfred Rademaker, M-Marsel Mesulam, Sandra Weintraub, Dan McAdams, Regina Logan, and Emily Rogalski. 2017. “Psychological Well-Being in Elderly Adults with Extraordinary Episodic Memory.” PloS One 12 (10): e0186413.
5. Holt-Lunstad, Julianne, Timothy B. Smith, and J. Bradley Layton. 2010. “Social Relationships and Mortality Risk: A Meta-Analytic Review.” PLoS Medicine 7 (7): e1000316.
6. “Harvard Second Generation Study.” n.d. Harvardstudy. Accessed May 16, 2024. https://www.adultdevelopmentstudy.org/
7. Shiba, Koichiro, Laura D. Kubzansky, David R. Williams, Tyler J. VanderWeele, and Eric S. Kim. 2022. “Purpose in Life and 8-Year Mortality by Gender and Race/Ethnicity among Older Adults in the U.S.” Preventive Medicine 164 (107310): 107310.
8. Hill, Patrick L., and Nicholas A. Turiano. 2014. “Purpose in Life as a Predictor of Mortality across Adulthood.” Psychological Science 25 (7): 1482–86.
If you’re a coach, or you want to be…
You can help people build sustainable nutrition and lifestyle habits that will significantly improve their physical and mental health—while you make a great living doing what you love. We’ll show you how.
If you’d like to learn more, consider the PN Level 1 Nutrition Coaching Certification.
The post The PN framework that improves healthspan, longevity, and quality of life appeared first on Precision Nutrition.
Source: Health1
If you live in a larger body, sometimes it feels like you can’t win.
If you don’t lose weight, people will criticize you for being “lazy,” “unhealthy,” or “lacking willpower.”
But if you take medication to help you, you’ll be criticized for “cheating” or “taking the easy way out,” even if you’ve tried for decades to manage your weight through diet, exercise, and lifestyle changes (sometimes extreme ones).
In this article, we’ll be talking about a highly contentious group of medicines—GLP-1 receptor agonist drugs such as semaglutide (Ozempic, Wegovy, Rybelsus) or tirzepatide (Mounjaro, Zepbound).
And people have lots of opinions about them.
But the opinion that matters most? Yours.
At PN, we’re medication agnostic.
We’re not here to judge whether a person should or should not take medication for weight loss. Ultimately, that’s a choice left up to you, with the guidance of your primary care physician.
Either way, we’re here to support our clients and elevate their results.
Whether you take medication or not, a coach can help you optimize nutrition and satiety with the right foods, find exercises that work with your changing body, and help you navigate the emotional ups and downs that come when you attempt to tackle a big, meaningful, long-term goal.
However, we also understand that if you’re debating the pros and cons of beginning (or continuing) medication, you might have mixed feelings.
If you’re not sure if these new medicines are right for you, we have your back. In the following article, we’ll give you the honest, science-backed information you need to make a confident decision.
You’ll learn…
- Why it’s so hard to lose (and keep off) fat
- Why taking medication isn’t “cheating,” nor is it the “easy way out”
- How GLP-1 drugs work, and the health benefits they can have (aside from weight loss)
- How to determine if you’re at a “healthy weight” (it’s not just about BMI)
- What actions you can take to minimize side effects and maximize long-term health, if you do decide to take these medications
Let’s begin.
First, why is it so hard to lose fat?
Fat loss is hard. Period.
But for some people, it’s harder still—because of environmental, genetic, physiological, social, cultural, and/or behavioral factors that work against them.
Here are a few of the contributing factors that can make fat loss so challenging.
We live in an environment that encourages a caloric surplus.
Imagine life 150 years ago, before cars and public transit were invented. To get from point A to point B, you had to walk, pedal a bicycle, or ride a horse.
Food was often in short supply, too. You had to expend calories to get it, and meals would just satisfy you (but not leave you “full”).
Today, however…
“We live in an obesogenic environment that’s filled with cheap, highly-palatable, energy-dense foods [that make overeating calories easy, often unconsciously],” says Karl Nadolsky, MD, an endocrinologist and weight loss specialist at Holland Hospital and co-host of the Docs Who Lift podcast.
“We also have countless conveniences that reduce our physical activity.”
Of course, even in such an environment, we have people in lean bodies, just as we have people who struggle to stop the scale from continuously creeping up.
Why?
Genetically, some people are more predisposed to obesity.
Some genes can lead to severe obesity at a very early age. However, those are pretty rare.
Much more common is polygenic obesity—when two or more genes work together to predispose you to weight gain, especially when you’re exposed to the obesogenic environment mentioned earlier.
People who inherit one or more of these so-called obesity genes tend to have particularly persistent “I’m hungry” and “I’m not full yet” signals, says Dr. Nadolsky.
Obesity genes also seem to cause some people to experience what’s colloquially known as “food noise.”
They feel obsessed with food, continually thinking, “What am I going to eat next? When is my next meal? Can I eat now?”
Physiologically, bodies tend to resist fat loss.
If you gain a lot of fat, the hormones in your gut, fat cells, and brain can change how you experience hunger and fullness.
“It’s like a thermostat in a house, but now it’s broken,” says Dr. Nadolsky. “So when people cut calories and weight goes down, these physiologic factors work against them.”
After losing weight, your gut may continually send out the “I’m hungry” signal, even if you’ve recently eaten, and even if you have more than enough body fat to serve as a calorie reserve. It also might take more food for you to feel full than, say, someone else who’s never been at a higher weight.
Being in a larger body often means being the recipient of fat stigma and discriminatory treatment.
Until you’ve lived in a larger body, it’s hard to believe how different the world might treat you.
Our clients have told us stories about being bullied at the gym, openly judged or lectured at the grocery store, and otherwise being subjected to innumerable comments and assumptions about their body shape, health, and even worth.
Even in medical settings, people with obesity are more likely to receive poor treatment.1, 2 Healthcare providers may overlook or downplay symptoms, attributing health concerns solely to weight. This can lead to delayed- or missed diagnoses or just plain old inadequate care.
All of this combined can add up to an incredibly pervasive and ongoing source of stress.
This stress—in addition to being socially isolating and psychologically damaging—can further contribute to increased appetite and pleasure from high-calorie foods, decreased activity, and poorer sleep quality.3
Which is why…
Taking medication isn’t an “easy way out.”
In 2013, the American Medical Association categorized obesity as a disease.
And yet, many people still don’t treat it as such, and rather consider obesity as a willpower problem, and the consequence of simply eating too much and moving too little. (The remedy: “Just try harder.”)
In reality, people with obesity have as much willpower as anyone else.
However, for them, fat loss is harder—for all the reasons mentioned above, and more.
So, just like chemotherapy or insulin isn’t “the easy way out” of cancer or type 1 diabetes, medication isn’t “the easy way out” of obesity.
Rather, medication is a tool, ideally used alongside healthy lifestyle behaviors, that can help offset some of the genetic and physiological variances that people with obesity may have, and have little individual control over otherwise.
What you need to know about GLP-1 drugs
In 2017, semaglutide (a synthentic GLP-1 agonist) was approved in the US as an antidiabetic and anti-obesity medication.
With the emergence of this class of drugs, science offered people with obesity a relatively safe and accessible way to lose weight long-term, so long as they continued the medication.
How Ozempic and other obesity medicines work
Current weight loss medications work primarily by mimicking the function of glucagon-like peptide 1 (GLP-1), a hormone that performs several functions:
- In the pancreas, it triggers insulin secretion, which helps regulate blood sugar (and also helps you feel full).
- In the gut, it slows gastric emptying, affecting your sensation of fullness.
- In the brain, it reduces cravings (the desire for specific foods) and food noise (intrusive thoughts about food).
In people with obesity, the body quickly breaks down endogenous (natural) GLP-1, making it less effective. As a result, it takes longer to feel full, meals offer less staying power, and food noise becomes a near-constant companion, says Dr. Nadolsky.
Semaglutide and similar medicines flood the body with synthetically made GLP-1 that lasts much longer than the GLP-1 the body produces. This long-lasting effect helps increase feelings of fullness, reduce between-meal hunger, and muffle cravings and food noise.
Interestingly, by calming down the brain’s reward center (the part of the brain that drives cravings and even addictions), these medicines may also help people reduce addictive behaviors like compulsive drinking and gambling, says Dr. Nadolsky.
Note: Newer weight loss medicines, for example tirzepatide, mimic not only GLP-1, but also another hormone called gastric inhibitory polypeptide (GIP). Like GLP-1, GIP also stimulates post-meal insulin secretion and reduces appetite, partly by decreasing gastrointestinal activity. Other drugs soon to come on the market, like retatrutide, mimic a third hormone, glucagon.
How effective are GLP-1 drugs?
Researchers measure a weight loss medicine’s success based on the percentage of people who reach key weight loss milestones of 5, 10, 15, or 20 percent of their weight.
These medicines are still evolving, but so far, they have shown to be quite effective:
About 86 percent of people who take GLP-1 drugs like Ozempic, Rybelsus, and Wegovy lose at least five percent of their body weight, with about a third of them losing more than 20 percent of their body weight.4, 5
And newer generation versions of these medications—such as tirzepatide, and the not-yet-FDA-approved retatrutide—are only getting better, with up to 57 percent of people losing more than 20 percent of their body weight.6, 7
How do weight loss medications compare to lifestyle interventions?
In the past, weight loss interventions have focused on lifestyle modifications like calorie or macronutrient manipulation, exercise, and sometimes counseling.
Rather than pitting lifestyle changes against weight loss medicines or surgery, it’s more helpful to think of them all as compatible players.
With lifestyle modifications and coaching, the average person can expect to lose about five to 13 percent of their body weight.
When you add FDA-approved versions of GLP-1 and other weight-loss drugs to lifestyle and coaching, average weight loss jumps up another ten percent or more. 8, 9, 10, 11
Fat loss often comes with powerful health benefits
For years, the medical community has told folks that losing 5 to 10 percent of their body weight was good enough.
Partly, this message was designed to right-set people’s expectations, as few lose much more than that (and keep it off) with lifestyle changes alone.
In addition, this modest weight loss also leads to measurable health improvements. Lose 5 to 10 percent of your total weight, and you’ll start to see blood sugar, cholesterol, and pressure drop.12
However, losing 15 to 20 percent of your weight, as people tend to do when they combine lifestyle changes with second-generation GLP-1s, and you do much more than improve your health. You can go into remission for several health problems, including:
- High blood pressure
- Diabetes
- Fatty liver disease
- Sleep apnea
That means, by taking a GLP-1 medicine, you might be able eventually to stop taking several other drugs, says Dr. Nadolsky.
Experts suspect GLP-1s may improve health even when no weight loss occurs.
“The medicines seem to offer additive benefits beyond just weight reduction,” says Dr. Nadolsky.
Research indicates that GLP-1s may reduce the risk of major cardiovascular events (heart attacks and strokes) in people with diabetes or heart disease.13, 14, 15 In people with diabetes, they seem to improve kidney function, too.16
The theory is that organs throughout the body have GLP-1 receptors on their cells. When the GLP-1s attach to these receptors in the kidneys and heart, they seem to protect these organs from damage.
For this reason, in 2023, the American Heart Association listed GLP-1 receptor agonists as one of the year’s top advances in cardiovascular disease.
What even is a “healthy body weight”?
Many people say, “I just want to be at a healthy weight.”
But what does that even mean?
At PN, we believe your healthiest body composition / weight is one that:
- Has relatively more lean mass (from muscle and healthy, dense bones), and relatively less body fat
- Emerges from doing foundational, sustainable health-promoting behaviors (like being active and eating well), rather than “crash diets” or other extreme measures
- Is relatively easy to maintain with a handful of consistent lifestyle choices, without undue sacrifices to overall well-being (or what we call Deep Health)
- Allows you to do the activities you want and enjoy, with as few limitations as possible
- Keeps your health markers (like blood pressure, cholesterol, and blood sugar) in safe and healthy ranges as much as is reasonably possible
- Feels good to you
This is not a specific size, shape, look, body fat percentage, or category on a BMI chart; A “healthy” body composition and/or weight will vary from person to person.
… Which can be both freeing and frustrating to hear.
Without a specific number to aim for, it’s harder to know if you’ve “arrived” at your healthiest weight or body composition.
However, we like this way of qualifying what a healthy weight is because it takes the pressure off a number on the scale, and puts the focus on behaviors you have more control over, and more importantly, how your life feels.
7 strategies to make weight loss medicines more effective—and improve long-term health
Here’s what we believe:
Weight loss medicines don’t render lifestyle changes obsolete; they make them more critical.
When GLP-1 medicines muffle food noise and hunger, many find it easier to prioritize lean protein, fruits and veggies, whole grains, and other minimally processed foods. Similarly, as the scale goes down, people often feel better, so they’re more likely to embrace weight lifting and other forms of exercise.
Indeed, according to a 2024 consumer trends survey, 41 percent of GLP-1 medicine users reported that their exercise frequency increased since going on the medication. The majority of them also reported an improvement in diet quality, choosing to eat more protein, as well as fruits and vegetables.17
This is great news, because it further reinforces the idea that medication isn’t simply “the easy way out.”
(Of course, sometimes drugs are used as “the easy way out”; After going on medication, people can continue to eat poor quality food—just less of it. This increases the risk of losing critical muscle and bone, and losing less—or even no—body fat.)
When used correctly, weight loss medication is a tool that, as mentioned above, can make healthy lifestyle changes easier to accomplish, making both the drugs and the lifestyle changes more effective, and enhancing both short- and long-term success.
If you do decide to take weight loss drugs, use these strategies to get the most out of them—and preserve your long-term health.
Strategy #1: Find ways to eat nutritiously despite side effects.
The slowed stomach emptying caused by GLP-1 drugs can trigger nausea and constipation.
Fortunately, for most people, these GI woes tend to resolve within several weeks.
However, if you’re experiencing a lot of nausea, you’re not likely going to welcome salads into your life with open arms. (Think of how you feel when you have the stomach flu. A bowl of roughage doesn’t seem like it’ll “go down easy.”)
So, try to find more palatable ways to consume nutritious foods. (For example, fruits and vegetables in the form of a smoothie or pureed soup might be easier.)
Dr. Nadolsky also suggests people avoid the following common offenders:
- Big portions of any kind
- Greasy, fatty foods
- Highly processed foods
- Any strong food smells that trigger your gag reflex
- Sugar alcohols (like xylitol, erythritol, maltitol, and sorbitol, often found in diet sodas, chewing gum, and low-sugar protein bars), which can trigger diarrhea in some
Strategy #2: Prioritize strength training.
When people take GLP-1 weight loss medicines, about 30 to 40 percent of the weight they lose can come from lean mass.18, 19, 20
Put another way: For every 10 pounds someone loses, about six to seven come from fat and three to four from muscle, bone, and other non-fat tissues.
However, there’s two important caveats to this statistic:
1. People with severe obesity generally have more muscle and bone mass than others. (Carrying around an extra 100+ pounds of body weight means muscles have to adapt by getting bigger and stronger.)
2. Muscle and bone loss aren’t inevitable. (As Dr. Nadolsky puts it, “Muscle loss isn’t a reason to avoid treating obesity [with medication]. It’s a reason to do more exercise.”)
To preserve muscle and bone mass, aim for at least two full-body resistance training sessions a week.
In addition, move around as much as you can. Walking and other forms of physical activity are vital for keeping metabolism healthy—and can help to move food through the gut to ease digestion.21, 22
(Need inspiration for strength training? Check out our free exercise video library.)
Strategy #3: Lean into lean protein.
In addition to strength training, adequate protein consumption is vital for helping to protect muscle mass.
You can use our free macros calculator to determine the right amount of protein for you. (Spoiler: Most people will need 1 to 2 palm-sized protein portions per meal, or about 0.5 to 1 gram of protein per pound of body weight per day.)
Strategy #4: Fill your plate with fruit and veggies.
Besides being good for your overall health, whole, fresh, and frozen produce fuels you with critical nutrients that can help drive down levels of inflammation.
In addition to raising your risk for disease, chronic inflammation can block protein synthesis, making it harder to maintain muscle mass.
(Didn’t know managing inflammation matters when it comes to preserving muscle? Find out more muscle-supporting strategies here: How to build muscle strength, size, and power)
Strategy #5: Choose high-fiber carbs over low-fiber carbs.
Beans, lentils, whole grains, and starchy tubers like potatoes and sweet potatoes do a better job of helping you feel full and managing blood sugar than lower-fiber, more highly processed options.
(Read more about the drawbacks—and occasional benefits—of processed foods here: Minimally processed vs. highly processed foods)
Strategy #6: Choose healthy fats.
Healthy fats can help you feel full between meals and protect your overall health.
Gravitate toward fats from whole foods like avocado, seeds, nuts, and olive oil, as well as fatty fish (which is a protein too!)—using them to replace less healthy fats from highly-processed foods (like chips or donuts).
(Not sure which fats are healthy? Use our 3-step guide for choosing the best foods for your body)
Strategy #7: Consider coaching.
It may go without saying, but the above suggestions are just the start.
(There’s also: quality sleep, social support, stress management, and more.)
While many people choose to tackle these strategies on their own, many others find that the support, guidance, and creative problem-solving that a good coach can provide makes the whole process a lot easier—not to mention more enjoyable and more likely to stick.
And that’s the real gift of coaching: A coach doesn’t just help you figure out what to eat and how to move; They help you remove barriers, build skills, and create systems and routines so that habits become so natural and automatic that it’s hard to imagine not doing them.
Then, if you do want to stop taking medication, your ingrained lifestyle habits (that coaching reinforced, and medication perhaps made easier to adopt) will make it more likely that you maintain your results.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Phelan, S. M., D. J. Burgess, M. W. Yeazel, W. L. Hellerstedt, J. M. Griffin, and M. van Ryn. 2015. “Impact of Weight Bias and Stigma on Quality of Care and Outcomes for Patients with Obesity.” Obesity Reviews: An Official Journal of the International Association for the Study of Obesity 16 (4): 319–26.
2. Tomiyama, A. Janet, Deborah Carr, Ellen M. Granberg, Brenda Major, Eric Robinson, Angelina R. Sutin, and Alexandra Brewis. 2018. “How and Why Weight Stigma Drives the Obesity ‘Epidemic’ and Harms Health.” BMC Medicine 16 (1).
3. Tomiyama, A. Janet. 2019. “Stress and Obesity.” Annual Review of Psychology 70 (1): 703–18.
4. Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021 Mar 18;384(11):989–1002
5. Garvey WT, Batterham RL, Bhatta M, Buscemi S, Christensen LN, Frias JP, et al. Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial. Nat Med. 2022 Oct;28(10):2083–91.
6. le Roux CW, Zhang S, Aronne LJ, Kushner RF, Chao AM, Machineni S, et al. Tirzepatide for the treatment of obesity: Rationale and design of the SURMOUNT clinical development program. Obesity. 2023 Jan;31(1):96–110.
7. Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022 Jul 21;387(3):205–16..
8. Leung, Alice W. Y., Ruth S. M. Chan, Mandy M. M. Sea, and Jean Woo. 2017. “An Overview of Factors Associated with Adherence to Lifestyle Modification Programs for Weight Management in Adults.” International Journal of Environmental Research and Public Health 14 (8).
9. Jastreboff, Ania M., Louis J. Aronne, Nadia N. Ahmad, Sean Wharton, Lisa Connery, Breno Alves, Arihiro Kiyosue, et al. 2022. “Tirzepatide Once Weekly for the Treatment of Obesity.” The New England Journal of Medicine 387 (3): 205–16.
10. Jastreboff, Ania M., Lee M. Kaplan, Juan P. Frías, Qiwei Wu, Yu Du, Sirel Gurbuz, Tamer Coskun, Axel Haupt, Zvonko Milicevic, and Mark L. Hartman. 2023. “Triple–Hormone-Receptor Agonist Retatrutide for Obesity — A Phase 2 Trial.” The New England Journal of Medicine 389 (6): 514–26.
11. Maciejewski, Matthew L., David E. Arterburn, Lynn Van Scoyoc, Valerie A. Smith, William S. Yancy Jr, Hollis J. Weidenbacher, Edward H. Livingston, and Maren K. Olsen. 2016. “Bariatric Surgery and Long-Term Durability of Weight Loss.” JAMA Surgery 151 (11): 1046–55.
12. Ryan DH, Yockey SR. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr Obes Rep. 2017 Jun;6(2):187–94.
13. Marx N, Husain M, Lehrke M, Verma S, Sattar N. GLP-1 Receptor Agonists for the Reduction of Atherosclerotic Cardiovascular Risk in Patients With Type 2 Diabetes. Circulation. 2022 Dec 13;146(24):1882–94.
14. Lincoff AM, Brown-Frandsen K, Colhoun HM, Deanfield J, Emerson SS, Esbjerg S, et al. Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes. N Engl J Med. 2023 Dec 14;389(24):2221–32.
15. Kosiborod MN, Abildstrøm SZ, Borlaug BA, Butler J, Rasmussen S, Davies M, et al. Semaglutide in Patients with Heart Failure with Preserved Ejection Fraction and Obesity. N Engl J Med. 2023 Sep 21;389(12):1069–84.
16. Karakasis P, Patoulias D, Fragakis N, Klisic A, Rizzo M. Effect of tirzepatide on albuminuria levels and renal function in patients with type 2 diabetes mellitus: A systematic review and multilevel meta-analysis. Diabetes Obes Metab [Internet]. 2023 Dec 20
17. N.d. Accessed May 21, 2024. https://newconsumer.com/wp-content/uploads/2024/03/Consumer-Trends-2024-Food-Wellness-Special.pdf
18. Ida S, Kaneko R, Imataka K, Okubo K, Shirakura Y, Azuma K, et al. Effects of Antidiabetic Drugs on Muscle Mass in Type 2 Diabetes Mellitus. Curr Diabetes Rev. 2021;17(3):293–303.
19. Wilding JPH, Batterham RL, Calanna S, Van Gaal LF, McGowan BM, Rosenstock J, et al. Impact of Semaglutide on Body Composition in Adults With Overweight or Obesity: Exploratory Analysis of the STEP 1 Study. J Endocr Soc. 2021 May 3;5(Supplement_1):A16–7.
20. Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021 Mar 18;384(11):989–1002.
21. Gorgojo-Martínez JJ, Mezquita-Raya P, Carretero-Gómez J, Castro A, Cebrián-Cuenca A, de Torres-Sánchez A, et al. Clinical Recommendations to Manage Gastrointestinal Adverse Events in Patients Treated with Glp-1 Receptor Agonists: A Multidisciplinary Expert Consensus. J Clin Med Res [Internet]. 2022 Dec 24;12(1).
22. Tantawy SA, Kamel DM, Abdelbasset WK, Elgohary HM. Effects of a proposed physical activity and diet control to manage constipation in middle-aged obese women. Diabetes Metab Syndr Obes. 2017 Dec 14;10:513–9.
The post Considering (or currently taking) weight loss drugs? Here’s what you need to know appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
We all make thousands of decisions every day, large and small.
What to have for breakfast. Whether or not to exercise—or when. Which project to tackle first at work. More coffee or not.
After a while, it’s only natural that decision fatigue sets in.
Decision fatigue can happen to anyone—but it’s especially disruptive when you’re trying to change old habits and make new (healthier) choices, but you lose steam by 10 AM.
Let’s take a closer look at what decision fatigue is, what causes it, and how to shake it off so you can continue to make good, intentional choices ongoing.
What is decision fatigue, anyway?
Decision fatigue refers to the deteriorating quality of decisions made after a prolonged period of decision-making. Decision fatigue can also happen when faced with an overwhelming number of choices.
When working toward wellness goals, the mental exhaustion from constant decision-making can hinder your ability to make positive choices, especially in areas like exercise and nutrition. The constant evaluation of your workout schedules, meal choices, and other aspects of your lifestyle and routine can lead to decision fatigue.
Signs of decision fatigue
Decision fatigue can manifest in several ways. It might last days, weeks, or longer.
Here are six common signs that you might be experiencing it.
Sign #1: Procrastination and avoiding decisions
One of the primary signs of decision fatigue is procrastination and the tendency to avoid making choices. As decision fatigue sets in, you may find it increasingly challenging to initiate or conclude decision-making processes, leading to delays and lack of action.
Sign #2: Impulsivity
On the other hand, decision fatigue can also manifest as impulsivity. In an effort to expedite decision-making and alleviate mental strain, you may resort to impulsive choices, increasing the likelihood of taking less thoughtful actions.
Sign #3: Exhaustion
Decision fatigue often leads to mental exhaustion. You may feel tired and mentally drained, which may affect your overall cognitive functioning and energy levels.
Sign #4: Brain fog
A common symptom of decision fatigue is the sensation of “brain fog.” This mental cloudiness can hinder clarity of thought, making it difficult for individuals to focus, process information, and make wise choices.
Sign #5: Overwhelm
As decision fatigue accumulates, individuals may become easily overwhelmed by even minor choices. Tasks that would typically be manageable may seem daunting, contributing to heightened stress levels.
Sign #6: Irritability
Decision fatigue can lead to increased irritability and emotional sensitivity. The mental strain from continuous decision-making may impact an individual’s patience and tolerance, resulting in reactive emotional responses.
What causes decision fatigue?
A combination of factors can contribute to decision fatigue.
Cause #1: You’re always making decisions.
When you find yourself constantly making numerous decisions throughout the day, from choosing what to wear to deciding on work-related tasks, you may be prone to decision fatigue.
The cumulative effect of these daily choices can overwhelm your cognitive resources, making subsequent decisions more challenging.
Cause #2: You make a lot of decisions that impact other people.
Decisions that have a significant impact on others can contribute to decision fatigue.
When your choices carry weight and affect those around you, the mental burden intensifies. Balancing personal and professional responsibilities that influence others can lead to a heightened sense of responsibility and decision-related stress.
Cause #3: You make stressful or complex decisions.
Engaging in decision-making that is particularly stressful or complex can accelerate the onset of decision fatigue.
Evaluating intricate scenarios, especially under pressure, demands more cognitive resources, expediting mental exhaustion. High-stake decisions amplify the toll on your mental energy, making subsequent choices more taxing.
Cause #4: You’re experiencing a difficult or uncertain life situation.
Life situations characterized by difficulty or uncertainty can exacerbate decision fatigue.
Coping with unusually stressful challenges, whether personal or professional, consumes mental bandwidth. Navigating through uncertainty heightens decision-related stress, intensifying the impact of decision fatigue.
How does decision fatigue relate to your health and wellness?
Decisions related to diet, exercise, and overall health management can be overwhelming.
Constantly evaluating food choices, workout routines, and health-related decisions can challenge cognitive resources, exacerbating decision fatigue.
Further, when experiencing decision fatigue, your ability to make thoughtful, proactive health decisions diminishes. Fatigue may lead to impulsive choices, such as impulsive eating or skipping workouts, impacting your progress toward your goals.
How to overcome decision fatigue
Overcoming decision fatigue may not happen instantly, but by following these tips, you can significantly reduce its effect on your health and well-being.
All it takes is some careful planning and learning to let go.
Strategy #1: Remove choice from areas of your life where you can.
The intentional simplification of daily decisions not only streamlines your life but also enhances your cognitive capacity for more meaningful and impactful choices.
One approach is to establish routines to set some aspects of your daily life in stone—no decisions necessary. This deliberate structuring (such as predetermining what days/times you do your workouts) serves to reduce the ongoing need for decision-making in these areas.
Implementing routines also provides a psychological framework that turns repetitive decisions into automatic actions. For instance, adopting a regular weekly meal prep ritual.
Of course, this strategy is particularly beneficial for recurring activities, where predetermined choices can be consistently applied. This act of intentionally removing choices can give you back a sense of control and predictability in your daily life.
Strategy #2: Delegate where you can.
Whether in the workplace or at home, delegating decisions to others not only lightens your cognitive (and practical) burden but also promotes collaboration.
Distributing tasks at work fosters a sense of shared responsibility—and of course lightens your workload. By involving team members in decision-making processes, you not only benefit from diverse perspectives but also empower others to contribute their expertise.
Similarly, within the family or household, delegating responsibilities not only shares the cognitive load but also promotes a more supportive environment. This practice allows each family member to contribute their unique strengths, creating a more balanced distribution of decision-making responsibilities.
Strategy #4: Prioritize relaxation activities.
Relaxation activities are particularly effective in combating the effects of decision fatigue.
Quality sleep rejuvenates cognitive functions and replenishes mental energy. When you’re well-rested, you’re better equipped to face the challenges of decision-making.
In addition to sleep, try engaging in mindfulness practices, such as meditation or deep breathing exercises.
Exercise, too, not only promotes better sleep but also releases endorphins, which elevate mood and improve cognitive function.
Strategy #5: Manage stress and practice self-care.
Stress and decision fatigue are connected, so learning to manage the former will help alleviate symptoms of the latter.
Many of the relaxation techniques we previously mentioned are also great stress management tactics.
Try establishing a consistent self-care routine, like reading, taking a warm bath, or spending quality time with loved ones. These activities can provide a mental break and contribute to a positive mindset, which, in turn, helps prevent and reduce decision fatigue.
Strategy #6: Work with a coach.
By hiring a coach, you effectively delegate certain decisions to an expert.
By leveraging their knowledge, you not only streamline decision-making but also gain valuable insights and support on your journey to optimal health.
A health coach provides guidance on fitness, nutrition, sleep, stress, and recovery, and can design tailored plans to help you improve each of these areas.
Moreover, a health coach assists in establishing routines, contributing to the removal of unnecessary decisions from your daily life.
Working with a coach offers personalized support, helping you navigate health-related decisions while also enhancing accountability and motivation.
We’re here to help you reach your goals
At Precision Nutrition, our coaches are certified experts who can help you make positive decisions to improve your life. Decision fatigue ends with us, as every client receives a personalized, tailored plan designed to work with their personal preferences, lifestyle, and goals.
Learn more about how the coaches at Precision Nutrition can help you learn to live the healthier, more well-balanced life you deserve.
The post How to navigate decision fatigue when working toward your fitness goals appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
Once you decide you want to work with a health coach, finding the right one goes beyond checking off a list of qualifications.
How do you know if you’ve found the best health coach for you? What are the qualities of a good coach besides the obvious credentials?
We’ve listed some traits to look out for when choosing a health coach.
Essentially, it all boils down to how the two of you “vibe.” You should find someone you get along with and trust, someone who seems to truly “get” you and is as invested in your success as you are.
Let’s dive deeper into what all that means.
Why is it important to find a good health coach?
A skilled health coach serves as a personalized guide.
They’ll help you achieve your goals with tailored advice, motivation, custom nutrition plans, and exercise routines designed specifically for you.
They won’t just give you generalized or generic advice about diet and exercise. This individualized approach ensures that you maximize your full potential and make the most of your fitness journey.
7 signs you’ve found a good coach
What are the qualities of a good coach?
How do you know when you’ve found one?
These seven qualities are by no means an exhaustive list, but they can help you narrow down your options.
1. They can walk you through their process.
A good health coach should possess the skill to clearly explain the steps, strategies, and milestones integral to their approach.
This not only demonstrates their expertise but also shows that they have a structured process to help you succeed.
Even more than that, they should also be able to draw on insights gained from practical experience. Articulating lessons learned from working with other clients like you shows understanding for the issues or preferences you might have. They’ve proven that they know how to address challenges similar to yours.
2. They can provide references and testimonials.
A hallmark of a good coach is their openness to share references and testimonials without hesitation. Transparency not only reflects confidence in their ability but also underscores their commitment to client satisfaction.
Ideally, these references should be from clients in your demographic with similar goals. If you have a particular injury, for example, a good coach will have testimonials from clients they’ve worked with in the past who experienced a similar injury or physical limitation. A good coach understands the value of real-world feedback and recognizes that the experiences of past clients can speak volumes.
Moreover, the ability to connect with past clients demonstrates a coach’s confidence in the relationships they’ve built. If a coach avoids providing references, that should raise concerns about their client interactions and the impact of their coaching.
Testimonials, in particular, offer insights into the tangible benefits clients have experienced under a coach’s guidance. Positive testimonials not only validate the coach’s skills but also provide you with a glimpse of the potential results you can expect.
3. They ask you questions.
A coach’s interest in your story is a reflection of their commitment to your success. They should ask you questions—lots of them. A quality coaching relationship is built on a foundation of understanding, and effective coaches recognize the importance of delving into your unique circumstances.
Rather than simply presenting a pre-packaged solution, a good coach should be genuinely interested in your “why.” They should want to understand your motivations, challenges, and specific goals. The questions they ask should help them tailor their coaching plan to your particular preferences and lifestyle.
4. They listen to you.
Another quality of a good coach is the ability to integrate your thoughts and feedback into the coaching process. Remember, this is a two-way, collaborative relationship.
Listening extends beyond the spoken word; it involves deciphering the nuances and subtleties of your communication. A good coach is attuned to not only what you say but how you say it.
A coach’s responsiveness to your feedback should foster an environment of trust. If you express concerns or suggest modifications to the plan, a good coach listens, understands, and adapts the program. This flexibility ensures that the coaching process remains dynamic, adjusting to your evolving needs and circumstances.
5. They communicate openly and often.
As we said, transparent and open communication is a two-way street. This element is fundamental to your success and includes how and when you and your coach touch base.
Effective coaches establish clear expectations regarding communication from the outset. Whether it’s setting regular check-ins, defining response times, or outlining preferred communication channels, a good coach is accessible to you and reliable in responding. You should feel comfortable reaching out, knowing that your coach is receptive to any questions or concerns you have.
6. They consider your health holistically.
Your well-being extends beyond isolated facets like exercise and nutrition. You’ll know you’ve found a good health coach when they also take into account your sleep quality, stress levels, past injuries, and exercise experience. They know how these factors work together and influence one another.
For instance, understanding your nutritional habits allows a coach to develop a diet plan that improves on your current eating habits, without being unrealistic. Acknowledging past injuries or exercise experiences informs workout routines that prioritize safety and effectiveness. The consideration of sleep patterns and stress levels further refines the approach, promoting overall well-being.
This holistic, multi-faceted view of well-being is called “Deep Health.” And when a Deep Health approach is applied, it means you’re more likely to create positive habits that affect every aspect of your life—for the long term.
7. They can adjust your program to fit your needs.
A good coach will adjust your program to fit your changing needs as you work to achieve your goals.
Whether you have specific dietary requirements, time constraints, or preferences in workout styles, a coach tailors the program to ensure it not only helps you make progress but also integrates seamlessly into your lifestyle—and can adapt as necessary.
Tips for finding a good health coach
Finding a good health coach goes beyond looking up online reviews or asking friends for recommendations (though those are good ways to get started).
Here are some more tips to keep in mind as you look for a health coach.
Identify your goals
Before seeking a coach, take a moment for introspection.
Ask yourself why you want to work with a health coach and what specific outcomes you aim to achieve.
Whether it’s weight loss, improved fitness, better sleep, or overall well-being, clarity on your objectives serves as a guiding compass in selecting the right coach.
However, it’s also okay not to have a specific goal, or if your goal is something general like, “I want to be healthier.” Helping you clarify and refine your goals is part of a health coach’s job. They can engage you in meaningful conversations to understand your aspirations, challenges, and motivations until the two of you shape a tailored plan together.
Talk to prospective health coaches
Once you’ve identified three to five potential health coaches, take time to meet with each one-on-one.
Prepare a list of questions and talking points to guide these discussions. Your questions should focus on things like their coaching philosophy, past experiences, and success stories. Understanding how their approach aligns with your goals is essential to making sure you truly “get” one another.
During these conversations, also pay attention to the coach’s communication style and demeanor. Consider whether you feel comfortable and genuinely heard during the conversation.
Day-to-day logistics are important as well. As you get to know each coach, ask them about their availability, preferred communication channels, and the structure of the coaching sessions. This will ensure a smooth and manageable collaboration.
Evaluate the “vibe”
Coaching is, at its core, a relationship-based service, and the personal connection you establish with your coach can profoundly impact your motivation and commitment to your health goals. A positive and supportive connection fosters a sense of trust, making the coaching relationship more enjoyable and effective.
However, recognize that there’s no “perfect” coach.
Instead, focus on finding a coach who’s “good enough” for you—someone whose approach aligns with your preferences and understands your unique circumstances. While there might be a coach who, on paper, seems to fit all your criteria, less tangible elements like a coach’s personality, communication style, and general energy are paramount. Trust your instincts and choose a coach with whom you genuinely connect.
We’re here to help you reach your goals
The health coaches at Precision Nutrition are experts in their fields. They take the time to understand your behavior and habits as they design a plan to fit your unique goals and lifestyle.
Our coaches don’t just give you advice about diet and exercise. They work closely with you so you can learn healthier, sustainable habits that will help you feel better long term.
Try our 1:1 coaching program now and achieve the results you deserve.
The post How to know you’ve found a good health coach appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
Once you decide you want to work with a health coach, finding the right one goes beyond checking off a list of qualifications.
How do you know if you’ve found the best health coach for you? What are the qualities of a good coach besides the obvious credentials?
We’ve listed some traits to look out for when choosing a health coach.
Essentially, it all boils down to how the two of you “vibe.” You should find someone you get along with and trust, someone who seems to truly “get” you and is as invested in your success as you are.
Let’s dive deeper into what all that means.
Why is it important to find a good health coach?
A skilled health coach serves as a personalized guide.
They’ll help you achieve your goals with tailored advice, motivation, custom nutrition plans, and exercise routines designed specifically for you.
They won’t just give you generalized or generic advice about diet and exercise. This individualized approach ensures that you maximize your full potential and make the most of your fitness journey.
7 signs you’ve found a good coach
What are the qualities of a good coach?
How do you know when you’ve found one?
These seven qualities are by no means an exhaustive list, but they can help you narrow down your options.
1. They can walk you through their process.
A good health coach should possess the skill to clearly explain the steps, strategies, and milestones integral to their approach.
This not only demonstrates their expertise but also shows that they have a structured process to help you succeed.
Even more than that, they should also be able to draw on insights gained from practical experience. Articulating lessons learned from working with other clients like you shows understanding for the issues or preferences you might have. They’ve proven that they know how to address challenges similar to yours.
2. They can provide references and testimonials.
A hallmark of a good coach is their openness to share references and testimonials without hesitation. Transparency not only reflects confidence in their ability but also underscores their commitment to client satisfaction.
Ideally, these references should be from clients in your demographic with similar goals. If you have a particular injury, for example, a good coach will have testimonials from clients they’ve worked with in the past who experienced a similar injury or physical limitation. A good coach understands the value of real-world feedback and recognizes that the experiences of past clients can speak volumes.
Moreover, the ability to connect with past clients demonstrates a coach’s confidence in the relationships they’ve built. If a coach avoids providing references, that should raise concerns about their client interactions and the impact of their coaching.
Testimonials, in particular, offer insights into the tangible benefits clients have experienced under a coach’s guidance. Positive testimonials not only validate the coach’s skills but also provide you with a glimpse of the potential results you can expect.
3. They ask you questions.
A coach’s interest in your story is a reflection of their commitment to your success. They should ask you questions—lots of them. A quality coaching relationship is built on a foundation of understanding, and effective coaches recognize the importance of delving into your unique circumstances.
Rather than simply presenting a pre-packaged solution, a good coach should be genuinely interested in your “why.” They should want to understand your motivations, challenges, and specific goals. The questions they ask should help them tailor their coaching plan to your particular preferences and lifestyle.
4. They listen to you.
Another quality of a good coach is the ability to integrate your thoughts and feedback into the coaching process. Remember, this is a two-way, collaborative relationship.
Listening extends beyond the spoken word; it involves deciphering the nuances and subtleties of your communication. A good coach is attuned to not only what you say but how you say it.
A coach’s responsiveness to your feedback should foster an environment of trust. If you express concerns or suggest modifications to the plan, a good coach listens, understands, and adapts the program. This flexibility ensures that the coaching process remains dynamic, adjusting to your evolving needs and circumstances.
5. They communicate openly and often.
As we said, transparent and open communication is a two-way street. This element is fundamental to your success and includes how and when you and your coach touch base.
Effective coaches establish clear expectations regarding communication from the outset. Whether it’s setting regular check-ins, defining response times, or outlining preferred communication channels, a good coach is accessible to you and reliable in responding. You should feel comfortable reaching out, knowing that your coach is receptive to any questions or concerns you have.
6. They consider your health holistically.
Your well-being extends beyond isolated facets like exercise and nutrition. You’ll know you’ve found a good health coach when they also take into account your sleep quality, stress levels, past injuries, and exercise experience. They know how these factors work together and influence one another.
For instance, understanding your nutritional habits allows a coach to develop a diet plan that improves on your current eating habits, without being unrealistic. Acknowledging past injuries or exercise experiences informs workout routines that prioritize safety and effectiveness. The consideration of sleep patterns and stress levels further refines the approach, promoting overall well-being.
This holistic, multi-faceted view of well-being is called “Deep Health.” And when a Deep Health approach is applied, it means you’re more likely to create positive habits that affect every aspect of your life—for the long term.
7. They can adjust your program to fit your needs.
A good coach will adjust your program to fit your changing needs as you work to achieve your goals.
Whether you have specific dietary requirements, time constraints, or preferences in workout styles, a coach tailors the program to ensure it not only helps you make progress but also integrates seamlessly into your lifestyle—and can adapt as necessary.
Tips for finding a good health coach
Finding a good health coach goes beyond looking up online reviews or asking friends for recommendations (though those are good ways to get started).
Here are some more tips to keep in mind as you look for a health coach.
Identify your goals
Before seeking a coach, take a moment for introspection.
Ask yourself why you want to work with a health coach and what specific outcomes you aim to achieve.
Whether it’s weight loss, improved fitness, better sleep, or overall well-being, clarity on your objectives serves as a guiding compass in selecting the right coach.
However, it’s also okay not to have a specific goal, or if your goal is something general like, “I want to be healthier.” Helping you clarify and refine your goals is part of a health coach’s job. They can engage you in meaningful conversations to understand your aspirations, challenges, and motivations until the two of you shape a tailored plan together.
Talk to prospective health coaches
Once you’ve identified three to five potential health coaches, take time to meet with each one-on-one.
Prepare a list of questions and talking points to guide these discussions. Your questions should focus on things like their coaching philosophy, past experiences, and success stories. Understanding how their approach aligns with your goals is essential to making sure you truly “get” one another.
During these conversations, also pay attention to the coach’s communication style and demeanor. Consider whether you feel comfortable and genuinely heard during the conversation.
Day-to-day logistics are important as well. As you get to know each coach, ask them about their availability, preferred communication channels, and the structure of the coaching sessions. This will ensure a smooth and manageable collaboration.
Evaluate the “vibe”
Coaching is, at its core, a relationship-based service, and the personal connection you establish with your coach can profoundly impact your motivation and commitment to your health goals. A positive and supportive connection fosters a sense of trust, making the coaching relationship more enjoyable and effective.
However, recognize that there’s no “perfect” coach.
Instead, focus on finding a coach who’s “good enough” for you—someone whose approach aligns with your preferences and understands your unique circumstances. While there might be a coach who, on paper, seems to fit all your criteria, less tangible elements like a coach’s personality, communication style, and general energy are paramount. Trust your instincts and choose a coach with whom you genuinely connect.
We’re here to help you reach your goals
The health coaches at Precision Nutrition are experts in their fields. They take the time to understand your behavior and habits as they design a plan to fit your unique goals and lifestyle.
Our coaches don’t just give you advice about diet and exercise. They work closely with you so you can learn healthier, sustainable habits that will help you feel better long term.
Try our 1:1 coaching program now and achieve the results you deserve.
The post Private: How to know you’ve found a good health coach appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
A personalized fitness and nutrition program is the antidote to one-size-fits-all, generic advice.
If you’re tired of trying programs that just don’t fit with your lifestyle or preferences, a personalized program may be what you need to get—and stay—on track.
We’ll explore what a personalized coaching program includes, as well as the many health and wellness benefits you can enjoy when you follow one.
What does it mean to have a personalized coaching program?
In a personalized coaching program, you work with a health coach who tailors a plan to fit your unique needs.
They assess your individual goals, lifestyle, and preferences to create a program that’s designed just for you.
Personalized coaching programs often include custom nutrition and exercise plans, but they also take into account factors like your current skills, history, schedule, relationships, and stressors.
What are the benefits of individualized coaching?
Let’s take a look at what you can expect from a personalized coaching program and all the ways it can help you feel better in the long term.
Specifically targets your goals
By personalizing your plan, a dedicated health coach helps you work toward specific goals while paying careful attention to your overall well-being.
Whether your aim is weight management, stress reduction, or improved sleep, a personalized program ensures that each aspect of your routine contributes to these goals. Your coach tailors not only workouts and dietary guidelines but also considers broader lifestyle factors to holistically support your health objectives.
For instance, if weight management is your primary goal, your coach doesn’t just prescribe a generic workout routine but tailors exercises that are both effective and enjoyable for you. Simultaneously, dietary recommendations are carefully customized, taking into account your preferences and expectations.
A health coach considers all elements of your daily life—your schedule, stress tolerance, health conditions—when developing your personalized program. When a health coach takes this approach, it can help shape your daily routine so it’s aligned with your goals.
Provides personal support and attention
With personalized coaching, you’re not navigating your health journey alone. Your coach is there to provide ongoing support, helping you overcome challenges and celebrate victories.
As you work together, your coach will continue adjusting your plan to meet your needs more precisely.
Moreover, the added accountability is a major advantage of personalized nutrition coaching. Regular check-ins and feedback sessions provide an opportunity for both of you to address concerns, refine strategies, and celebrate milestones.
The individualized support and attention from a coach can increase your chances of achieving—and sustaining—your health and wellness goals.
Customized learning and teaching
In a personalized nutrition coaching program—unlike generic workout classes or mass-produced fitness programs—the teaching approach can be customized to suit your unique learning style. This customization helps you integrate information more effectively while also enjoying the process.
Perhaps in the past, you’ve experienced the frustration of feeling overwhelmed or lost in a workout class due to a mismatch in teaching styles. With a personal health coach, you have the opportunity to find someone you connect with better.
This dynamic of trust between the two of you helps you both feel confident, comfortable, and excited to work together. You can ask questions, seek clarification, and engage in meaningful discussions with your coach. They, in turn, can ask questions and clarify your needs as you progress.
Incorporates your preferences and needs
A good health coach will consider your past experiences, limitations, and current values and goals to ensure that every aspect of the program is customized to you.
Whether it’s dietary choices, favorite exercises, or scheduling constraints, your coach tailors the plan to fit organically into your life. This helps maximize the chances you’ll stick with the plan.
For instance, if you have dietary restrictions or preferences, your coach can design a personal nutrition plan that accommodates those specifications. Similarly, if you have physical limitations or aptitudes in terms of exercise, they can adapt a program to include activities that you enjoy and that align with your abilities.
Your coach will also consider your mental and emotional well-being. A good health coach will not only be trained in nutrition and fitness, but also human behavior and psychology, so they can design strategies to help you address stress, motivation, and overall recovery.
Easily adjustable
One major advantage of a personalized coaching program is the flexibility it offers, allowing you to easily adjust your plan as needed. Unlike rigid, one-size-fits-all approaches, a dedicated health coach understands that life is dynamic and what works today may need adjusting tomorrow.
This adaptability is essential for long-term success. Your coach will also help you progress at a pace that works for you so you can continue to feel challenged and motivated without pushing too hard or getting bored.
If something in your plan isn’t working as expected, your coach is there to help. Open communication with a coach you trust allows you to have candid conversations about your progress, challenges, and any necessary modifications.
For instance, if you find a particular type of exercise uncomfortable or unenjoyable, your coach can make program or movement adjustments for you. Similarly, if a dietary recommendation isn’t feasible due to budgetary constraints or simply your palate, your coach can help you explore alternative options that still support your health goals.
How to pick a health coach
Select a number of health coaches that work with people who have goals like yours, and then have one-on-one conversations with each to narrow down your options.
During these discussions, pay attention to how well they listen and understand what you’re looking for. The coach you choose should have a portfolio of happy clients in or close to your specific demographic. Their experience working with clients who have similar abilities or limitations to yours lets you know they understand your unique needs.
We’re here to help you reach your goals
The certified coaches at Precision Nutrition are experts in their field and can help you make sustainable lifestyle changes to reach your goals. You’ll not only receive customized nutrition and exercise plans, but you’ll learn the skills you need to maintain your success long-term, too.
Our coaches will delve into your personal habits so you can understand why you make the choices you do—and add positive changes to your life. Learn more about our personalized, science-based coaching program today and start your journey to a healthier, happier you.
The post The importance of personalizing your fitness and nutrition program appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
From hitting a wall with your workouts to stalled weight loss, plateaus can occur at any stage.
But all that hard work hasn’t been for nothing. Plateaus, although frustrating, can be useful.
In this article, we’ll take a closer look at what causes them, how to push through, and when to consider embracing the plateau and shifting into maintenance mode.
What is a plateau in fitness?
A plateau refers to a period of time where you feel like you’re no longer making progress. For anyone who’s been actively pursuing fitness for a while, you know the signs: maybe you’ve stopped losing weight or gaining muscle, you’re bored by your workouts, or you’re struggling to find energy and recovery properly.
Progress isn’t linear, and the gains you make initially aren’t sustainable at the same rate indefinitely. Newcomers to health and fitness often experience rapid initial results, which they might expect to last forever.
However, as you become more seasoned, progress becomes more challenging, and you’ll inevitably hit plateaus more often.
Does a plateau only refer to your workout routine?
Plateaus can happen in any aspect of your wellness journey. Remember that “wellness” incorporates more than exercise—it’s about your whole, multidimensional health. Also called “Deep Health,” this refers to the many aspects of your lifestyle that work together to contribute to your overall well-being, including:
- Social health
- Physical health
- Emotional health
- Mental health
- Environmental health
- Existential health
While we often talk about plateaus in the context of your workout or fitness routine—you can’t increase the weight you’re deadlifting, or lose another few pounds of body fat—it’s not the only place a plateau can happen.
Sometimes working out harder might not be the answer, and you’ll have to address one of the other dimensions of your Deep Health—whether that’s working on your sleep, mindset, or supportive relationships.
Is a plateau always a bad thing?
Contrary to what you may have heard, a plateau is not inherently negative. It’s a natural and expected phase that occurs for various reasons (which we’ll cover in more detail below).
A plateau is simply your body’s way of providing valuable feedback.
A plateau may actually signify that you’ve reached a level of fitness worth preserving. In fact, learning how to navigate and sustain a plateau is a valuable skill. It ensures that you don’t lose the progress you’ve worked so hard to achieve.
Just as breaking through plateaus can be essential to keep working toward your goals, mastering the art of maintaining your current state of wellness also contributes to the overall success of your health endeavors.
Ultimately, that’s many people’s long-term goal: to be able to sustain the progress they’ve made at the apex of their achievement.
Why does a plateau happen?
The more you understand why you’ve hit the plateau, the better you’ll be able to adjust your plan accordingly to move beyond it.
We’ll list seven common reasons why you might have hit a plateau, plus some initial fixes to try.
Plateau reason #1: Repetitively performing the same workout routines
A fitness plateau can happen when you stick to the same workout routine without variety. While routine helps you build habits, your body adapts to the repetitive stress, which leads to diminished returns.
 To work through this plateau: Diversify your exercises, introducing new challenges that keep your muscles engaged and responsive. For example, if you’ve primarily taken cycling classes, it might be time to include some weightlifting.
To work through this plateau: Diversify your exercises, introducing new challenges that keep your muscles engaged and responsive. For example, if you’ve primarily taken cycling classes, it might be time to include some weightlifting.
Plateau reason #2: Performing ineffective training routines
Not all exercises yield the same results for everyone. If your current routine doesn’t target specific muscle groups effectively, you might hit a workout plateau.
 To work through this plateau: Focus on exercises that align with your goals and provide adequate challenges. Once you’ve determined your goals, research and select workouts that specifically target the necessary muscle groups.
To work through this plateau: Focus on exercises that align with your goals and provide adequate challenges. Once you’ve determined your goals, research and select workouts that specifically target the necessary muscle groups.
Plateau reason #3: Not pushing yourself hard enough (Intensity not high enough)
In fitness, intensity matters. If you’re not pushing yourself hard enough during workouts, your body won’t experience the necessary stress to prompt muscle growth.
 To work through this plateau: Gradually increase the intensity of your exercises and challenge your limits without compromising safety. This could mean increasing the weight you’re lifting or the tempo at which you’re completing your exercises. Take note of the number of reps you perform and/or the pace you move through your workouts so you can measure progress over time.
To work through this plateau: Gradually increase the intensity of your exercises and challenge your limits without compromising safety. This could mean increasing the weight you’re lifting or the tempo at which you’re completing your exercises. Take note of the number of reps you perform and/or the pace you move through your workouts so you can measure progress over time.
Plateau reason #4: Not progressively overloading your muscles
Muscles adapt to stress over time. If you’re not progressively increasing resistance or intensity, your muscles won’t get stronger. Plateaus can occur when your workout fails to challenge your muscles beyond their current capacity.
 To work through this plateau: Regularly increase the resistance or intensity to stimulate ongoing improvements.
To work through this plateau: Regularly increase the resistance or intensity to stimulate ongoing improvements.
Plateau reason #5: Training inconsistently
Keeping a consistent workout schedule is one of the keys to fitness. Irregular workout patterns can lead to plateaus as your body doesn’t receive a consistent stimulus for growth.
 To work through this plateau: Establish a regular workout schedule and stick to it to maintain steady progress.
To work through this plateau: Establish a regular workout schedule and stick to it to maintain steady progress.
Plateau reason #6: Needing to adjust your nutrition plan
Your eating habits can also cause plateaus. If you’re experiencing persistent fatigue or energy crashes, your nutritional intake may be falling short of your body’s needs.
Your body needs certain nutrients and enough calories for peak functionality, and if it doesn’t receive those, you might not be able to perform your workouts as well.
 To work through this plateau: Try to incorporate a higher proportion of nutrient dense, minimally processed foods into your diet so you get the macronutrients and micronutrients you need to achieve your goals.
To work through this plateau: Try to incorporate a higher proportion of nutrient dense, minimally processed foods into your diet so you get the macronutrients and micronutrients you need to achieve your goals.
Plateau reason #7: Not paying attention to other lifestyle factors
Fitness is more than just exercise. Ignoring lifestyle factors such as nutrition, sleep, and stress can contribute to plateaus. Your body needs proper fuel, recovery, and stress management to thrive.
 To work through this plateau: Try to focus on incorporating high-nutrition foods into your diet, creating an atmosphere of calm before bed, or learning healthy techniques for coping with stress.
To work through this plateau: Try to focus on incorporating high-nutrition foods into your diet, creating an atmosphere of calm before bed, or learning healthy techniques for coping with stress.
How do you know if you’ve hit a plateau?
Here are some things to look out for.
Plateau sign #1: Your workouts feel easy
When your workouts start feeling noticeably easier than they used to, it’s a strong indicator that you might be experiencing a fitness plateau. The initial challenge that once accompanied your exercises diminishes, suggesting that your body has adapted to the current routine. Pay attention to changes in perceived effort during your workouts.
Plateau sign #2: You’re not noticing progress
Lack of progress is a clear sign of a fitness plateau. If you’re not seeing improvements in strength, endurance, or other fitness parameters over an extended period, it’s time to reassess your approach. Tracking your performance and noting any stagnation can help identify when you’ve hit a plateau.
Plateau sign #3: Hitting a standstill with a particular exercise
Whether it’s running at a consistent speed, lifting heavier weights, or performing more repetitions, a plateau becomes evident when you can’t seem to push past a certain point. If you consistently struggle to make progress in a particular aspect of your fitness routine, it may be time for an adjustment.
Plateau sign #4: You’re feeling fatigued
If you’re experiencing persistent levels of tiredness, or you feel like your energy skyrockets then drops, your wellness routine—including your workout and your nutrition plan—may not be providing your body with the support and fuel it needs.
Excessive fatigue or brain fog may point to nutrient imbalances or insufficient caloric intake. On the other hand, it might indicate that you’re training too hard and not allowing your body the rest it needs. Either way, this could lead to a plateau since your body doesn’t have the resources it needs to recover and continue making progress.
How to break through a plateau
While you don’t always need to break through a plateau, it’s often worth trying.
These seven methods can help you push through if that’s what your body needs.
Or, if they don’t work, they can let you know that it’s time to shift into maintenance mode.
Plateau breakthrough #1: Upend your routine
To overcome a workout plateau, consider a radical shift in your routine.
If cardio has been your mainstay, integrate strength training to challenge your muscles in new ways.
Conversely, if you’ve been predominantly lifting weights, experiment with machines, resistance bands, or high intensity interval training to introduce variety.
Altering the type and intensity of your workouts not only targets different muscle groups but also prevents your body from acclimating to a specific routine.
Plateau breakthrough #2: Focus on nutrition
Breaking through a plateau isn’t only about changing your exercise routine—it’s about addressing all aspects of health.
Assess your nutrition to ensure it supports your fitness goals, providing the energy and nutrients your body requires.
Experiment with meal timing and frequency to optimize energy levels throughout the day, preventing slumps and cravings.
Hydration also plays an important role in performance, so make sure you’re drinking enough water daily.
Plateau breakthrough #3: Try something completely new
Introduce novelty to shake things up.
If solo workouts have been your norm, join a group fitness class for a change of pace. If the gym is your usual setting, consider engaging in a local sports league or trying a new outdoor activity over the weekend.
The unfamiliarity of a new challenge not only sparks physical adaptation but might also rekindle your motivation.
Beyond exercise, shake up your nutrition. Experiment with different foods. Try new recipes. Explore a different dietary approach. These can all provide the nutritional variety your body needs for renewed progress.
Plateau breakthrough #4: Focus on progressive overload
If your focus is on strength training, a plateau may arise when you neglect to consistently challenge your muscles. Avoid this plateau (or push through it) by gradually increasing the resistance or intensity of your exercises.
Carefully track your current lifting capacity and strategically plan increased increments of resistance.
Aim for gradual but steady progression, whether it’s adding more weight, increasing repetitions, or adjusting the intensity of your workout.
Plateau breakthrough #5: Rest, recover, repeat
Overtraining or consistently pushing your body without adequate recovery can lead to plateaus. To break through, incorporate planned periods of rest into your routine.
During rest, the body repairs and strengthens itself, allowing muscles to recover and adapt to the stress of previous workouts. This process helps you avoid burnout, reduce the risk of injury, and ultimately overcome plateaus.
Consider incorporating active recovery days, where you engage in low-intensity activities to promote circulation and flexibility without imposing excessive stress on your body.
Always listen to your body’s signals. Rest and recovery are not signs of weakness but essential components of a well-rounded fitness routine—and life.
Plateau breakthrough #6: Practice healthy sleep hygiene
While a full eight hours a night of uninterrupted sleep may not be realistic for everyone, you can take proactive measures to help yourself get a good amount of rest.
Turn off devices well before bedtime, make your room quiet, cool, and comfortable, and try to stick to a consistent sleep-wake schedule.
Helping yourself learn healthy sleep habits can help you feel better, manage your weight, reduce stress, and improve your mood—among many other benefits.
Plateau breakthrough #7: Work with a health coach
When facing a plateau, enlisting the support of a health coach can be a game-changer.
A health coach brings expertise in nutrition, exercise, anatomy, physiology, sleep, stress, and recovery to help you uncover the reasons behind your plateau and navigate potential solutions tailored to your unique situation.
A health coach specializing in exercise and movement can design a progressive and personalized workout plan, ensuring that you’re incorporating variety and addressing potential weaknesses. They can also analyze your diet to ensure it aligns with your fitness goals. They may also help you improve other lifestyle factors such as sleep, stress management, and overall well-being.
Additionally, a health coach can help you determine whether this plateau is an opportunity for a breakthrough—or a sign that it’s time to focus on maintenance.
We’re here to help you reach your goals
The coaches at Precision Nutrition can help you make sustainable lifestyle changes to reach your goals. With one of our health coaches by your side, you’ll never be left alone to figure it all out. We provide expert nutritional and wellness advice that’s customized to your goals and lifestyle.
Learn more about our 1:1 Coaching Program and find out how we can help you transform your life for the better in a sustainable, healthy way.
The post Why you might have hit a plateau with your fitness goals appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
You can learn everything on your own… right?
In other words, between books and free online articles and videos, what’s the point of working with a health coach?
Well, there’s a few points…
A health coach offers unique knowledge and insights that can help you in ways you can’t necessarily get on your own. They fill in the nutritional and exercise gaps you may overlook, make sure you’re adhering to your intentions, and suggest solutions (and moral support) when you hit inevitable obstacles.
In fact, hiring a health coach may be one of the best decisions you can make for your long term wellbeing.
Keep reading to find out 11 (good) reasons to work with a health coach.
First, what is a health coach?
A health coach is a dedicated wellness expert who can help you achieve your goals.
Health coaches possess expertise based on a solid foundation in exercise science, anatomy, and physiology to craft safe and effective programs. They take into account individual requirements, capabilities, and objectives to tailor wellness plans to suit your unique needs.
Health coaches may also have nutrition expertise. They’ll delve into the dietary considerations and lifestyle factors (like stress management, sleep, and recovery) that impact your overall health.
As you attempt to make and sustain changes, your health coach can also be a valuable source of encouragement and accountability. They provide guidance, monitor progress, make adjustments as needed—so you can get the results you’ve been looking for.
11 reasons to work with a health coach
Working with a health coach can help you in numerous ways, whether you’re just starting, or need some tips or tweaks along the way.
Reason #1: You’re not seeing results.
If you’ve been putting in consistent effort without seeing results, consider the expertise of a health coach.
They bring a fresh set of eyes to your habits and routines. They’ll assess what you’re currently doing and suggest tweaks or changes to make your plan more efficient and effective.
Sometimes, it’s simply a matter of fine-tuning your approach. They’ll also help you set realistic, achievable goals, ensuring you’re on the right track.
Reason #2: You don’t know where to start.
With so much information out there, how do you know where to start? A health coach can help you make sense of all the (sometimes contradictory) advice and provide you with a clear, actionable plan.
They streamline the process, break it down into manageable steps, and offer an appropriate starting point tailored to you.
They’ll introduce you to fundamental exercises, including cardio, weight training, and flexibility training. If appropriate, they might introduce you to nutrition fundamentals, including finding the right balance of macronutrients.
A health coach takes the time to understand your specific needs, capabilities, and objectives. They’ll also ensure you’re not just going through the motions but truly understand why you’re doing what you’re doing. This helps you build a solid foundation to make gradual but definite progress.
Reason #3: You have a specific goal in mind.
If you’re focused on an objective, such as weight loss, muscle building, healthier eating, or stress management, a health coach can make a difference, helping you connect the dots between what you eat, how you move, your sleep quality, and more.
Even if you have a particular area of your life you’re striving to improve, a health coach can help you see the “big picture” view, and how often one aspect of your life is connected to and affects other aspects of your life.
That way, you can understand where to focus your energy—sleep, exercise, nutrition, relationships—to help you achieve your goal.
Reason #4: You need more structure in your wellness routine.
A health coach will create a plan that optimizes both effectiveness and efficiency.
During workouts, health coaches offer direction to ensure you exercise with precision. They provide feedback, corrections, and technique guidance to make your routine more impactful.
This also applies to nutrition. A health coach can help you learn how to incorporate foods with greater nutrient value in ways that work for you, so you’re more likely to develop healthier habits in the long-term.
Reason #5: You need someone to hold you accountable.
By scheduling regular sessions and check-ins, health coaches create a structured framework for your progress.
This significantly increases the likelihood of you adhering to your workout and nutrition intentions. Without the accountability of a scheduled session, it’s easier to skip exercise or make less nutritious food choices.
Of course, there’s always a financial and temporal investment associated with health coaching. Committing to regular sessions not only safeguards your financial investment but also reaffirms the importance of allocating time for your well-being.
Reason #6: You’re having trouble staying motivated.
In addition to accountability, your health coach serves as a source of encouragement and motivation.
They celebrate your triumphs, provide reassurance during challenging moments, and offer constructive feedback. They understand the ebb and flow of progress and help you generate the motivation needed to sustain behavior changes.
A health coach will take the time to understand your aspirations, struggles, and targets so you feel heard and valued. Having a coach to cheer you on and push you past your limits can make all the difference.
Reason #7: You need an expert resource.
Working with a health coach goes beyond achieving exercise and nutrition goals—it can be a valuable learning experience.
Certified health coaches possess a deep understanding of human physiology, body mechanics, behavior change, and nutrition science, making them a valuable resource for clients seeking comprehensive knowledge on holistic wellness.
Reason #8: You need someone to make decisions for you.
Working with a health coach offers a reprieve from the constant decision-making that comes with managing your fitness and nutrition.
The multitude of choices, from exercise routines to dietary plans, can often lead to “decision fatigue,” which can then lead to frustration. You may find it a relief to have a trusted expert guide you and help narrow your options.
Reason #9: You want to enjoy taking care of yourself.
Exercise doesn’t have to feel like a chore.
A health coach can help you find ways to move your body that are enjoyable so that you look forward to taking care of yourself.
Not all exercise suits all people, but a health coach can help you find something that works—even if you’ve never exercised before.
Reason #10: You want to learn how to take care of yourself.
If your goal is to eventually create and follow your own instincts, working with a health coach can help get you there.
As we’ve said, health coaches understand exercise, nutrition and how those two things work together to create a healthier lifestyle. By dedicating yourself to learning the wellness skills and knowledge that work for you, you’ll one day be able to sustainably take care of yourself.
Reason #11: You’re looking for long-term benefits.
Anyone can start exercising or following a fad diet.
However, a health coach will help you learn how to incorporate nutrition and movement into your life in a way that’s sustainable.
This means taking into account factors such as your age, current fitness level, goals, lifestyle, and anything else that affects your health. Long-term benefits include learning how to tend to all six aspects of Deep Health (not just what you eat and how much you exercise). Those six aspects are:
- Relational health
- Existential health
- Mental health
- Physical health
- Emotional health
- Environmental health
When you take into account your psychological well-being, your ability to focus and think clearly, how well your home and work environment supports your health, your relationships with others, and your overall sense of purpose, you’ll be more likely to create a meaningful plan—and stick with it.
We’re here to help you reach your goals
You don’t have to tackle your health journey alone.
The coaches at Precision Nutrition are experts in exercise and nutrition—as well as behavior change—and can help you reach your goals effectively and safely.
With our 1:1 Coaching Program, you’ll work with a coach who’ll tailor a nutrition and wellness plan based on your lifestyle, goals, and preferences using scientifically proven methods. With help, you’ll learn how to incorporate healthy habits into your daily lifestyle for long-term success.
The post 11 reasons to work with a health coach appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
There are so many ways to track your nutritional intake.
It can seem overwhelming to pick an (accurate) method that works for you.
That’s why we’ve developed the hand portion method.
It simplifies nutrition tracking in a way that’s accessible to anyone—and can suport any of your health and fitness goals.
A breakdown: The Hand Portion Method
Precision Nutrition’s hand portion method offers an easy solution to tracking your macros, allowing you to manage your food intake without weighing, measuring, or counting calories.
The method is simple: Estimate portion sizes with your hands.
It’s not about meticulous measurements—rather, it’s about using your hand as a reliable gauge for portion sizes.
What makes the hand portion method particularly effective is its inherent alignment with your body’s proportions. Plus, the size of your adult hand remains constant, ensuring consistency in portioning.
Here’s an overview:
- Protein: Your palm determines the size of your protein portion.
- Vegetables: Your clenched fist determines the size of your veggie portion.
- Carbohydrates: Your cupped hand determines the size of your carb portion.
- Fat: Your thumb determines the size of your fat portion.
Once you have an idea of what each portion looks like, you can aim to meet your personalized daily recommended balance of portions.
How many hand portions to eat
Most people will meet their nutritional needs by eating:
- 1-2 palms of protein-dense foods at each meal
- 1-2 fists of vegetables at each meal
- 1-2 cupped handfuls of carbohydrates at most meals
- 1-2 thumbs of fat-dense foods at most meals
Depending on your goals and frame, you may need to adjust these general recommendations up or down.
Benefits of the hand portion method
When it comes to tracking macros, the hand portion method offers several benefits:
- Accuracy with minimal effort: Our internal research shows that hand portion tracking is 95 percent as accurate as other tracking methods—but without the effort of meticulous measurement. Check out these results to see for yourself how well hand portion tracking works.
- Can be customized to your dietary preferences: Whether you follow a Mediterranean, Paleo, vegetarian, ketogenic, or fully plant-based diet, you can apply this method.
- Easy to manage macronutrient splits: With the hand portion method, you have the power to fine-tune your macronutrient split. Adjust the proportions of protein, carbohydrates, and fats to align precisely with your individual needs and objectives.
- Helpful tool for estimating calorie intake: Each hand portion is equivalent to an approximate amount of protein, carbohydrates, fat—and therefore calories. For example: 1 palm protein ~ 130-145 kcal; 1 fist of veggies ~ 25 kcal; 1 cupped hand of carbs ~ 110-120 kcal; and 1 thumb fats ~ 90-100 kcal.
Assumed variety of food choices
Our hand portion system assumes a mix of high-fat, moderate-fat, and low-fat protein sources; a mix of fruit, starchy tubers, beans, and whole grains for carbs; and a mix of fat-rich whole foods (such as nuts, cheese, or avocado), blended foods (such as pesto or nut butters), and pressed oils for fats.
And, the hand portion method can be adjusted to fit individual dietary preferences.
For example, if you’re following a ketogenic diet, you can simply increase your fat intake to make up for the decrease in carbohydrates.
Examples of the hand portion method: Approximate portion sizes for each macronutrient
Here are some examples of how much you’d eat using our hand portion method.
However, these are just approximations. The actual portion sizes will depend on the size of your individual hand and your body’s needs.
For men
A palm-sized portion of protein equals about 4 ounces of cooked meat/tofu, 1 cup of Greek yogurt or cottage cheese, 1 scoop of protein powder, or 2 whole eggs.
A fist-sized portion of vegetables is equivalent to about 1 cup of non-starchy vegetables such as spinach, carrots, cauliflower, or peppers.
A cupped hand of carbs is about ⅔ cup of cooked grains or legumes, 1 medium-sized fruit, or 1 medium tuber.
A thumb-sized portion of fat is around 1 tablespoon of oils, nuts, seeds, nut butter, avocados/guacamole, cheese, and dark chocolate.
For women
A palm-sized portion of protein equals about 3 ounces of cooked meat/tofu, 1 cup of Greek yogurt or cottage cheese, 1 scoop of protein powder, or 2 whole eggs.
A fist-sized portion of vegetables is equivalent to about 1 cup of non-starchy vegetables such as spinach, carrots, cauliflower, or peppers.
A cupped hand of carbs is about ½ cup of cooked grains or legumes, 1 medium-sized fruit, or 1 medium tuber.
A thumb-sized portion of fat is around 1 tablespoon of oils, nuts, seeds, nut butter, avocados/guacamole, cheese, and dark chocolate.
Approximate math for macronutrient portions
For number-oriented users, based on the examples above, these are the approximate macros each of the portions provide.
Macros for men’s approximate portions:
- 1 palm of protein ~ 24 g protein, 2 g carbs, 4.5 g fat, 145 kcal
- 1 fist of veggies ~ 1.5 g protein, 5 g carbs, 0 g fat, 25 kcal
- 1 cupped hand of carbs ~ 3 g protein, 25 g carbs, 1 g fat, 120 kcal
- 1 thumb of fats ~ 2 g protein, 2 g carbs, 9 g fat, 100 kcal
Macros for women’s approximate portions:
- 1 palm of protein ~ 22 g protein, 2 g carbs, 4 g fat, 130 kcal
- 1 fist of veggies ~ 1.5 g protein, 5 g carbs, 0 g fat, 25 kcal
- 1 cupped hand of carbs ~ 3 g protein, 22 g carbs, 1 g fat, 110 kcal
- 1 thumb of fats ~ 2 g protein, 2 g carbs, 8 g fat, 90 kcal
Please remember that these are approximations.
All aspects of calorie and macronutrient calculations are based on averages with known error rates.
Testing the accuracy of hand portion math
In the examples below, we’ll demonstrate that using the hand portion method is 95 to 100 percent as accurate as carefully weighing, measuring, and logging everything you eat.
Example 1
Our first example individual is a female athlete who weighs 135 pounds and has 18 percent body fat. She maintains a high activity-level, engaging in two training sessions per day. This is what she consumes in a day:
- Pre-workout @ 6 am: 16 oz of black coffee, 1 cup of plain low-fat Greek yogurt, 1 cup of chopped pineapple, 2 tbsp of chopped walnuts, 1 glass of water.
- Workout @ 7:15-8:30 am: Sips on 16 oz of water during the training session.
- Post-workout shake @ 9 am: 12 oz of water, 2 scoops of protein powder, 1 medium apple, 1/2 cup of old-fashioned oats, 2 cups of spinach, 1 tbsp of ground flax seed, 1 tbsp of almond butter.
- Lunch @ 12 pm: 3 oz of salmon, 1 cup of steamed mixed veggies, 1 medium sweet potato, 1 tbsp of coconut oil, 2 glasses of water.
- Mid-afternoon snack @ 4 pm: 1 banana, 2 tbsp of natural peanut butter, 1 glass of water.
- Workout @ 5:30-6 pm: Sips on 16 oz of water during the training session.
- Post-workout dinner @ 7 pm: 3 oz of chopped chicken breast, 2 cups of cooked whole grain pasta, plus 2 cups of sautéed veggies with 2 tbsp of extra virgin olive oil, minced garlic and white cooking wine, 2 glasses of water.
If you compute the calories and macronutrients of this person’s intake using the USDA nutrient database, you get:
- 2672 kcal
- 170 g protein
- 264 g carbs
- 104 g fat
And if you translate this person’s intake into hand-size portion terms, you get:
- Protein = 5 palms (Greek yogurt, protein powder x 2, salmon, chicken)
- Veggies = 5 fists (spinach x 2, mixed veggies, sautéed veggies x 2)
- Carbs = 10 cupped hands (pineapple x 2, apple, oats, sweet potato, banana, pasta x 4)
- Fats = 9 thumbs (walnuts x 2, flax seed, almond butter, coconut oil, peanut butter x 2, olive oil x 2)
By multiplying those portion numbers using approximate hand-portion math for women (refer to the section above), the estimated intake is:
- 2672 kcal (precisely the same as calculating it with apps and spreadsheets)
- 166 g protein (4 g less than calculating it with apps and spreadsheets)
- 273 g carbs (9 g more than calculating it with apps and spreadsheets)
- 102 g fat (2 g less than calculating it with apps and spreadsheets)
As you can see, the difference between manually tracking and using our hand portion method is a matter of only a few small grams.
Example 2
Our second example individual is a moderately active male who weighs 210 pounds and has 17 percent body fat. This is what he consumes in a day:
- Wake @ 5:30 am: 12 oz of black coffee
- Breakfast @ 7 am: 4 whole eggs with a large bunch of peppers, scallions, and mushrooms cooked in a large pat of butter, placed on a whole wheat wrap, with ~1 oz cheese, 1 cupped hand of black beans, and some pico de gallo, large glass of water, 12 oz black coffee.
- Super Shake @ 10:30 am: ~10 oz of water, 2 scoops of chocolate protein powder, 2 cups of spinach, 2 cups of frozen cherries, ~1 tablespoon cacao nibs, ~1 tablespoon of chia seeds.
- Lunch @ 2 pm: 4 oz of turkey breast, ~⅔ cup of quinoa, 1 fist of mixed veggies, 1 apple, 2 thumbs of roasted almonds, 1-2 large glasses of water.
- 1-2 cups of green tea @ 3-4 pm.
- Dinner @ 6 pm: 8 oz of sirloin (lean), 2 cupped hands of roasted red potatoes with onions, 2 cups of roasted rainbow carrots, 2 tbsp of olive oil for roasting, 1 glass of wine, 1-2 large glasses of water.
If you calculate the calories and macronutrients of this person’s intake using the USDA nutrient database, you get:
- 3130 kcal
- 212 g protein
- 283 g carbs
- 111 g fat
And if you put this person’s intake into hand portion terms, you get:
- Protein = 7 palms (eggs x 2, protein powder x 2, turkey, sirloin x 2)
- Veggies = 6 fists (scallions/peppers/mushrooms/pico, spinach x 2, mixed veggies, rainbow carrots x 2)
- Carbs = 9 cupped hands (wrap, beans, cherries x 3, quinoa, apple, potato x 2)
- Fats = 8 thumbs (butter, guacamole, cacao nibs, chia seeds, almonds x 2, olive oil x 2)
- Alcohol = 1 (wine)
When you multiply those portion numbers using approximate hand-portion math for men, the estimated intake is:
- 3183 kcal (53 kcal more than calculating it with apps and spreadsheets)
- 220g protein (8 g more than calculating it with apps and spreadsheets)
- 285g carbs (2 g more than calculating it with apps and spreadsheets)
- 113g fat (2 g more than calculating it with apps and spreadsheets)
Once again, the hand portion method is nearly as accurate as manually weighing and tracking portions—and much simpler.
We can help you meet your goals
Our Ultimate Macro Calculator can help you figure out the ideal macronutrient ratio for your specific nutrition and fitness goals. From there, our hand portion method can guide you along the road to success.
The post How to do hand portion math to track your macros appeared first on Precision Nutrition.
Source: Health1
None of us is getting any younger.
Take it from someone who’s old:
You don’t want to reach the Age of Senior Discounts with regrets about all the things you didn’t do to prepare your body and mind.
Fortunately, there’s a lot you can do, at any age.
In the following article, we’ll cover the best practices for aging well—preserving longevity, quality of life, and healthspan. They include:
- The very short list of things you should avoid.
- The much more detailed list of what you can do to get the most out of the time you have.
- The most impactful way to combine a healthy life with a happy life.
Some are easy. Some take more effort. Many are common sense. All are supported by research, some of it going back decades.
But before we get into all that, we’ll start with something more fundamental.
Why do we get old?
Despite centuries of medical breakthroughs, everyone who’s been lucky enough to get old either has died or will die.
There’s a reason no one’s been able to find a loophole.
“Virtually all of our genes, and all of our vital systems, play a role in aging,” says biochemist Charles Brenner, PhD, chair of the Department of Diabetes and Cancer Metabolism at City of Hope National Medical Center.
Because there’s no “lone gunman”—no single gene that goes gray and takes everything else down with it—there will never be a single pill, potion, or practice to stop the process, let alone reverse it.
It doesn’t matter how much money goes into the search for an “off” switch.
“The anti-aging industry has been full of grifters for thousands of years,” Brenner says. “Overpromisers and underperformers.”
The modern roots of the industry go back to 1990, when a study in the New England Journal of Medicine showed promising results from administering human growth hormone to older men.1
It was a small study—just 12 men received hGH, with nine comparable participants serving as a control group.
But the results “were sensationalized by the press in a number of exaggerated reports,” according to biologist Richard F. Walker, PhD.2
That was enough to jump-start an anti-aging “gold rush,” Walker wrote—one that was commercialized from the jump.
The money is bigger today, with tech billionaires investing crypt-loads of cash in life-extension startups.3
But the problem they keep running into remains the same, Brenner says:
In terms of lifespan, humans have already exceeded the intended “warranty.”
What he means is that humans evolved to satisfy five basic priorities:
- Avoid predation.
- Acquire food.
- Attract a mate.
- Together with your mate, turn food into babies.
- Make sure your babies live long enough to produce babies of their own.
If we had stopped there, we would be similar to all other animals. We would live as long as we’re reproductively capable, and then we’d expire.
But in the 300,000 generations since hominids split off from the great apes, we doubled our life expectancy.
That allowed some of our ancient ancestors to become active grandparents, which was a huge evolutionary advantage.4
Life expectancy doubled again in the past two centuries, thanks to breakthroughs in sanitation, nutrition, medicine, hygiene, and public safety.
And yet, despite all those gains in average lifespan, there remains a hard cap on maximum lifespan.
That’s because the aging process begins at birth and never stops.5
Once you get past your growth stage, your body becomes progressively less capable of repairing tissues and maintaining vital structures and functions.6
Two systems in particular drive the aging process.
 The first is metabolism.
The first is metabolism.
Your metabolic rate declines about 0.7 percent per year in your sixties and beyond. If you live to 95, your daily energy expenditure will be about 20 percent lower than it was in your late 50s.
That’s according to research from an international consortium of scientists who crunched four decades’ worth of metabolic data on thousands of participants of all ages.7
The problem isn’t just that elderly people lose muscle. Their remaining lean mass also burns fewer calories. That includes energy-hungry organs like the brain and liver. A slower metabolism means you’re more likely to store fat in your muscles, liver, heart, and other places it doesn’t belong.
Intramuscular fat, for example, is linked to lower strength and mobility, as well as elevated blood sugar and higher insulin resistance.8
 The second is cognition.
The second is cognition.
With advancing age comes a long list of declining cognitive abilities:9
- You’ll remember things less accurately, and take longer to pull up the memories you retain.
- You’ll struggle to learn new words, and to recognize and retrieve words you already know.
- New skills will be harder to master. It will also be harder to use your current skills in complex sequences.
The combination of physical and cognitive decline means you’re less able to do what you know how to do, and less capable of adapting to your changing circumstances.
But while the process itself is inexorable, there’s a lot you can do to slow it down.
How to age well: 4 evidence-based strategies
If you asked an expert to make a list of healthy aging strategies, it would probably have two parts. You’d expect the “do this” section to be more substantial, as it is here.
But it’s on the other side of the list that you’ll find your first line of defense against physical and mental decline.
“What you don’t do is at least as important as what you do.”
That’s according to Brian St. Pierre, MS, RD, Director of Performance Nutrition for PN.
You can probably guess most of the potential life-shortening behaviors:
- Overeating
- Smoking
- Drinking to excess
- Using non-prescription drugs to excess
- Excessive unprotected sun exposure
- Inactivity
All those things—along with infectious diseases and environmental pollutants—are what Brenner calls metabolic insults.
They all stress your metabolism and make it more difficult for your body to repair itself. (That’s the focus of Brenner’s research at City of Hope.)
On the proactive side of the list, you’ll probably find aspirational targets like:
- Get a minimum of 150 minutes a week of moderate-intensity cardio, and do some form of resistance exercise twice a week.
- Get seven to eight hours of sleep a night.
- Maintain a “healthy” body weight, defined as a body-mass index (BMI) between 18.5 and 24.9.
The problem is, very few of us have the energy or ambition to check every item on the list. Just 6.3 percent of Americans collect the entire set, according to a 2016 study by the U.S. Centers for Disease Control and Prevention.10
So, from a public-health perspective, you could say the glass is 93.7 percent empty.
Or, from a personal perspective, you could pick and choose which practices and behaviors will have the most impact on your own health—and, by extension, give you the best chance for a long, satisfying life.
Make those your “big rocks,” the things you value most and will continue doing as long as possible.
Healthy aging strategy #1: Move more and preserve muscle.
In studies going back to the last century, participants who increased their levels of physical activity lowered their risk of dying of any cause by 15 to 40 percent.11
What does that mean?
Let’s look at one study:
Starting in the late 1970s, the British Regional Heart Study recruited thousands of middle-aged men. More than 3,000 were still in contact with the researchers 20 years later. By 2016, just over half of them had died, according to public records. 12
Participants who told researchers they increased their activity level were 24 percent less likely to die of any cause, compared to those who reported moving less.
Those who sustained modest activity levels were 17 percent less likely to die than the low-activity group.
Studies show even more powerful benefits when participants push themselves hard enough to increase their cardiovascular fitness.
Simply moving up from the lowest level of fitness—usually the bottom 20 percent of the study population—to a higher level significantly decreased the risk of dying of any cause in the following years.11
Moreover, the protective benefit of cardio fitness appears to be linear. That is, the higher your fitness level, the lower your risk of dying during any particular window of time.13
You don’t need to lose weight to get the benefits of fitness
If you’re among the two-thirds of Americans with a BMI of 25 or above (full disclosure: I’m with you), you can mitigate any potential weight-related disease risk through exercise and diet.
Studies show, for example, that increasing your maximum aerobic capacity (a.k.a. VO2 max), is consistently linked to lower all-cause mortality among participants classified as overweight and obese, even when they don’t lose weight in the process.11
Muscular strength and muscle mass are also correlated with a lower mortality risk.
So is resistance training—the process of trying to increase your strength and size—especially when it’s combined with cardio exercise.14,15,16
Finally, there’s walking speed. It’s one of the least known but most powerful predictors of who’ll live the longest.17,18 Which makes sense: Walking at a brisk pace requires a mix of muscular strength, cardio fitness, balance, and mobility.
You can make all of the above as simple as this:
“Move every day,” says Stuart Phillips, PhD, director of McMaster University’s Physical Activity Centre of Excellence, where he works closely with older adults who live near the campus in Hamilton, Ontario.
“Without daily movement, you go downhill fast.”
The specifics don’t matter nearly as much as the fact you’re doing something.
Another benefit of exercise: The “virtuous cycle”
“On average, people tend to eat better when they exercise more,” St. Pierre says.
That doesn’t mean we eat less.
Although exercise does seem to have an appetite-regulating effect (especially among people with low to moderate activity levels), that changes as we crank up the duration and intensity of our workouts. Hunger rises, and we eat more.19
But even then, we at least try to make better food choices, and often succeed.
St. Pierre says we do that for both physiological and psychological reasons.
“Physiologically, exercise improves your brain health, including the parts of the brain that are highly involved in our thoughts, actions, and emotions,” he says.
Those improvements seem to reduce our desire for highly processed foods, and help us make healthier choices to replace them.
Psychologically, he says, our fitness pursuits tend to lead to a healthier meal pattern because we don’t want all that effort to go to waste. “And good habits tend to stack on one another in a virtuous cycle, as opposed to a vicious one.”
Healthy aging strategy #2: Upgrade your meal pattern.
A healthy diet, one based on minimally processed whole foods, also helps prevent many of the chronic diseases associated with aging, St. Pierre says.
Those foods include:
- A wide variety of fruits and vegetables
- Lean protein from both plant and animal sources
- High-quality carbs (whole grains, beans and legumes, and tubers)
- Fibrous fats (nuts, seeds, avocadoes) and extra-virgin olive oil and other cold-pressed oils
“The biggest thing to emphasize is the overall pattern,” he adds. “Whether you eat more carbs or more fats is a personal preference.”
Getting a variety of foods within each category is helpful. That’s especially true for fruits and vegetables. You’ll not only get an abundance of key vitamins and minerals, the water they contain will also help keep your body hydrated.
That’s important because, the older you get, the greater your risk of dehydration.
“It’s far more common in the elderly, due to medications and a reduced sense of thirst,” St. Pierre says. “And it can impact physical and mental health more profoundly in that group.”
Healthy aging strategy #3: Prioritize high-quality sleep.
Generally speaking, people who sleep less than seven or more than eight hours a night, and who go to bed and wake up at unpredictable times, are at higher risk for pretty much everything—obesity, diabetes, cardiovascular disease, and death from any cause.20,21
Establishing a regular, consistent sleeping-and-waking routine is probably the most powerful way to improve your sleep quality. (Bonus: It also helps to start that routine before midnight.)
One of the most impactful strategies to use to encourage good sleep is to employ a nightly bedtime ritual.
Just like Pavlov’s dogs learned to salivate at the sound of a bell, your body can learn to wind down with a custom-tailored pre-sleep routine.
About 30 minutes to an hour before bedtime, wrap up any stimulating activities (working, doomscrolling, intense exercise) and switch to activities that promote physical and mental relaxation. For example, read, take a bath or shower, do a mini yoga routine, or watch a favorite show.
Dim the lights, and maybe lower the thermostat a few degrees.
If you’re the ruminating type, consider doing a “brain dump.” Take a few minutes to write out a list of whatever’s bugging you: Emails you need to send or reply to, calls you have to make, project ideas, creative thoughts, that thing you should have said to that person…
Whatever’s on your mind, get it out of your head and onto your list.
(For more advice on how to engineer an excellent night’s sleep, check out our infographic: The power of sleep)
Healthy aging strategy #4: Deepen your human connections.
There’s one more key to a long, healthy life.
It’s something you can’t get with exercise, nutrition, or sleep. It’s impervious to wealth, fame, or professional achievement.
Tech bros can’t buy it, big pharma can’t replicate it, and longevity hustlers can’t sell it.
Good relationships, it turns out, are the ultimate life hack.
That’s according to the Harvard Study of Adult Development, which began in 1938 and continues today with the descendants of its original participants—Harvard undergrads (including future U.S. president John F. Kennedy) and teenage boys from underprivileged backgrounds.22
Robert Waldinger, MD, is the study’s fourth director. In his 2015 TED talk, he said it’s this simple:
“Good relationships keep us happier and healthier. Period.”
Participants who were most satisfied with their relationships at 50 were the healthiest at 80.
A 2016 study by Waldinger and his coauthors found that octogenarian participants who felt securely attached to their spouses—they believed they could count on them in life’s roughest moments—performed better on memory tests than those who felt less connected.23
“Think about relationships as something akin to physical fitness,” said Marc Schulz, PhD, associate director of the Harvard study, in a recent podcast interview.
To function, they require not just time and energy. At critical moments you also need to reflect on what is and isn’t working for you and the other person. And that applies to all important relationships—family, friends, neighbors, and colleagues as well as life partners.
Put another way: If you want a longer life, it helps to have a life.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Rudman, D., A. G. Feller, H. S. Nagraj, G. A. Gergans, P. Y. Lalitha, A. F. Goldberg, R. A. Schlenker, L. Cohn, I. W. Rudman, and D. E. Mattson. 1990. “Effects of Human Growth Hormone in Men over 60 Years Old.” The New England Journal of Medicine 323 (1): 1–6.1990
2. Walker, Richard F. 2006. “On the Evolution of Anti-Aging Medicine.” Clinical Interventions in Aging 1 (3): 201–3.
3. “Issue No. 164: What’s Trending in 2022?.” n.d. Fit Insider. Accessed January 22, 2024. https://insider.fitt.co/issue-no-164-whats-trending-in-2022/
4. Song C, Havlin S, Makse HA. 2009. “Self-similarity of complex networks.” Proceedings of the National Academy of Sciences, 106(33), 11448-11453.
5. McDonald, Roger B., and Rodney C. Ruhe. 2011. “Aging and Longevity: Why Knowing the Difference Is Important to Nutrition Research.” Nutrients 3 (3): 274–82.
6. Walker, Richard F. 2007. “What’s in a Name?” Clinical Interventions in Aging 2 (1): 1–2.
7. Pontzer, Herman, Yosuke Yamada, Hiroyuki Sagayama, Philip N. Ainslie, Lene F. Andersen, Liam J. Anderson, Lenore Arab, et al. 2021. “Daily Energy Expenditure through the Human Life Course.” Science 373 (6556): 808–12.
8. Addison, Odessa, Robin L. Marcus, Paul C. Lastayo, and Alice S. Ryan. 2014. “Intermuscular Fat: A Review of the Consequences and Causes.” International Journal of Endocrinology 2014 (January): 309570.
9. Veríssimo, João, Paul Verhaeghen, Noreen Goldman, Maxine Weinstein, and Michael T. Ullman. 2022. “Evidence That Ageing Yields Improvements as Well as Declines across Attention and Executive Functions.” Nature Human Behaviour 6 (1): 97–110.
10. Liu, Yong, Janet B. Croft, Anne G. Wheaton, Dafna Kanny, Timothy J. Cunningham, Hua Lu, Stephen Onufrak, Ann M. Malarcher, Kurt J. Greenlund, and Wayne H. Giles. 2016. “Clustering of Five Health-Related Behaviors for Chronic Disease Prevention Among Adults, United States, 2013.” Preventing Chronic Disease 13 (May): E70.
11. Gaesser, Glenn A., and Siddhartha S. Angadi. 2021. “Obesity Treatment: Weight Loss versus Increasing Fitness and Physical Activity for Reducing Health Risks.” iScience 24 (10): 102995.
12. Aggio, Daniel, Efstathios Papachristou, Olia Papacosta, Lucy T. Lennon, Sarah Ash, Peter Whincup, S. Goya Wannamethee, and Barbara J. Jefferis. 2020. “Trajectories of Physical Activity from Midlife to Old Age and Associations with Subsequent Cardiovascular Disease and All-Cause Mortality.” Journal of Epidemiology and Community Health 74 (2): 130–36.
13. Mandsager, Kyle, Serge Harb, Paul Cremer, Dermot Phelan, Steven E. Nissen, and Wael Jaber. 2018. “Association of Cardiorespiratory Fitness With Long-Term Mortality Among Adults Undergoing Exercise Treadmill Testing.” JAMA Network Open 1 (6): e183605.
14. Li, Ran, Jin Xia, X. I. Zhang, Wambui Grace Gathirua-Mwangi, Jianjun Guo, Yufeng Li, Steve McKenzie, and Yiqing Song. 2018. “Associations of Muscle Mass and Strength with All-Cause Mortality among US Older Adults.” Medicine and Science in Sports and Exercise 50 (3): 458–67.
15. Srikanthan, Preethi, and Arun S. Karlamangla. 2014. “Muscle Mass Index as a Predictor of Longevity in Older Adults.” The American Journal of Medicine 127 (6): 547–53.
16. Saeidifard, Farzane, Jose R. Medina-Inojosa, Colin P. West, Thomas P. Olson, Virend K. Somers, Amanda R. Bonikowske, Larry J. Prokop, Manlio Vinciguerra, and Francisco Lopez-Jimenez. 2019. “The Association of Resistance Training with Mortality: A Systematic Review and Meta-Analysis.” European Journal of Preventive Cardiology 26 (15): 1647–65.
17. Stamatakis, Emmanuel, Paul Kelly, Tessa Strain, Elaine M. Murtagh, Ding Ding, and Marie H. Murphy. 2018. “Self-Rated Walking Pace and All-Cause, Cardiovascular Disease and Cancer Mortality: Individual Participant Pooled Analysis of 50 225 Walkers from 11 Population British Cohorts.” British Journal of Sports Medicine 52 (12): 761–68.
18. Studenski, Stephanie, Subashan Perera, Kushang Patel, Caterina Rosano, Kimberly Faulkner, Marco Inzitari, Jennifer Brach, et al. 2011. “Gait Speed and Survival in Older Adults.” JAMA: The Journal of the American Medical Association 305 (1): 50–58.
19. Beaulieu, Kristine, Mark Hopkins, John Blundell, and Graham Finlayson. 2018. “Homeostatic and Non-Homeostatic Appetite Control along the Spectrum of Physical Activity Levels: An Updated Perspective.” Physiology & Behavior 192 (August): 23–29.
20. Jean-Louis, Girardin, Michael A. Grandner, and Seithikurippu R. Pandi-Perumal. 2021. “Sleep Health and Longevity-Considerations for Personalizing Existing Recommendations.” JAMA Network Open.
21. Mazzotti, Diego Robles, Camila Guindalini, Walter André Dos Santos Moraes, Monica Levy Andersen, Maysa Seabra Cendoroglo, Luiz Roberto Ramos, and Sergio Tufik. 2014. “Human Longevity Is Associated with Regular Sleep Patterns, Maintenance of Slow Wave Sleep, and Favorable Lipid Profile.” Frontiers in Aging Neuroscience 6 (June): 134.
22. “Harvard Second Generation Study.” n.d. Harvard Study. Accessed January 22, 2024. https://www.adultdevelopmentstudy.org/
23. Waldinger, Robert J., Shiri Cohen, Marc S. Schulz, and Judith A. Crowell. 2015. “Security of Attachment to Spouses in Late Life: Concurrent and Prospective Links with Cognitive and Emotional Wellbeing.” Clinical Psychological Science 3 (4): 516–29.
The post How to live the longest, healthiest life possible appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
“Cargo pants are back.”
This was the news that Brian St. Pierre, PN’s director of nutrition, broke when we met.
(St. Pierre, a father, found this out via his 12-year-old daughter.)
Why does this matter? Apparently, a certain type of exercise is running a parallel cycle: An old trend resurfacing as a new “it” thing.
Cardio’s back, baby.
Specifically, zone 2 cardio—also known as steady state cardio, low intensity steady state cardio (LISS), or what your treadmill may call the “fat burning zone” (more on this term later).
When I got into the fitness industry over a decade ago, cardio was at its peak of being disrespected.
“Are you trying to lose all your muscle??” the naysayers said.
St. Pierre—who’s coached top athletes in the NBA, NFL, MLB, and the NHL—remembered:
“You either did intervals, or you lifted. Maybe both. Steady state cardio was for endurance athletes only.”
Now, as steady state cardio makes its triumphant return, interval training seems to be getting tagged as overrated. (Lifting, of course, is as badass as ever.)
So, what’s the deal? Is there a “best” form of cardio? Is zone 2 exercise worthy of the hype?
In this article, you’ll find out. You’ll also learn:
- What zone 2 cardio is (and how to know when you’re “in it”)
- How much zone 2 cardio you should do per week to reap the health and fitness benefits
- How zone 2 cardio compares to other forms of exercise
- What the potential downsides of zone 2 cardio are—and how to mitigate them
Let’s get to it.
What is “zone 2 cardio,” anyway?
St. Pierre struggled to give a simple answer to this question. Not because he didn’t know, but because it’s a trickier question than you might think.
In a nutshell though:
Zone 2 cardio is sub-maximal aerobic training—meaning, aerobic exercise that’s performed below your maximum effort.
But St. Pierre offers some caveats:
“Zone 2 training could mean different things in different contexts,” he says.
“How elite athletes measure and train zone 2 is going to be different from what my mother would be doing.”
Elite endurance athletes use precise (often expensive) tools to ensure they’re in zone 2 (such as lactate meters and power meters). They strive to improve zone 2 fitness to maximize performance.
Regular people, though, tend to train in zone 2 without using gadgets—just some simple body awareness cues—with the likely goal of improving overall health.
Zone 2 cardio examples
Any intentional physical activity that feels stimulating, but still relatively easy—like you could go for an hour, or even hours—counts as zone 2 cardio work.
For example:
- Casual cycling
- Using the elliptical machine
- Hiking or walking uphill
- Rucking (walking with a weighted backpack or vest)
- Slow jogging on flat terrain
- Rowing (using a machine, or if you’re lucky, a canoe on a calm lake)
Zone 2 cardio compared to other cardiovascular “zones”
Different levels of exertion—as measured by heart rate—are categorized into five different “zones.”
(This is a common model, but here are other zone models that have seven zones. And models that are based on power rather than heart rate. See how quickly this can get complicated?)
Each zone will use different energy sources at different rates, and will have unique benefits, as the table below shows.
| Zone | % of Max Heart Rate | Main Energy source* | Feels like… | Examples | Benefits |
|---|---|---|---|---|---|
| 1 | <60% | Fat | Comfortable; can nasal breath easily and hold a conversation | Walking or light household activities | Increases overall activity, improves blood flow |
| 2 | 60-70% | Fat | Can maintain nasal breathing, but not comfortably | Light jogging, hiking, cycling, elliptical | Improves aerobic base without impeding recovery |
| 3 | 70-80% | Fat and carbs | Tough to maintain a conversation; will need to start breathing heavier | Jogging or cycling at faster pace (but not sprinting) | Improves aerobic and anaerobic fitness, and lactate threshold |
| 4 | 80-90% | Carbs | Huffing and puffing; might be able to get out a few words | Running, cycling or using a machine for for 1-4 minute sprints | Improves power output, VO2 max, lactate threshold, and overall athletic performance |
| 5 | >90% | Carbs | Near or at maximal effort; heart pounding and talking is impossible | Maximal sprinting | Improves VO2 max, heart rate max, and fitness at maximal levels |
Why zone 2 cardio is sometimes called “the fat burning zone”
Zone 2 cardio is a form of aerobic exercise.
Aerobic means “with oxygen,” which means the body needs oxygen in order to produce ATP—our primary source of energy—to power this kind of activity.
Anaerobic exercise—like sprinting, intense cycling, or heavy weightlifting—doesn’t require oxygen to produce the energy (ATP) needed to fuel it.
Instead, anaerobic activities use readily-available sources of energy—primarily carbohydrates stored in the muscles and liver. These energy sources can be accessed rapidly, but run out quickly. And, it takes time—and possibly a big sandwich—to replenish them.
Meanwhile, aerobic exercise taps into energy reserves gradually, primarily burning body fat for fuel. This process is slower, but the energy reserve is much larger (even among lean individuals) and thus can sustain activity for longer.
This is why the treadmill at your gym may call zone 2 cardio “the fat burning zone”.
When engaged in steady, moderately paced aerobic work, your body uses fat as its primary energy source.
If the term “fat burning” perked your ears, just keep the following in mind:
- Other forms of cardio—such as high intensity interval training (HIIT)—are equally effective in terms of fat loss, on average.1 2
- Exercise alone doesn’t tend to yield significant changes in body fat. Meaning: There’s nothing “magical” about zone 2 cardio’s ability to burn fat as it relates to losing fat and body weight.
Truly, the most effective exercise—in terms of fat loss and overall health benefits—will be the kind(s) you enjoy, and are able to do most consistently.
Three big benefits of zone 2 cardio
So, why might you incorporate zone 2 cardio work into your routine (or suggest your clients do the same)?
Let’s discuss three strong arguments for jumping on this trend.
Benefit #1: It builds your aerobic base.
St. Pierre offers this analogy:
“Imagine your overall cardio fitness is a pyramid: The base is your aerobic fitness, and the top is your peak anaerobic fitness,” he says.
“If you only train the peak, the structure is top heavy; it’s not built to last.”
This is one of the biggest assets of zone 2. Training at the peaks may be fun (in a masochistic way), but it’s not the best way to build your base.
To see how this works, let’s use an example with St. Pierre’s sport of choice: Hockey
On the ice, you’ll be mostly fueled by the anaerobic system.
With a strong aerobic base, you’ll recover quickly between “sprints” on the ice while resting on the bench.
Without a good aerobic base, your body may actually stay in an anaerobic state while you’re bench-warming. This not only inhibits recovery; it also drains precious energy reserves.
(And if you burn through your reserves in the first period, those second and third periods are going to suck.)
This ability to adapt to changes in physical demands is called metabolic flexibility4—and zone 2 cardio is particularly good at enhancing it.
With good metabolic flexibility, your body can toggle between energy sources as needed (instead of using mostly glucose or mostly fat all the time) to power activity, leading to better endurance, power, and performance.
Benefit #2: It’s exercise that gives more than it takes.
Intense workouts are both mentally and physically draining. They also “cost” a fair bit, from a recovery perspective.
Not zone 2 exercise.
“Zone 2 cardio may even help your recovery in between sessions,” says St. Pierre. “At worst, it’s going to be recovery neutral.”
Cycling on a bike at a relatively low intensity for 45 minutes might not be the most fun, but it’ll improve your overall fitness without adding much stress or demanding recovery in the same way intervals would.
If you have time to train five hours per week, but only have the energy to train all out for two to three hours, that still leaves you with time to train—just at a lower intensity.
Many folks have an “all or nothing” mindset and get mad at themselves for not being able to train like a beast for all five hours. But you don’t need to. Three hours of intense training and two hours of low intensity training is amazing.
Benefit #3: It boosts mitochondrial health—which might help you live better, longer.
One of the promises of zone 2 is that it can improve mitochondrial health.
Better mitochondrial health means a lowered risk of many diseases, such as type 2 diabetes, cardiovascular disease, metabolic syndrome, and cancer.5
Zone 2 cardio might be the most effective form of exercise to maximize mitochondrial health6 (though the research supporting this has participants doing many hours of zone 2 work per week).
Fortunately, all physical activity—including interval and resistance training—supports and improves mitochondrial health.7 8 9
Plus, effectiveness is a spectrum. Obsessing over having “the best mitochondrial health possible” is pointless if you can’t consistently perform the amount of exercise it takes to get there.
“How do I know if I’m in zone 2?”
Understandably, many people (including your clients) will ask. There are several ways to assess if you’re in zone 2, ranging from “fancy and high-tech” to “luddite-approved.”
Tracking method #1: Gadgets
If you’re a high level endurance athlete fixated on tracking hard data, a lactate meter will be your most accurate measurement tool.
If you’re just looking to achieve better overall health and aerobic fitness, you can use a heart monitor. (Try a chest strap or a wearable wrist watch that tracks heart rate.10)
Tracking method #2: Math
If you want to use your heart rate to calculate if you’re in zone 2—which is about 60 to 70 percent of your heart rate max—you first have to figure out your max heart rate.
The simplest way to estimate your heart rate max is to take 220 and subtract your age. Calculate 60 to 70 percent of that number, and you’ll get your target zone 2 heart rate range.
For example, if you’re 42 years old:
220 – 42 = 178 beats per minute is your maximum heart rate
0.6 (or 60%) x 178 = 106.8
0.7 (or 70%) x 178 = 124.6
So, if your heart rate is between 107 and 125 beats per minute, that puts you in zone 2.
(Another common approach: Take 180, subtract your age, and that’ll give you the top of your zone 2 range.)
Of course, if you’re in that range and can’t talk, nasal breath, or focus on anything other than just… keep… going, you’ll know you’re not in zone 2.
Sometimes, the body knows best. Which brings us to…
Tracking method #3: Body awareness
Without gadgets or formulas, can tell if you’re in zone 2 if:
- You’re doing a form of cardio that requires effort—but also feel like you could perform it for an extended period of time
- You can breathe through your nose
- You can talk (but perhaps not sing very well)
- You could pay attention to a podcast, movie, or have a thoughtful conversation
As St. Pierre eloquently put it:
“When you’re done with your session, you should be able to say you could do it again if not for time and boredom.”
TL;DR: Zone 2 work shouldn’t crush you.
How much zone 2 cardio should you do per week?
The shortest (and most practical) answer: Whatever you can fit in.
If you have more time and want some specificity, the WHO and the CDC suggest between 150-300 minutes of moderate-intensity aerobic activity per week.11 12
Weekly, that could look like three 30 minute-sessions, two 45 minute-sessions, or one longer 90-minute session.
But don’t get bogged down by specifics. Any cardio is great if you haven’t been doing any.
How long should zone 2 cardio sessions be?
You’ll commonly hear sessions need to be at least 45 minutes.
Your aerobic system doesn’t fatigue easily during zone 2 work, so duration is somewhat important if you’re aiming to maximize adaptations.
If you go with the WHO and CDC’s guidelines, two to three 45 to 75 minute sessions of zone 2 cardio per week is pretty ideal. (Note: If you’re a competitive athlete, you’ll probably need more.)
But if you can only fit in 25 or 30 minutes a week total, it’s not pointless.
“Any amount of activity improves health, so while yes, more is better, anything you can get in will make a difference for your wellbeing,” says St. Pierre.
You may not get the maximum benefits by doing less, but you’ll experience many amazing health improvements by getting in some cardio.
Factor in your goals.
Don’t get so fixated on zone 2 that you dedicate all your workout time to it and lose the benefits you can get from other kinds of training.
And, consider your fitness priorities.
If you want to build muscle and strength, resistance training should be the focus of your training. (In other words: Don’t cut your strength workouts in half just to squeeze in ideal zone 2 training targets.)
“I hate cardio” and other barriers to zone 2 work
Have you ever seen the show Suits? It’s not the Sopranos, but it’s entertaining and full of tea.
St. Pierre hadn’t seen it—that is until he started watching it while doing zone 2 work on his bike at home.
Zone 2 training isn’t his favorite way to train. With this, he found a way to make it enjoyable.
If you hate cardio, find ways to turn down the suck.
Here are a few ways to do that.
Consume that sweet, sweet content.
Whether it’s watching a fun TV show or listening to an audiobook or podcast, you can offset the tedium of zone 2 cardio with something you enjoy.
Play.
You can also get zone 2 work with sports or various leisure activities.
Personally, I like to shoot around the basketball with my heart rate monitor on. (Yes, there will be times I’m at a higher heart rate zone than what is truly zone 2, but that’s okay. I’m not an elite endurance athlete, so precision isn’t crucial.)
Grab your frisbee, pickleball racket, or ball-of-choice, and have fun.
Make it work with your schedule—and life.
“I just don’t have the time.”
If this is your primary obstacle, incorporate zone 2 cardio in a way that supports your life.
Some examples:
- If you can, bike to commute to work. Especially in busier cities with lots of traffic, this can actually be more time efficient than driving or taking transit.
- Run your errands with a purpose. Walk briskly to the store (or around the mall), and carry your groceries if you can.
- Do domestic chores like you mean it. More laborious house work such as cutting the grass, shoveling the snow, or vacuuming—anything that takes a while and takes some effort—counts.
- Run around with other animals. Your kids and your pets are hard to keep up with, right? Make their week and chase after them at the park or local rec center. Alternatively, pull them in a wagon or take a brisk walk pushing the stroller.
If these activities don’t keep you in zone 2 the entire time, that’s okay. These are just ideas for those who simply don’t have the time for more structured cardio.
Start with less.
If 45 minutes of anything still sounds like too much, just start with 10 minutes. You can always build up from there.
Ignore what’s optimal, and integrate what’s practical.
Something is truly better than nothing. (If you’re strapped for time, remember that line.)
Another tool in the kit
Trends in the fitness industry are cyclical. (Kind of like trends in pants-with-pockets.)
Training styles will come and go. When one comes back in, remember this and temper your response. Nothing—no food, exercise, or supplement—is a magic bullet.
The zone 2 cardio trend has been awesome for re-inspiring folks (including myself and St. Pierre) to do more cardio.
It’s also been confusing to some, leaving them even more stressed about how to train “the optimal way.”
At PN, we’re less fussed about what’s theoretically optimal than what’s practically optimal. Do the best you can. Find activities you enjoy. And do those consistently.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
-
- Kramer, Ana Marenco, Jocelito Bijoldo Martins, Patricia Caetano de Oliveira, Alexandre Machado Lehnen, and Gustavo Waclawovsky. 2023. “High-Intensity Interval Training Is Not Superior to Continuous Aerobic Training in Reducing Body Fat: A Systematic Review and Meta-Analysis of Randomized Clinical Trials.” Journal of Exercise Science and Fitness 21 (4): 385–94.
- Steele, James, Daniel Plotkin, Derrick Van Every, Avery Rosa, Hugo Zambrano, Benjiman Mendelovits, Mariella Carrasquillo-Mercado, Jozo Grgic, and Brad J. Schoenfeld. 2021. “Slow and Steady, or Hard and Fast? A Systematic Review and Meta-Analysis of Studies Comparing Body Composition Changes between Interval Training and Moderate Intensity Continuous Training.” Sports (Basel, Switzerland) 9 (11).
- Johns, David J., Jamie Hartmann-Boyce, Susan A. Jebb, Paul Aveyard, and Behavioural Weight Management Review Group. 2014. “Diet or Exercise Interventions vs Combined Behavioral Weight Management Programs: A Systematic Review and Meta-Analysis of Direct Comparisons.” Journal of the Academy of Nutrition and Dietetics 114 (10): 1557–68.
- Goodpaster, Bret H., and Lauren M. Sparks. 2017. “Metabolic Flexibility in Health and Disease.” Cell Metabolism 25 (5): 1027–36.
- San-Millán, Iñigo. 2023. “The Key Role of Mitochondrial Function in Health and Disease.” Antioxidants (Basel, Switzerland) 12 (4).
- Bishop, David J., Cesare Granata, and Nir Eynon. 2014. “Can We Optimise the Exercise Training Prescription to Maximise Improvements in Mitochondria Function and Content?” Biochimica et Biophysica Acta 1840 (4): 1266–75.
- Lim, Ai Yin, Yi-Ching Chen, Chih-Chin Hsu, Tieh-Cheng Fu, and Jong-Shyan Wang. 2022. “The Effects of Exercise Training on Mitochondrial Function in Cardiovascular Diseases: A Systematic Review and Meta-Analysis.” International Journal of Molecular Sciences 23 (20).
- Ruegsegger, Gregory N., Mark W. Pataky, Suvyaktha Simha, Matthew M. Robinson, Katherine A. Klaus, and K. Sreekumaran Nair. 2023. “High-Intensity Aerobic, but Not Resistance or Combined, Exercise Training Improves Both Cardiometabolic Health and Skeletal Muscle Mitochondrial Dynamics.” Journal of Applied Physiology 135 (4): 763–74.
- Porter, Craig, Paul T. Reidy, Nisha Bhattarai, Labros S. Sidossis, and Blake B. Rasmussen. 2015. “Resistance Exercise Training Alters Mitochondrial Function in Human Skeletal Muscle.” Medicine and Science in Sports and Exercise 47 (9): 1922–31.
- Hajj-Boutros, Guy, Marie-Anne Landry-Duval, Alain Steve Comtois, Gilles Gouspillou, and Antony D. Karelis. 2023. “Wrist-Worn Devices for the Measurement of Heart Rate and Energy Expenditure: A Validation Study for the Apple Watch 6, Polar Vantage V and Fitbit Sense.” European Journal of Sport Science: EJSS: Official Journal of the European College of Sport Science 23 (2): 165–77.
- Dishman, Rod K., Richard A. Washburn, and Dale A. Schoeller. 2001. “Measurement of Physical Activity.” Quest 53 (3): 295–309.
- CDC. 2023. “How Much Physical Activity Do Adults Need?” Centers for Disease Control and Prevention. June 28, 2023. https://www.cdc.gov/physicalactivity/basics/adults/index.htm
The post Zone 2 cardio: Flaky fitness trend or worthy pursuit? appeared first on Precision Nutrition.
Source: Health1
Angela Fitch’s family history of obesity caught up to her at age 40, when she was pregnant with her first child.
As a physician and obesity medicine specialist, Dr. Fitch knew the lifestyle levers to pull—and she had the financial means to yank them hard.
After giving birth, she lifted weights with a trainer twice a week. She sweated through one Peloton workout after another and tracked her food intake on MyFitnessPal.
Nevertheless, for the next decade, Dr. Fitch lost (and regained) the same five to ten pounds. Her blood pressure crept upward. Then came a sleep apnea diagnosis.
As her 50th birthday neared, Dr. Fitch decided to take the advice she gave her patients. She went on medication. (And, she lost 30 pounds.)
In the years since, Dr. Fitch has occasionally stopped her meds. For a few months, she maintains her results.
Eventually, however, the scale climbs back. For now, she’s decided that she’ll be on medication long-term.
If you’re a coach, how does this story land with you?
Does it…
… Make you feel disappointed? Does this seem like a story of someone “giving up” or “not trying hard enough”?
… Inspire you with a sense of awe? That modern medicine has figured out how to treat yet another chronic disease?
… Bring up questions? Like wondering about the effects of being on medication—potentially long-term? (Or if weight loss is even that relevant—so long as a person is eating healthy and exercising regularly?)
Dr. Fitch is now president of the Obesity Medicine Association and chief medical officer of Known Well, a primary care and obesity medicine practice in Needham, Massachusetts. Regardless of how you feel about her story, it illustrates what can initially seem like an inconvenient truth for those of us in the health coaching industry:
Behavior change on its own isn’t always enough.
For many people with obesity, semaglutide (Ozempic, Wegovy, Rebelsus), tirzepatide (Mounjaro, Zepbound), and other glucagon-like peptide-1 receptor agonists (GLP-1 RAs) serve as valuable tools that make significant and lasting weight loss possible.
But for health coaches, these drugs can seem like an existential threat.
You might wonder:
‘Who needs a nutrition coach or a personal trainer when people can get faster, easier, and more dramatic results with drugs?’
However…
People need health coaches now more than ever.
In this story, we’ll explain why—and show you how to turn “the golden age of obesity medicine” into a massive career opportunity.
With fat loss, there’s no such thing as an “easy way out.”
To manage diabetes or treat cancer, most people consider it normal and natural to combine lifestyle behaviors with prescription medicine.
No one would tell someone with cancer, “You’re on chemo? Way to take the easy way out!”
However, that’s what many people with obesity hear when they mention medication or surgery.
For decades, much of society hasn’t viewed obesity as the disease that it is.
Instead, people have seen it as a willpower problem.
The remedy: “Just try harder.”
However, rather than motivating people to succeed, this “remedy” often encourages them to give up. (More importantly, the willpower theory isn’t based on science.)
In reality, people with obesity likely have as much willpower as anyone else.
However, for them, fat loss is harder—because of genetics and physiology, along with social, cultural, behavioral, and/or environmental factors that work against them.
Why is it so difficult to lose fat?
Imagine life 150 years ago, before the invention of the automobile. To get from point A to point B, you had to walk, pedal a bicycle, or ride a horse.
Food was often in short supply, too. You had to expend calories to get it, and meals would just satisfy you (but not leave you feeling “full”).
Today, however…
“We live in an obesogenic environment that’s filled with cheap, highly-palatable, energy-dense foods [that make overeating calories easy, often unconsciously], and countless conveniences that reduce our physical activity,”
says Karl Nadolsky, MD, an endocrinologist and weight loss specialist at Holland Hospital and co-host of the Docs Who Lift podcast.
You might wonder: Why do some people gain fat in an obesity-promoting environment while others don’t?
The answer comes down to, in large part, genetics and physiology.
(Obesity is complex and multifactorial. As we noted above, there are other influential factors, but your genes and physiology are mostly out of your control, and so medication might be the best tool to modify their impact.)
Genetically, some people are more predisposed to obesity.
Some genes can lead to severe obesity at a very early age. However, those are pretty rare.
Much more common is polygenic obesity—when two or more genes work together to predispose you to weight gain, especially when you’re exposed to the obesogenic environment mentioned earlier.
People who inherit one or more of these so-called obesity genes tend to have particularly persistent “I’m hungry” and “I’m not full yet” signals, says Dr. Nadolsky.
Obesity genes also seem to cause some people to experience what’s colloquially known as “food noise.”
They feel obsessed with food, continually thinking, “What am I going to eat next? When is my next meal? Can I eat now?”
Physiologically, bodies tend to resist fat loss.
If you gain a lot of fat, the hormones in your gut, fat cells, and brain can change how you experience hunger and fullness.
“It’s like a thermostat in a house, but now it’s broken,” says Dr. Nadolsky. “So when people cut calories and weight goes down, these physiologic factors work against them.”
After losing weight, your gut may continually send out the “I’m hungry” signal, even if you’ve recently eaten, and even if you have more than enough body fat to serve as a calorie reserve. It also might take more food for you to feel full than, say, someone else who’s never been at a higher weight.
Enter: GLP-1 drugs
In 2017, semaglutide—a synthetic analog of the metabolic hormone glucagon-like peptide 1—was approved in the US as an antidiabetic and anti-obesity medication.
With the emergence of this class of drugs, science offered people with obesity a relatively safe and accessible way to lose weight long-term, so long as they continued the medication.
How Ozempic and other obesity medicines work
Current weight loss medications work primarily by mimicking the function of glucagon-like peptide 1 (GLP-1), which is a hormone that performs several functions:
- In the pancreas, it triggers insulin secretion, which helps regulate blood sugar.
- In the gut, it slows gastric emptying, affecting your sensation of fullness.
- In the brain, it reduces cravings (the desire for specific foods) and food noise (intrusive thoughts about food).
In people with obesity, the body quickly breaks down endogenous (natural) GLP-1, making it less effective. As a result, it takes longer to feel full, meals offer less staying power, and food noise becomes a near-constant companion, says Dr. Nadolsky.
Semaglutide (Ozempic, Wegovy, Rybelsus) and medicines like it flood the body with synthetically made GLP-1 that lasts much longer than the GLP-1 the body produces. This long-lasting effect helps increase feelings of fullness, reduce between-meal hunger, and muffle cravings and food noise.
Interestingly, by calming down the brain’s reward center, these medicines may also help people reduce addictive behaviors like problem drinking and compulsive gambling, says Dr. Nadolsky.
The lesser-known history of weight loss medicine
To understand the power of semaglutide (Ozempic, Wegovy, Rybelsus) and other GLP-1 medicines, it’s helpful to know a little about the drugs that predated it.
Decades before the age of Ozempic, physicians realized that several drugs originally developed to treat other conditions also seemed to help people lose weight.
These included:
- Qsymia, which pairs phentermine (an older weight loss medicine) with the epilepsy medicine topiramate
- Contrave, which combines the antidepressant bupropion (Wellbutrin) with naltrexone, used to treat addictions
- Metformin, a diabetes medicine
However, weight loss from these older medicines was modest, helping people to lose (and keep off) around 5 to 10 percent of their body weight.1 2 3
Around 2010, liraglutide (Victoza, Saxenda) was approved by the FDA to treat diabetes. Like Ozempic and other newer weight loss medicines, liraglutide mimics glucagon-like peptide-1 (GLP-1), but it’s less effective than the newer medicines.
Why does Ozempic get all the credit?
Ozempic has become the Kleenex of weight loss medicines—a name brand people toss around as if it’s generic.
This fame is at least partly earned: Dr. Fitch says that semaglutide (Ozempic, Rybelsus, Wegovy) also works more effectively than liraglutide, its GLP-1 predecessor.
“Semaglutide is 94 percent similar to our own GLP-1,” she says, “They’ve been able to make it closer and closer to the GLP-1 our bodies make.”
It also lasts longer than liraglutide, and more of it reaches the brain.
However, newer meds outperform Ozempic. (See the table in the section below.)
And there are other medicines—available orally rather than via injection—coming. These pills will be easier to mass produce, which will drive down costs and make GLP-1 medicines even more accessible to more people.
So, although Ozempic is the current reigning brand of the weight loss drug world, it may be ousted in time.
The growing effectiveness of weight loss drugs (especially in combination with lifestyle modifications)
Researchers measure a weight-loss medicine’s success based on the percentage of people who reach key weight loss milestones.
For example, most people start to see health benefits after losing five percent of their weight—and remission from disease after losing around 20 percent.
As the chart below shows, weight loss medicines have become increasingly effective at helping people to reach both milestones.
| Medicine | % of people who lose 5% of their weight | % of people who lose >20% of their weight |
|---|---|---|
| First-generation weight loss medicines (Qsymia, Contrave, Metformin) 4 5 6 | 53-80% | 10-20% |
| Semaglutide (Ozempic, Rybelsus, Wegovy) 7 8 | 86% | 32% |
| Tirzepatide (Mounjaro, Zepbound) 9 10 | 85-91% | 50-57% |
| Retatrutide (not yet FDA approved) 11 12 | 92-100% | 80-83% |
How do weight loss medications compare to traditional interventions?
In the past, weight loss interventions have focused on lifestyle modifications like calorie or macronutrient manipulation, exercise, and sometimes counseling.
Rather than pitting lifestyle changes against weight loss medicines or surgery, it’s more helpful to think of them all as tools.
As the graph below shows, the more weight loss tools someone uses—including coaching—the more significant the results.13 14 15 16
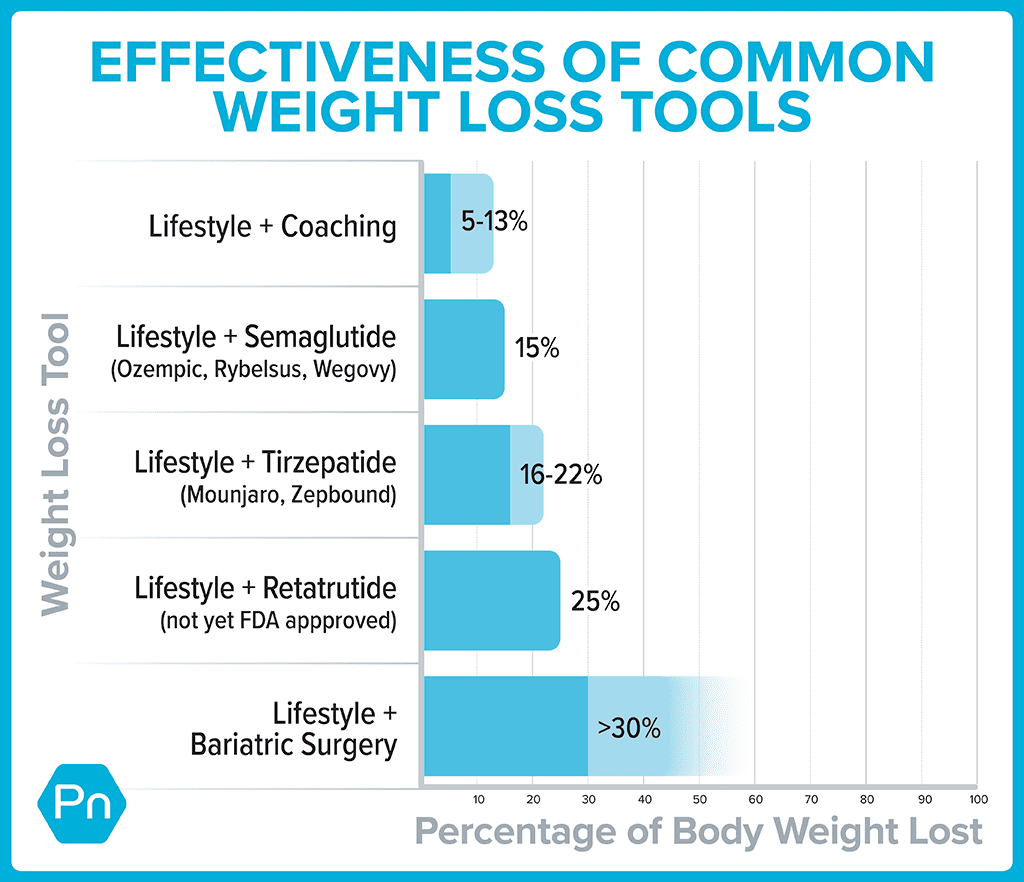
Fat loss often comes with powerful health benefits
For years, the medical community has told folks that losing 5 to 10 percent of their body weight was good enough.
Partly, this message was designed to right-set people’s expectations, as few lose much more than that (and keep it off) with lifestyle changes alone.
In addition, this modest weight loss also leads to measurable health improvements. Lose 5 to 10 percent of your total weight, and you’ll start to see blood sugar, cholesterol, and pressure drop.17
However, losing 15 to 20 percent of your weight, as people tend to do when they combine lifestyle changes with second-generation GLP-1s, and you do much more than improve your health. You can go into remission for several health problems, including:
- High blood pressure
- Diabetes
- Fatty liver disease
- Sleep apnea
That means, by taking a GLP-1 medicine, you might be able eventually to stop taking several other drugs, says Dr. Nadolsky.
Experts suspect GLP-1s may improve health even when no weight loss occurs.
“The medicines seem to offer additive benefits beyond just weight reduction,” says Dr. Nadolsky.
Research indicates that GLP-1s may reduce the risk of major cardiovascular events (heart attacks and strokes) in people with diabetes or heart disease.18 19 20 In people with diabetes, they seem to improve kidney function, too.21
The theory is that organs throughout the body have GLP-1 receptors on their cells. When the GLP-1s attach to these receptors in the kidneys and heart, they seem to protect these organs from damage.
For this reason, in 2023, the American Heart Association listed GLP-1 receptor agonists as one of the year’s top advances in cardiovascular disease.
Ozempic side effects
You’ve likely heard that slowed gastric emptying from GLP-1s can lead to nausea, constipation, and other GI woes.
That’s all true.
However, for most, these side effects are manageable, especially with the help of a few key strategies (which we’ll cover later).
For now, however, we’d like to hash out a particular downside you’ve likely heard about from the media—because it offers a huge opportunity for health coaches.
When people take GLP-1 weight loss medicines, about 30 to 40 percent of the weight they lose can come from lean mass.22 23 24
Put another way: For every 10 pounds someone loses, about six to seven come from fat and three to four from muscle, bone, and other non-fat tissues.
This statistic has been broadcast among many media outlets in recent weeks as a dire warning against taking Ozempic, Wegovy, or Zepbound.
Such stories often fail to mention two important caveats:
Caveat #1: People with severe obesity generally have more muscle and bone mass than others.
To understand why, imagine you were forced to wear a 100- or 200-pound body suit every day for a year. Everyday activities—getting in and out of chairs, walking to and from the mailbox, climbing steps into a building—would feel like a resistance workout.
That’s likely partly why bariatric surgery patients experience a nine-year extension on their life expectancy, despite 30 percent of their weight loss coming from lean mass. They have more muscle than average to begin with, and therefore can safely lose some.25 26
For people with severe obesity, the health boost from body fat loss offsets the health risk of muscle and bone loss, says Dr. Fitch.
That said, there’s a caveat to the caveat: People who are only 30 pounds or so overweight may not be starting out with muscle and bone mass to spare. Especially if they’re older, they may begin their weight loss journey already under-muscled, with relatively low bone density. In those people, another drop in lean mass and bone density can add up to big health problems.
However…
Caveat #2: Muscle and bone loss aren’t inevitable.
As Dr. Nadolsky puts it, “Muscle loss isn’t a reason to avoid treating obesity [with medication]. It’s a reason to do more exercise.”
This is where coaches can shine.
By showing clients how to adopt muscle-building behaviors like strength training, combined with adequate protein consumption, you can help people offset the worst of the side effects when taking these medicines.
The yo-yo problem
GLP-1s are expensive, costing roughly $1000 USD a month. As a result, many insurers either refuse to cover them or limit their coverage to a year or two.
Once the money runs out, people tend to go off the meds—and the hunger and cravings return.
If they’ve done little to change their foundational eating habits, this puts them at a significant disadvantage. If they’re not eating slowly and mindfully and improving satiety with veggies and lean protein, the return of hunger and food noise can be overpowering.
That’s likely why, in one study, participants who stopped taking semaglutide regained, on average, two-thirds of the weight they’d lost.27
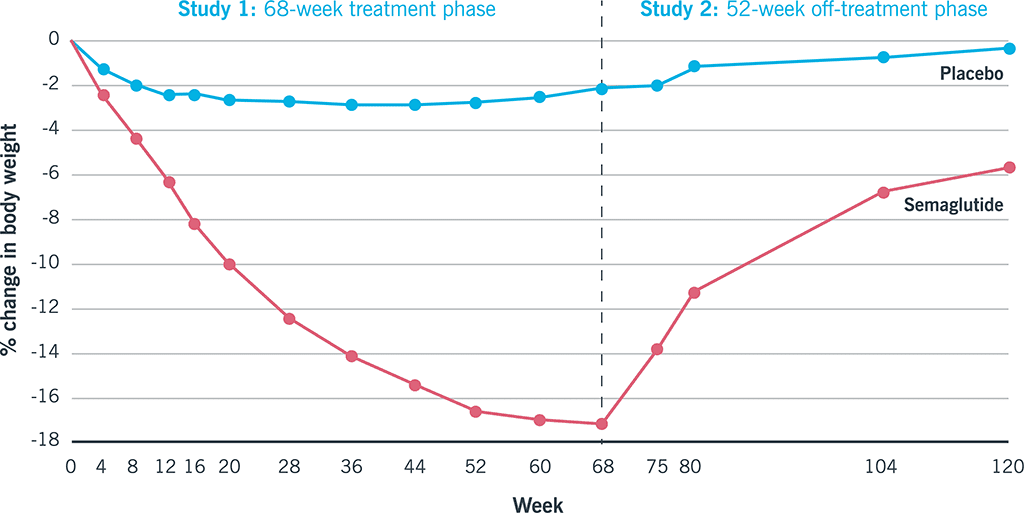
Again, here’s another opportunity for coaches…
Use weight loss medicine as a key that unlocks lifestyle changes.
Weight loss medicines don’t render behavior-based strategies obsolete; they make them more critical.
When GLP-1 medicines muffle food noise and hunger, your client will find it easier to prioritize protein, fruits and veggies, legumes, and other minimally processed whole foods. Similarly, as the scale goes down, clients feel better, so they’re more likely to embrace weight lifting and do other forms of exercise.
According to a 2024 consumer trends survey, 41 percent of GLP-1 medicine users reported that their exercise frequency increased since going on the medication. The majority of them also reported an improvement in diet quality, choosing to eat more protein, as well as fruits and vegetables.28
This is great news, because, as mentioned above, lifestyle changes are critical to preserving lean mass and preventing regain, should clients choose to discontinue medication.
When working with clients on GLP-1s, keep the following challenges in mind.
Coaching strategy #1: Find ways to eat nutritiously despite side effects.
The slowed stomach emptying caused by GLP-1 drugs can trigger nausea and constipation.
Fortunately, for most people, these GI woes tend to resolve within several weeks.
However, if you’re working with a client who’s experiencing a lot of nausea, they won’t likely welcome salads into their lives with open arms. (Think of how you feel when you have the stomach flu. A bowl of roughage doesn’t seem like it’ll “go down easy.”)
Instead, help clients find more palatable ways to consume nutritious foods. (For example, fruits and vegetables in the form of a smoothie or pureed soup might be easier.)
Dr. Nadolsky also suggests people avoid the following common offenders:
- Big portions of any kind
- Greasy, fatty foods
- Highly processed foods
- Any strong food smells that trigger a client’s gag reflex
- Sugar alcohols (like xylitol, erythritol, maltitol, and sorbitol, often found in diet sodas, chewing gum, and low-sugar protein bars), which can trigger diarrhea in some
Coaching strategy #2: Prioritize strength training.
To preserve muscle mass, aim for at least two full-body resistance training sessions a week.
In addition, move around as much as you can. Walking and other forms of physical activity are vital for keeping the weight off—and can help to move food through the gut to ease digestion.29 30
(Need inspiration for strength training? Check out our free exercise video library.)
Coaching strategy #3: Lean into lean protein.
In addition to strength training, protein is vital for helping to protect muscle mass.
You can use our free macros calculator to determine the right amount of protein for you or your client. (Spoiler: Most people will need 1 to 2 palm-sized protein portions per meal, or about 0.5 to 1 gram of protein per pound of bodyweight per day.)
Coaching strategy #4: Fill your plate with fruit and veggies.
Besides being good for your overall health, whole, fresh, and frozen produce fuels you with critical nutrients that can help drive down levels of inflammation.
In addition to raising your risk for disease, chronic inflammation can block protein synthesis, making it harder to maintain muscle mass.
(Didn’t know managing inflammation matters when it comes to preserving muscle? Find out more muscle-supporting strategies here: How to build muscle strength, size, and power)
Coaching strategy #5: Choose high-fiber carbs over low-fiber carbs.
Beans, lentils, whole grains, and starchy tubers like potatoes and sweet potatoes are more likely to help clients feel full and manage blood sugar than lower-fiber, more highly processed options.
(Read more about the drawbacks—and occasional benefits—of processed foods here: Minimally processed vs. highly processed foods.)
Coaching strategy #6: Choose healthy fats.
Healthy fats can help you feel full between meals and protect your overall health. Gravitate toward fats from whole foods like avocado, fatty fish (which is also a protein!), seeds, nuts, and olive oil—using them to replace less healthy fats from highly processed foods.
(Not sure which fats are healthy? Use our 3-step guide for choosing the best foods for your body.)
Coaching strategy #7: Build resilient habits.
It may go without saying, but the above suggestions are just the start.
(There’s also: quality sleep, social support, stress management, and more.)
Most importantly, clients need your help to make all of the above easier and more automatic.
And that’s the real gift of coaching: You’re not merely helping clients figure out what to eat and how to move; You’re showing them how to remove barriers and create systems and routines so their road to health is a little smoother.
That way, if they do need to stop taking medication, their ingrained lifestyle habits (that the medicine made easier for them to adopt) will make it more likely that they maintain their results.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
- Hendricks EJ. Off-label drugs for weight management. Diabetes Metab Syndr Obes. 2017 Jun 10;10:223–34.
- Lonneman DJ Jr, Rey JA, McKee BD. Phentermine/Topiramate extended-release capsules (qsymia) for weight loss. P T. 2013 Aug;38(8):446–52.
- Sherman MM, Ungureanu S, Rey JA. Naltrexone/Bupropion ER (Contrave): Newly Approved Treatment Option for Chronic Weight Management in Obese Adults. P T. 2016 Mar;41(3):164–72.
- Apolzan JW, Venditti EM, Edelstein SL, Knowler WC, Dabelea D, Boyko EJ, et al. Long-Term Weight Loss With Metformin or Lifestyle Intervention in the Diabetes Prevention Program Outcomes Study. Ann Intern Med. 2019 May 21;170(10):682–90.
- Sherman MM, Ungureanu S, Rey JA. Naltrexone/Bupropion ER (Contrave): Newly Approved Treatment Option for Chronic Weight Management in Obese Adults. P T. 2016 Mar;41(3):164–72.
- Lonneman DJ Jr, Rey JA, McKee BD. Phentermine/Topiramate extended-release capsules (qsymia) for weight loss. P T. 2013 Aug;38(8):446–52.
- Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021 Mar 18;384(11):989–1002.
- Garvey WT, Batterham RL, Bhatta M, Buscemi S, Christensen LN, Frias JP, et al. Two-year effects of semaglutide in adults with overweight or obesity: the STEP 5 trial. Nat Med. 2022 Oct;28(10):2083–91.
- le Roux CW, Zhang S, Aronne LJ, Kushner RF, Chao AM, Machineni S, et al. Tirzepatide for the treatment of obesity: Rationale and design of the SURMOUNT clinical development program. Obesity. 2023 Jan;31(1):96–110.
- Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med. 2022 Jul 21;387(3):205–16.
- Jastreboff AM, Kaplan LM, Frías JP, Wu Q, Du Y, Gurbuz S, et al. Triple-Hormone-Receptor Agonist Retatrutide for Obesity – A Phase 2 Trial. N Engl J Med. 2023 Aug 10;389(6):514–26.
- Frias JP, Deenadayalan S, Erichsen L, Knop FK, Lingvay I, Macura S, et al. Efficacy and safety of co-administered once-weekly cagrilintide 2·4 mg with once-weekly semaglutide 2·4 mg in type 2 diabetes: a multicentre, randomised, double-blind, active-c,ontrolled, phase 2 trial. Lancet. 2023 Aug 26;402(10403):720–30.
- Leung, Alice W. Y., Ruth S. M. Chan, Mandy M. M. Sea, and Jean Woo. 2017. An Overview of Factors Associated with Adherence to Lifestyle Modification Programs for Weight Management in Adults. International Journal of Environmental Research and Public Health 14 (8).
- Maciejewski, Matthew L., David E. Arterburn, Lynn Van Scoyoc, Valerie A. Smith, William S. Yancy Jr, Hollis J. Weidenbacher, Edward H. Livingston, and Maren K. Olsen. 2016. Bariatric Surgery and Long-Term Durability of Weight Loss. JAMA Surgery 151 (11): 1046–55.
- Ryan DH, Yockey SR. Weight Loss and Improvement in Comorbidity: Differences at 5%, 10%, 15%, and Over. Curr Obes Rep. 2017 Jun;6(2):187–94.
- Marx N, Husain M, Lehrke M, Verma S, Sattar N. GLP-1 Receptor Agonists for the Reduction of Atherosclerotic Cardiovascular Risk in Patients With Type 2 Diabetes. Circulation. 2022 Dec 13;146(24):1882–94.
- Lincoff AM, Brown-Frandsen K, Colhoun HM, Deanfield J, Emerson SS, Esbjerg S, et al. Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes. N Engl J Med. 2023 Dec 14;389(24):2221–32.
- Kosiborod MN, Abildstrøm SZ, Borlaug BA, Butler J, Rasmussen S, Davies M, et al. Semaglutide in Patients with Heart Failure with Preserved Ejection Fraction and Obesity. N Engl J Med. 2023 Sep 21;389(12):1069–84.
- Karakasis P, Patoulias D, Fragakis N, Klisic A, Rizzo M. Effect of tirzepatide on albuminuria levels and renal function in patients with type 2 diabetes mellitus: A systematic review and multilevel meta-analysis. Diabetes Obes Metab [Internet]. 2023 Dec 20.
- Ida S, Kaneko R, Imataka K, Okubo K, Shirakura Y, Azuma K, et al. Effects of Antidiabetic Drugs on Muscle Mass in Type 2 Diabetes Mellitus. Curr Diabetes Rev. 2021;17(3):293–303.
- Wilding JPH, Batterham RL, Calanna S, Van Gaal LF, McGowan BM, Rosenstock J, et al. Impact of Semaglutide on Body Composition in Adults With Overweight or Obesity: Exploratory Analysis of the STEP 1 Study. J Endocr Soc. 2021 May 3;5(Supplement_1):A16–7.
- Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021 Mar 18;384(11):989–1002.
- Reinmann A, Gafner SC, Hilfiker R, Bruyneel AV, Pataky Z, Allet L. Bariatric Surgery: Consequences on Functional Capacities in Patients With Obesity. Front Endocrinol. 2021 Apr 1;12:646283.
- Carlsson LMS, Carlsson B, Jacobson P, Karlsson C, Andersson-Assarsson JC, Kristensson FM, et al. Life expectancy after bariatric surgery or usual care in patients with or without baseline type 2 diabetes in Swedish Obese Subjects. Int J Obes. 2023 Oct;47(10):931–8.
- Wilding JPH, Batterham RL, Davies M, Van Gaal LF, Kandler K, Konakli K, et al. Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab. 2022 Aug;24(8):1553–64.
- Consumer trends: 2024 Food & Wellness special. The New Consumer. (n.d.). https://newconsumer.com/trends/consumer-trends-2024-food-wellness/
- Gorgojo-Martínez JJ, Mezquita-Raya P, Carretero-Gómez J, Castro A, Cebrián-Cuenca A, de Torres-Sánchez A, et al. Clinical Recommendations to Manage Gastrointestinal Adverse Events in Patients Treated with Glp-1 Receptor Agonists: A Multidisciplinary Expert Consensus. J Clin Med Res [Internet]. 2022 Dec 24;12(1).
- Tantawy SA, Kamel DM, Abdelbasset WK, Elgohary HM. Effects of a proposed physical activity and diet control to manage constipation in middle-aged obese women. Diabetes Metab Syndr Obes. 2017 Dec 14;10:513–9.
The post Ozempic for weight loss: What coaches (and clients) need to know about GLP-1 drugs appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
Calorie manipulation—whether to lose weight or gain muscle—seems simple.
After all, it’s just math… right?
Sort of. But it’s tricky.
Your body is a complex machine. In order to determine how many calories your body needs to achieve your goals, you need to first understand how your body burns (and stores) calories.
Want to find out more about what your body does with calories? Keep reading.
What’s the average necessary daily calorie intake?
The concept of a calorie is grounded in tangible science: One calorie equals the energy needed to raise the temperature of 1 gram of water by 1 degree Celsius.
Caloric needs can vary significantly from person to person, depending on various factors. These factors include your gender-assigned-at-birth, age, height, and overall lifestyle.
Generally speaking, adults require approximately 1,600 to 3,000 Calories per day.
(Yes, that’s a huge range. So obviously, your individual needs might differ.)
The foods you eat and their quantities dictate the number of calories you consume.
Consuming more calories than your body expends leads to weight gain, while consuming fewer calories than your body expends in weight loss—including fat and eventually muscle mass.
Making food choices based on calorie count is a common practice for people striving to lose or maintain weight. Calories are derived from the macronutrients of carbohydrates, fats, proteins, and other sources like alcohol.
The timing and frequency of meals also impact energy use, as your body’s energy expenditure fluctuates throughout the day.
What factors affect how many calories you need per day?
As we mentioned above, several factors influence your daily calorie needs. Let’s go into more detail about these factors and how they work together.
1. Age
As you age, your metabolism naturally slows down, so your body requires fewer calories.
This is why teenagers, with their active growth phases, usually need more calories compared to middle-aged adults.
2. Height and weight
Your physical dimensions (height and weight) as well as your body composition (muscle and fat ratios) play a role in caloric calculations.
Those who are larger—either taller, or they have a higher percentage of muscle mass—may burn more calories at rest and require more calories to sustain their daily needs.
3. Gender and hormones
Gender-assigned-at-birth and hormonal differences significantly influence caloric needs.
Men often have higher muscle mass and a faster metabolism, necessitating more calories.
Affected by hormonal fluctuations, women may experience appetite and energy expenditure variations throughout their menstruating years.
4. Activity level
Your lifestyle and activity level have an enormous impact on caloric requirements.
Those with physically demanding jobs or who engage in vigorous exercise will naturally burn more calories and need a higher intake to maintain energy balance.
Of course, the reverse is true for those who have sedentary jobs (such as desk jobs) and don’t intentionally exercise much.
5. Medical conditions and medications
Certain medical conditions, like thyroid disorders, can affect your metabolism and alter your caloric needs.
Additionally, certain medications might influence appetite, energy expenditure, or nutrient absorption, further impacting your daily calorie needs.
6. Basal Metabolic Rate (BMR)
Your basal metabolic rate represents the energy your body expends at rest to perform essential functions like breathing, circulating blood, and maintaining body temperature.
BMR is influenced by genetics, muscle mass, and age, all of which contribute to your daily caloric requirements.
We’ll discuss BMR and how it works alongside other body processes in greater detail below.
7. Goals
Whether you aim to lose weight, gain muscle, or maintain your current physique, your goals shape your caloric needs.
Weight loss typically involves a controlled reduction in caloric intake, while muscle gain demands additional calories to support growth and repair.
What processes affect how you burn calories?
Here are the various ways your body burns calories.
Exercise Activity Thermogenesis (EAT)
EAT refers to the energy your body expends during intentional physical activity, such as walking, running, lifting weights, fitness classes, or any other exercise you incorporate into your routine.
Contrary to common belief, EAT constitutes a relatively small portion of your total energy expenditure—approximately five to ten percent on average.
(Like everything, this percentage can vary.)
For most individuals, while EAT is undoubtedly beneficial for overall health and well-being, its direct impact tends to be minimal; the broader context of your overall energy expenditure matters more.
Non-Exercise Activity Thermogenesis (NEAT)
Non-Exercise Activity Thermogenesis (NEAT) encompasses the calories burned through your everyday physical movements outside of structured exercise routines.
It’s the energy your body expends when you engage in activities like cooking, cleaning, shopping, or even fidgeting—actions that don’t fall under planned exercise or sports.
Despite its inconspicuousness, NEAT holds remarkable potential to influence your metabolic rate and calorie burning. NEAT can contribute up to 15 to 30 percent of your daily caloric expenditure. While it’s not a substitute for vigorous workouts, that’s a noteworthy portion of the calories you burn every day.
Environmental conditions, genetics, job type, and lifestyle all contribute to NEAT’s variability from person to person. A sedentary job and an active profession might result in notable differences in daily calories burned.
Research has highlighted NEAT’s role in promoting wellness. A study tracking over 12,000 women for 12 years demonstrated that activities like fidgeting could mitigate the risks associated with prolonged sedentary behavior.
If you want to increase your NEAT, subtle changes like opting for a standing desk at work instead of sitting—which burns more calories per hour—can help.
NEAT’s influence extends beyond just calorie burn—it encourages a lifestyle that values movement throughout the day. This impacts on your overall energy balance—but maybe even your long term quality of life too.
Basal Metabolic Rate (BMR)
BMR, often referred to as your “resting metabolic rate,” represents the energy your body expends to maintain essential functions while at complete rest.
These include vital activities like your heartbeat, respiration, cell regeneration, body temperature maintenance, and all the other foundational biological activities required to sustain life when you’re inactive.
BMR calculators tell us that, on average, BMR constitutes about 60 to 70 percent of your daily energy expenditure. However, accurate BMR calculation requires a 12-hour fast, sufficient sleep, and absolute rest devoid of physical exertion.
Age, body composition, hormones, and body shape influence your BMR:
 Children and adolescents exhibit higher rates due to ongoing growth demands, while adults experience a gradual decline as the body shifts from building to breaking down.
Children and adolescents exhibit higher rates due to ongoing growth demands, while adults experience a gradual decline as the body shifts from building to breaking down.
 Individuals with more muscle have higher BMRs, as muscles demand more energy for maintenance. Conversely, higher proportions of body fat will lower BMR since fatty tissue requires minimal energy upkeep.
Individuals with more muscle have higher BMRs, as muscles demand more energy for maintenance. Conversely, higher proportions of body fat will lower BMR since fatty tissue requires minimal energy upkeep.
 Gender-assigned-at-birth also matters, with men generally possessing higher BMRs due to higher average muscle mass.
Gender-assigned-at-birth also matters, with men generally possessing higher BMRs due to higher average muscle mass.
 Hormones, like thyroxine from the thyroid gland, also influence BMR. Thyroxine levels correlate with metabolic rate: Elevated levels increase BMR, while reduced levels decrease it.
Hormones, like thyroxine from the thyroid gland, also influence BMR. Thyroxine levels correlate with metabolic rate: Elevated levels increase BMR, while reduced levels decrease it.
Thermic Effect of Food (TEF)
The Thermic Effect of Food (TEF) is how your body expends energy during the processes of digestion, absorption, and metabolism of the food you consume.
Think of TEF as the energy cost your body pays to process the nutrients from your meals.
TEF accounts for roughly ten percent of your caloric intake in a day. So, if you consume 2,000 calories, around 200 calories are expended just through eating and digestion.
The composition of your food profoundly influences TEF. Different macronutrients (carbs, fats, and protein) require varying levels of energy for digestion and metabolism.
Protein and complex carbohydrates have a higher thermic effect, demanding more energy for breakdown. In contrast, fats and simple carbohydrates have a lower thermic effect, necessitating comparatively less energy expenditure.
To delve into specifics, here’s how macronutrients impact TEF:
- Fat: 9 calories per gram; TEF ranges from 0-5 percent
- Carbohydrate: 4 calories per gram; TEF ranges from 5-15 percent
- Protein: 4 calories per gram; TEF ranges from 20-30 percent
This is one of the reasons a high-protein diet has a metabolic advantage and contributes to prolonged satiety. Same with choosing minimally processed, complex carbohydrates over simple carbohydrates.
Fats exhibit the lowest thermic effect, but despite this, healthy fats like those found in avocados, salmon, nuts, and seeds play vital roles in maintaining bodily functions, safeguarding organs, and providing energy source.
Factors like age, insulin resistance, and physical activity levels also influence TEF. For example, physically active individuals experience higher TEF.
And in case you’ve ever wondered, what you eat is definitely more important than when you eat. While some believe a large breakfast boosts daily calorie burn, the impact of meal timing on TEF remains inconclusive.
TDEE: Your Total Daily Energy Expenditure
Total Daily Energy Expenditure (TDEE) is the comprehensive sum of energy your body expends in a single day.
These components, which we’ve discussed above, add up to your TDEE:
| Basal Metabolic Rate (BMR) Your BMR reflects the calories your body consumes while performing essential functions at rest. This constitutes roughly 70 percent of your TDEE and encompasses activities like breathing, circulating blood, and supporting brain function. |
Thermic Effect of Food (TEF) TEF denotes the energy needed to digest, absorb, and metabolize the foods you consume. Around 10 percent of your TDEE stems from TEF, but this can vary based on your diet. Foods high in protein or complex carbs require more energy for processing, boosting TEF. |
| Exercise Activity Thermogenesis (EAT) EAT contributes a small portion, approximately 5 percent, to your TDEE. It includes the calories burned during intentional exercise like hitting the gym, jogging, or yoga. |
Non-Exercise Activity Thermogenesis (NEAT) NEAT accounts for the remaining 15 percent of your TDEE. It includes the energy expended during your daily non-exercise activities, such as walking, fidgeting, and household chores. |
As you can see, BMR is the calorie-burning foundation, and is boosted by EAT, NEAT, and TEF.
The sum of these define your daily calorie needs and calories burned.
If you’re working toward a specific fitness goal—weight loss or muscle gain, for example—your TDEE and your calorie needs will change as you progress. As you lose fat or build muscle, your metabolism will adapt to your new body composition, impacting your calorie needs along your fitness journey.
We can help you meet your goals
Knowing—and meeting—your daily calorie needs is integral to many health and fitness goals.
To figure out how many calories you need to meet your goals, try our Weight Loss Calculator or Ultimate Macro Calculator.
Whatever your goals, Precision Nutrition can help you reach them.
The post Everything you need to know about calculating your daily calorie needs appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
Health coaching goes beyond diet and exercise advice.
To improve your health, a good health coach will not just consider your physical needs, but also your goals, personal preferences, and overall value system.
There are many reasons why you might decide to work with a health coach, but many people haven’t considered just how much a health coach can help—and how they can help.
Below, we’ll look at four ways a health coach can benefit you that you might not have known about.
First, what is a health coach?
A health coach is a guide, someone who assists you in cultivating and maintaining healthy habits to meet your individual needs and goals. They collaborate with you to set personalized goals, devise actionable plans, establish accountability, and make sure you understand the strategies you’ll use to create positive change.
Health coaches address diverse health concerns. Their role goes beyond giving advice—they actively support you in implementing sustainable lifestyle changes.
From weight loss to stress relief or managing a health crisis, a health coach can help you take charge of your life for the better.
4 lesser-known reasons to work with a health coach
There are many reasons to hire a health coach, but here are some you may not have considered.
Reason #1: You’re recovering from an injury that impacts your movement.
If you’ve already completed physical therapy, engaging a health coach can be a logical next step for lasting recovery. Health coaches aren’t a substitute for medical care. However, they can support individuals looking to maintain—or even gain— mobility, muscle mass, and overall athletic ability.
A health coach will collaborate with you to develop a personalized plan that aligns with your physical capabilities as well as any restrictions cautioned by your doctor or physical therapist. They can guide you toward healthy movement patterns through tailored exercises and lifestyle adjustments that complement your recovery.
Many health coaches are experts in post-injury recovery. They provide support and motivation to help you navigate the challenges of rebuilding strength and mobility post-injury. They also know how to address the mental and emotional dimensions of recovery for your overall well-being, which we’ll discuss in more detail below.
Reason #2: You’re interested in improving your Deep Health.
While you might have heard that health coaches can assist with fitness and nutrition, what may separate them from many personal trainers or dieticians is their holistic approach.
Health coaches recognize the interconnectedness of different factors that contribute to your overall well-being, including stress, sleep, and mental health.
They work with you to identify areas that may be impacting your overall wellness, including your job and relationships, and collaboratively devise strategies to address them.
(To read more about Deep Health, PN’s term for thriving in all areas of life, check out: The Deep Health Assessment: How’s your health… REALLY?)
Reason #3: You want to be an active participant in your health and wellness.
Partnering with a health coach offers you the opportunity to have a more active role in your health. This dynamic relationship allows you to take control of your well-being while also benefiting from the guidance and expertise of a professional.
A health coach can help you discover and develop your “owner’s manual,” and you can use this self-knowledge and awareness to keep making decisions that support your unique needs and goals.
Your health coach serves as a resource to provide you with valuable insights and knowledge about self-care and goal setting. They’ll share with you the tools to understand your own needs better so you can make informed choices that align with your health objectives. Through two-way communication, your feedback, questions, concerns, and thoughts are actively integrated into your wellness process.
Reason #4: You’re focused on your long-term health.
While immediate health concerns often drive individuals to seek support, the lasting impact of a health coach lies in their ability to guide you toward practices that prevent chronic illnesses and negative health impacts for the rest of your life.
In addition to healthy nutrition practices, this includes maintaining your muscle tone to increase your balance and stability, thereby helping to prevent falls or other injuries as you get older.
A health coach will work with you to develop sustainable habits tailored to your lifestyle, abilities, preferences, stage of life, what foods you enjoy or avoid, and more.
Think of a health coach as an investment in your well-being for many years to come.
How to pick a health coach
If you’ve decided that a health coach can benefit you, make sure you do your research and choose several options that you can interview one-on-one. Look for coaches with a record of assisting clients in situations similar to yours.
Discuss their ability to tailor their approach and make sure they can answer any questions you might have about what makes your situation unique.
A good health coach should also ask you a lot of questions in return. They too want to make sure the relationship is a good fit, as well as understand your circumstances and history. When speaking with a health coach, make sure to be open and honest about your goals, your lifestyle, and your expectations from the partnership.
Remember that this is a collaborative and supportive relationship. So effective communication is key. Work with someone who listens well and provides reasonable and actionable answers that make sense to you. You should like your health coach, and further feel like they are trustworthy and comfortable to be around.
We’re here to help you reach your goals
The health coaches at Precision Nutrition are certified experts who can help you realize long-term wellness goals.
They meet you where you are and tailor programs that focus on your individual needs and lifestyle. Our Precision Nutrition 1:1 Coaching Program is designed to keep you motivated, help you develop positive habits, and see results.
Learn more today about how to work with us so you can feel your best.
The post 4 lesser-known reasons to work with a health coach appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
Not all foods fit into neat macro categories.
Meeting your macro goals can seem simple on paper or on an orderly spreadsheet, but in real life, it can sometimes feel more like a child’s finger painting.
Finding foods that align perfectly with your macro targets can be challenging, making the task of accurately tracking your intake feel impossible.
While there are many apps that can help you track the nutritional breakdown of each food you eat, using an app doesn’t work for everyone.
For those trying to track macros without the assistance of an app in your back pocket, you might have questions about how exactly some foods fit into different macro categories.
Luckily, there are multiple strategies available to help.
In this post, we’ll go over methods and solutions for accommodating foods that don’t naturally fit into a single macro category—from individual foods like beans (which contain both protein and carbs) to dishes like soup or stew (that might contain a mix of macronutrients).
A brief review of the macro categories: Carbs, protein, and fat
Before we start exploring foods that don’t easily fit into traditional macro categories, let’s take a minute to get a solid understanding of macro basics.
Carbohydrates, protein, and fat are the three macronutrients that our bodies need in large amounts. They provide us with energy, help build and repair tissues, and protect our organs.
- Carbohydrates are our body’s main source of energy. They’re found in foods like bread, pasta, rice, fruits, beans, and starchy vegetables. Carbs are broken down into glucose and used by our cells as fuel.
- Protein is essential for building and repairing tissues. It’s found in foods like meat, fish, poultry, eggs, dairy products, soy, and beans. It’s made up of amino acids, which are the building blocks of protein.
- Fat is a concentrated source of energy and nourishes our brain and cell membranes. It’s found in foods like oils, nuts, seeds, and avocados. Fats also help absorb vitamins, and play a role in hormone production.
Of course, there’s a lot more to macronutrients than this summary above.
Macro-based diets are designed to meet daily targets for these three macros—often through measuring/weighing foods and calculating their corresponding macros.
Weighing food on a scale using grams provides the most accurate way to account for macros, though measuring cups and spoons work too.
However, for those who want to track macros without the hassle of weighing and measuring your food, our Hand Portion Method is highly effective.
A brief overview of the Hand Portion Method
Precision Nutrition’s Hand Portion Method offers a solution to the inconvenience of tracking your macros, allowing you to manage your food intake without weighing, measuring, or counting calories.
The method is simple: Estimate portion sizes with your hands.
Your hand serves as a reliable gauge for portion sizes because the size of your hand remains constant, ensuring consistency when portioning meals.
Here’s a breakdown:
- The size of your palm represents your protein portion
- The size of your clenched fist represents your vegetable portion
- The amount that can fit in your cupped hand represents your carb portion
- The size of your thumb represents your fat portion
Once you have an idea of how much each portion looks like, you can aim to meet your personalized recommended number of macros daily—in a practical, sustainable way.
The only wrinkle with tracking methods like the hand portion method is that for some foods, it can be hard to figure out which category they fit into. We’ll discuss solutions below.
Macro organizing category guide: Some foods don’t fit perfectly
Food is complex (beans have both carbs and proteins; nuts have both fats and proteins). And, measuring can be complicated (soda can’t follow the cupped hand rule). Yet, if you’re trying to meet your macro goals, what you eat still needs to be accounted for.
We’ll cover some of the most common, tricky-to-categorize foods and provide recommendations for how to account for them.
The key for all of these foods is to pick an approach, and apply it consistently. (This is probably more important than the actual classification itself!)
Tricky macro #1: Legumes (beans and lentils)
Legumes and lentils both contain protein and carbs—so where should they be counted?
Generally, it depends on the meal itself and/or the eating style of the individual.
If someone is fully plant-based/vegan, then it’s likely the legumes or lentils will count as their protein source, since those are probably the most protein-dense foods they’re consuming. But they can also count as both protein and carb, under certain conditions.
Our suggestion: Choose the most protein-rich food (assuming there is one) as your protein source, and categorize the other items from there.
Here are a few examples.
In a meal with…
 Chicken with beans, broccoli and olive oil, chicken is the protein (the most protein-rich part of the dish), beans are the carbs, broccoli is the vegetable, and olive oil is the fat.
Chicken with beans, broccoli and olive oil, chicken is the protein (the most protein-rich part of the dish), beans are the carbs, broccoli is the vegetable, and olive oil is the fat.
 Beans with rice, broccoli and olive oil, beans are the protein (the most protein-rich part of the dish), rice is the carbs, broccoli is the vegetable, and olive oil is the fat.
Beans with rice, broccoli and olive oil, beans are the protein (the most protein-rich part of the dish), rice is the carbs, broccoli is the vegetable, and olive oil is the fat.
 Two servings of beans with broccoli and olive oil, one serving of beans would count as protein, and the other serving would count as carbs.
Two servings of beans with broccoli and olive oil, one serving of beans would count as protein, and the other serving would count as carbs.
 Rice with broccoli and olive oil, there isn’t a protein-rich food—just a carb, vegetable, and fat.
Rice with broccoli and olive oil, there isn’t a protein-rich food—just a carb, vegetable, and fat.
 Beans, broccoli and olive oil, it would depend on the eater. Omnivore? Then we’d count the beans as a carb. Plant-based? Then we’d count the beans as a protein.
Beans, broccoli and olive oil, it would depend on the eater. Omnivore? Then we’d count the beans as a carb. Plant-based? Then we’d count the beans as a protein.
Tricky macro #2: Dairy
Despite being a dietary staple, dairy doesn’t always neatly fit into a macro category.
Cow’s milk and non-Greek yogurt tend to be a pretty even mix of all three macros, but can vary depending on the fat level (whole, low fat, skim).
Ultimately, we suggest categorizing based on the fat or carbohydrate content of the milk or yogurt you’re consuming.
- Generally, consider 1 cup (8 oz) of whole milk products a “thumb” of fat. (Even though it’s larger than a thumb and also provides protein and carbs, it’s fat rich so can be counted as a fat.)
- A cup of lower fat milk (0-2%) is generally considered a cupped hand of carbs (although it also provides fats and protein).
- A portion of lower fat Greek yogurt or cottage cheese (0-2%) is generally considered a palm of protein.
- A cup of anything highly sweetened (chocolate milk, strawberry yogurt) is generally considered a cupped hand of carbs (though it has fats and protein).
So, let’s say you have a full-fat Greek yogurt or whole milk that’s highly sweetened.
Is it a fat or carb??
Think of it this way: If it’s full-fat, you know it’s a thumb of fat. But if there’s also a lot of sugar added to it, then it’s also a cupped hand of carbs.
Tricky macro #3: Dairy Alternatives
Dairy alternatives—nut, soy, or grain milks—are much like products made from cow’s milk. They tend to provide a mix of macros, depending on the source, and classification also depends on whether or not they’re sweetened.
At just 30 to 40 calories for an 8-ounce serving, unsweetened variants like almond milk can almost be considered negligible on macro counts. If you’re just using a splash in coffee or tea, you might just overlook it altogether.
However, this isn’t a universal rule across all dairy alternatives.
For instance, oat, soy, or pea protein milk may have a richer nutrient profile that, even when unsweetened, should be factored in.
Sweetened dairy alternatives introduce another layer of complexity. Added sugars can quickly ramp up the carbohydrate content, and should be categorized as a cupped hand of carbs.
Tricky macro #4: Soda
A serving of soda doesn’t fit into a cupped hand, and a scale isn’t always on hand.
To classify when on the go, consider an average 12-ounce can of soda as a cupped hand of carbs.
Eight ounces might be a preferable serving in terms of sugar content, but 12 ounces simplifies the math, as most beverages come packaged this way.
This is similar to how we account for bananas, apples, oranges, pears, and other fruits, since they’re “pre-packaged” by nature. While they can be standardized, each piece can differ significantly in its macro content.
Estimating is okay. By frequently comparing actual measurements with visual estimations, we can train ourselves to be more accurate over time.
Tricky macro #5: Alcohol
Alcohol generally should be in its own category, as the majority of its calories are derived from fermentation from starch and sugar.
This applies to pretty much all alcohol, be it light beer, microbrew/craft beer, wine, and spirits (although some microbrews/craft beer and dessert wines can contain quite a few carbs).
Many folks like to put alcohol in the carb category, which works. Again, whatever method you prefer can work; just follow it consistently.
Note that most alcohol is about 100-150 Calories per serving. If it has a sweetened additive (think margarita, or alcohol + soda), count that as an additional cupped hand of carbs.
How to account for mixed-food meals
With the tricky food out of the way, it’s time to discuss mixed food, like soups, salads, chili, casseroles, curries, and more.
Since these types of foods are technically several foods put together, they naturally have a mix of macros.
Our advice: Eyeball it.
Make your best guess at the proportion of protein-rich foods, carb-rich foods, and fats. This isn’t a full-proof method, but the key is consistency. If you categorize chili one way one day, do the same the next day.
With mixed meals, the goal is to get a protein, veggie, quality carb, and/or healthy fat in each portion.
This is relatively easy to do when making it yourself, as you can weigh each ingredient to calculate the macros and then divide by the total portions. When made by others, simply guesstimate as well as you can.
Tip: If a mixed meal—like chili or soup—is low in any particular macronutrient, you can always add a side dish to fill the gap.
We can support you on your fitness journey
If you’re just getting started with macros, take a moment to explore Precision Nutrition’s Ultimate Macro Calculator.
This interactive tool can help you determine your ideal calorie and macronutrient intake based on your individual goals and needs to create a personalized plan—no expertise on the carb content of beans required.
The post What do I do with foods that don’t easily fit my macros? appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
Are there “good” and “bad” fats?
And how much fat, exactly, should a health-conscious person strive to eat?
In this article, we’ll talk all about fats, including the effects of certain fats on your health, plus how fats work in your body.
What is fat?
Fat, an essential macronutrient, plays a crucial role in maintaining the proper functioning of your body.
Fat is a concentrated energy source which contains more calories per gram than either carbohydrates or protein. (Fat contains 9 Calories per gram, whereas carbs and proteins contain 4 Calories per gram.) This energy supports your daily activities.
Fat also plays a pivotal role in your body’s ability to absorb specific vitamins and minerals, ensuring you get the most out of the nutrients you consume.
Fatty acids
All fats are made up of fatty acids.
These tiny building blocks are classified into three main categories: saturated, polyunsaturated, and monounsaturated. We’ll discuss each in more detail below.
Unsaturated fats
These fats, sometimes referred to as “healthy fats,” are your allies in the quest for a healthier lifestyle.
Monounsaturated fats in foods like avocados and olive oil are known for their heart health benefits.
Polyunsaturated fats, the dynamic duo of omega-3s and omega-6s found in nuts, seeds, and fish, help regulate inflammation and support brain health, and by extension, overall well-being.
Saturated fats
These fats, which are often solid at room temperature, are commonly found in animal products like butter and fatty cuts of meat, as well as plant foods like coconut and chocolate.
While they’re essential for some bodily functions, it’s wise to consume them moderately. High intake—over 10 percent of your daily calories—of saturated fats has been linked to higher cholesterol, and an increased risk of certain diseases.
What are trans fats?
Trans fats are created when liquid oils transform into solid fats through a manufacturing process called hydrogenation.
While trans fats enhance shelf life, they can wreak havoc on your health. Trans fats can raise bad cholesterol and increase heart disease risk. These are the only fats that we can confidently say are “bad” for health, and should be minimized or avoided.
Why is some fat considered healthy, and some unhealthy?
Not all fats are created equal.
Let’s go into some of the nuances of unsaturated and saturated fats.
The benefits of unsaturated fats
Unsaturated fats, on the other hand, actively contribute to your well-being.
Some of the ways these fats can help your body include:
- Monounsaturated and polyunsaturated fats may help lower bad cholesterol, and boost good cholesterol, creating a harmonious balance that supports cardiovascular health.
- Unsaturated fats work to quell inflammation in your body, reducing the risk of chronic diseases and fostering overall health.
- By providing steady, sustained energy and promoting satiety, whole foods rich in unsaturated fats can help maintain a healthy weight.
- Unsaturated fats assist in improving insulin sensitivity, reducing your risk of diabetes.
- Monounsaturated and polyunsaturated fats (especially omega-3s) are like brain food, promoting cognitive function and stable moods.
In other words, incorporating sources of unsaturated fats into your diet—from foods such as avocados, nuts, seeds, and olive oil—help support a healthier you.
What to consider when it comes to saturated fats
Unsaturated fats may, on the whole, offer more health benefits than saturated fats.
But that doesn’t mean saturated fats are inherently unhealthy.
Excess saturated fats are known to raise levels of LDL cholesterol, often referred to as the “bad” cholesterol. This can create a risk factor for heart disease, jeopardizing your cardiovascular health.
Moderating your intake of saturated fats—often found in red meat, full-fat dairy products, coconut, chocolate, and certain processed foods—can be a smart move for your long-term health. Most research suggests limiting saturated fats to about 10 percent of your daily calories.
The role of fat in your diet
What effect does fat have on your overall health? What does it do inside your body?
Let’s find out.
Role #1: Cell development
From infancy to maturity, your body’s cells depend on fatty acids for cellular development.
Omega-3 and omega-6 fatty acids are like the architects of your cell membranes. They determine the structure and function of these cellular gatekeepers, influencing what goes in and out.
Omega-3s, found in fatty fish like salmon and flaxseeds, work to keep inflammation in check. This helps prevent chronic diseases, plus supports overall health.
Omega-6s, abundant in sources like vegetable oils and nuts, orchestrate pro-inflammatory responses when needed. This doesn’t mean they’re bad; These controlled inflammations play crucial roles in healing and immune responses.
Role #2: Overall health
The right fats, particularly those in the unsaturated category, can shield you from some major health challenges.
Healthy fats help your heart. Emphasizing monounsaturated and polyunsaturated fats, moderating saturated fats, and avoiding trans fats promotes healthy cholesterol levels, and reduces the risk of blockages that lead to heart attacks.
You can also minimize your risk of stroke with your fat choices. Unsaturated fats contribute to good blood flow and prevent blood clots.
Role #3: Nervous system
Picture your nervous system as a complex communication network, and healthy fats as the high-speed data cables that keep it running seamlessly.
From the crown of your head to the tips of your fingers, fats ensure the smooth functioning of your brain and nervous system.
As the control center, your brain is a fat-rich organ, with nearly 60% of its structure composed of fats. (Omega-3 fatty acids are especially known for their brain-boosting abilities: They enhance cognitive function, support memory, and even contribute to mood regulation.)
Myelin, a protective sheath that covers nerve fibers, is predominantly composed of fats. This insulation ensures that signals are transmitted accurately and efficiently throughout your nervous system.
Role #4: Hormone health and function
Hormones serve as messengers in the body, and they influence a number of critical metabolic processes including (but not limited to) weight regulation, digestive health, skin quality, ovulation and reproduction, sleep, and energy levels.
Since hormones are made from a combination of fats and cholesterol, it’s crucial to include enough fat in your diet to support hormone production.
This is specifically important for sex hormones such as testosterone, estrogen, and progesterone. If dietary fat and cholesterol are too low, these hormones may stop being produced in optimal quantities, and you may experience symptoms of hormonal deficiencies.
Role #5: Source of micronutrients
Many minimally-processed fat sources also supply a slew of beneficial micronutrients and phytonutrients.
Avocados, for example, are a great source of fiber, magnesium, vitamin E, B vitamins, and folic acid. Nuts and seeds provide omega-3 fatty acids, fiber, and other beneficial compounds.
Role #6: Vitamin absorption
Fats don’t just provide crucial vitamins and minerals, they also facilitate the absorption of fat-soluble vitamins A, D, E, and K.
Vitamin A—vital for vision, immune function, and skin health—depends on fats to be metabolized and used in the body.
Vitamin D, often called the “sunshine vitamin,” is crucial for bone health, immunity, and more. But sunlight alone isn’t enough—fats are the facilitators that help your body absorb and use it effectively.
Vitamin E, a powerful antioxidant, thrives in the presence of fats. It reduces oxidative stress and inflammation, and protects the health of your cells.
Vitamin K, essential for blood clotting and bone health, benefits from fats, too. They assist in its absorption, ensuring it’s available when your body needs it.
How to incorporate more unsaturated fats into your diet
If you want to boost your intake of unsaturated fats to reap their benefits, a few strategic changes to your eating habits can help:
- Embrace monounsaturated fats: Foods like olive oil, avocados, nuts, and seeds are your go-to sources of monounsaturated fats. Drizzle extra-virgin olive oil on salads, add slices of avocado to your sandwiches, and sprinkle nuts or seeds onto your morning yogurt for a delightful crunch.
- Avoid trans fats: To get the best balance of dietary fats, minimize processed foods with trans fats. These artificially created fats can negatively impact your health, so read labels and opt for whole, minimally-processed options instead.
- Seek out omega-3-rich foods: Omega-3 fatty acids boost brain function and fight excess inflammation. Salmon (and other fatty fish), flaxseeds, chia seeds, and walnuts are rich sources. Aim to include them in your meals a few times a week.
- Moderate saturated fat sources: While some saturated fats are necessary and even beneficial, it’s wise to keep their intake in check. Limit red meat and butter consumption, opting for leaner cuts of meat and small to moderate amounts of butter.
- Sprinkle in flavor and support satiety: A drizzle of olive oil on your vegetables, a sprinkle of nuts on your oatmeal, or a dollop of nut butter on your whole-grain toast can enhance both flavor and appetite regulation— without exceeding daily calorie requirements.
We can support you on your fitness journey
If you’re wondering where exactly to start, or how much fat you should be incorporating into your diet, we’re here to help.
Creating a nutrition and fitness plan can be daunting, but you don’t have to do it alone. Our Ultimate Macro Calculator can help you figure out the optimal proportions of all the macronutrients—fats, carbohydrates, and protein—that you need to meet your goals.
Precision Nutrition can help you build habits that improve your physical and mental health, bolster your immunity, help you manage stress, and get sustainable results.
The post All about fats appeared first on Precision Nutrition.
Source: Health1
Reviewed by Brian St. Pierre, MS, RD
Growing up, we learn that vitamins and minerals are essential for health.
(We all took those animal-shaped multis, right?)
But what does that mean?
What vitamins do we need, and why?
How can we get the minerals our body needs for optimal health and well-being?
In this article, we’ll take a detailed look at vitamins and minerals, where they come from, what they do, and what happens if you don’t get enough or too many of them.
What are micronutrients?
Micronutrients are the vitamins and minerals your body needs in smaller quantities (as opposed to macronutrients, which are needed in larger quantities).
Your body can’t produce micronutrients, so you must rely on your meals to give you what you need. That’s why they’re also known as “essential nutrients.”
Vitamins are found in plants and animal products and can be broken down or altered by heat, acid, or air.
In contrast, minerals are inorganic, originate from soil or water, and cannot be broken down.
When you eat, you’re consuming the vitamins produced by plants and animals and the minerals they’ve absorbed. Each food item carries a unique micronutrient load, so it’s important to eat a wide variety of foods. (We’ll discuss later which foods are best for getting which micronutrients.)
Vitamins and minerals fuel growth, bolster your immune system, and even shape your brain’s development.
Types of micronutrients and what they do
There are four categories of micronutrients, defined by what they are and how they work in your body.
Water-soluble
Water-soluble vitamins readily dissolve in water, then your body uses what it needs. Whatever’s left is excreted (through urine and sweat, primarily), not stored.
The water-soluble micronutrients include Vitamin C and the eight B Vitamins: B1, B2, B3, B5, B6, B7, B9, and B12.
Fat-soluble
Unlike water-soluble micronutrients, fat-soluble vitamins are stored within the liver and fatty tissues.
To be absorbed, fat-soluble vitamins must be consumed with dietary fats.
The fat-soluble micronutrients are Vitamins A, D, E, and K. These aid in fortifying the immune system, proper bone development, preserving eye health, and shielding cellular structures from harm.
While it’s usually best to get these vitamins from food sources, if you suspect a deficiency, ask your doctor about whether you should take a supplement. Taking supplements without consulting a doctor is riskier, as fat-soluble vitamins can accumulate in the body. (We’ll discuss the possible effects of that later.)
Macrominerals
Macrominerals get their name because they’re required in larger quantities than other micronutrients and serve many vital functions.
The macrominerals are:
- Calcium
- Chloride
- Magnesium
- Phosphorus
- Potassium
- Sodium
- Sulfur
Trace Minerals
While your body doesn’t need these in large quantities, trace minerals significantly affect your overall health and are essential for various bodily functions.
The trace minerals include iron, manganese, copper, zinc, iodine, fluoride, and selenium.
Why are micronutrients important?
Micronutrients are necessary for proper bodily functions.
For example, folate (Vitamin B9) plays a pivotal role in genetic material creation, cell division, and birth defect prevention.
Calcium fortifies bones, aids circulatory function, and supports nerve activity and hormonal secretion. Iodine impacts cognitive development and thyroid health.
Antioxidant micronutrients—Vitamins A, C, and E, along with copper, zinc, and selenium—shield the body from oxidative stress caused by free radicals. In excess, these free radicals—produced from normal metabolic processes—can harm tissues, organs, and genetic material.
Micronutrients in growth and development
In children, micronutrients are absolutely essential for growth because they support brain and immune system development. They also act as catalysts for metabolic reactions and regulate fluid balance.
Micronutrients and physical performance
While macronutrients are often at the forefront of dietary considerations for athletes and fitness enthusiasts, micronutrients also play a pivotal role.
For example, electrolytes (sodium, potassium, and calcium) help prevent dehydration and replenish salts lost from excessive sweating.
Efficient micronutrient intake before, during, and after exercise:
- Supports blood glucose regulation and healthy muscle glycogen levels
- Enhances endurance, strength, and recovery
- Aids protein synthesis and immune function
Athletes also need to pay attention to:
- Antioxidants like Vitamins C, E, and beta-carotene (which converts in the body to Vitamin A), which protect cells from exercise-induced oxidative stress
- B Vitamins, which improve energy production and metabolism
- Vitamin D, which enhances muscle function and physical performance. Getting enough Vitamin D is especially important for indoor athletes and those in regions with limited sun exposure
- Avoiding mineral deficiencies (especially in calcium, magnesium, iron, zinc), which impact bone health, muscle performance, and metabolic processes.
Micronutrients and weight management
Individuals hoping to lose weight must maintain their micronutrient intake even if they cut calories.
Although micronutrients do not induce weight loss directly, micronutrients like zinc, magnesium, and chromium play supportive roles in the weight loss process: Low levels of zinc cause the body to store extra fat; Magnesium helps maintain a healthy metabolism; Chromium helps keep blood sugar levels under control.
Ideally, try to obtain these micronutrients by consuming a variety of minimally-processed foods, rather than relying solely on supplements.
Vitamins and minerals are more potent when they come from food, and our bodies process them more efficiently than through supplements,
Micronutrients in cellular health and immunity
Micronutrients influence enzymatic activity—they promote healthy tissues and prevent excessive free radical damage, which also helps protect DNA and reduces the risk of many diseases.
Additionally, micronutrients like Vitamins B6, C, and E, as well as magnesium and zinc, fortify the immune system, enhancing barriers against pathogens and infection-fighting mechanisms.
Micronutrients and overall health
Zinc is a micronutrient that helps maintain overall health. It’s distributed within various cells across your body, playing a pivotal role in bolstering your immune system against bacteria and viruses.
Zinc is also instrumental in synthesizing DNA and producing essential proteins. Throughout pivotal stages such as pregnancy, infancy, childhood, and adolescence, a sufficient supply of zinc helps with growth and development.
Finally, this micronutrient aids in effectively healing wounds and is fundamental for ensuring a keen sense of taste.
Best sources for micronutrients
Obtaining micronutrients from diverse food sources promotes optimal health. Here are some of the best sources for getting the micronutrients you need.
Food sources of water-soluble vitamins
- Vitamin C (ascorbic acid): Citrus fruits, kiwi, bell peppers, broccoli, strawberries, and tomatoes.
- Vitamin B1 (thiamine): Found in whole grains, fortified cereals, pork, beef, trout, tuna, and black beans.
- Vitamin B2 (riboflavin): Eggs, beef liver, milk, yogurt, cheese, fortified cereals, almonds, and clams.
- Vitamin B3 (niacin): Chicken, turkey, beef, pork, salmon, tuna, peanuts, potatoes, and rice.
- Vitamin B5 (pantothenic acid): Beef, chicken, organ meats, whole grains, shiitake mushrooms, sunflower seeds, and avocado.
- Vitamin B6 (pyridoxine): Chickpeas, beef liver, turkey, tuna, salmon, chicken, fortified cereals, potatoes, and bananas.
- Vitamin B7 (biotin): Organ meats, eggs, salmon, pork, beef, sunflower seeds, almonds, and sweet potatoes.
- Vitamin B9 (folate): Beef liver, spinach, fortified cereals and grains, asparagus, brussels sprouts, beans, and nuts.
- Vitamin B12 (cobalamin): Beef liver, nutritional yeast, fatty fish (salmon, tuna), clams, beef, dairy products, and eggs.
Food sources of fat-soluble vitamins
- Vitamin A: Beef liver, fish, eggs, fortified dairy products, sweet potatoes, carrots, and cantaloupe.
- Vitamin D: Fatty fish like trout, tuna, salmon, fish liver oils, egg yolks, fortified milk, and UV light-exposed mushrooms.
- Vitamin E: Nuts (almonds, hazelnuts), seeds, vegetable oils, spinach, and broccoli.
- Vitamin K: Leafy greens (collard greens, spinach, kale, broccoli), vegetable oils, blueberries, and pomegranate juice.
Food sources of macrominerals
- Calcium: Dairy products, fortified orange juice, canned sardines and salmon with bones, tofu, soybeans, spinach, and kale.
- Magnesium: Spinach, pumpkin seeds, chia seeds, almonds, cashews, peanuts, soy milk, black beans, potatoes, and brown rice.
- Phosphorus: Dairy products, salmon, chicken, beef, scallops, lentils, potatoes, and kidney beans.
- Potassium: Dried apricots, lentils, prunes, raisins, potatoes, oranges, bananas, and acorn squash.
- Sodium: Salts and processed foods like bread, deli meats, frozen meals, canned foods, chips, and salted popcorn.
- Sulfur: Broccoli, cabbage, cauliflower, onions, garlic, dairy products, fish, legumes, nuts, meats, raspberries, and wheat germ.
Food sources of trace minerals
- Copper: Shellfish, seeds, nuts, organ meats, whole grains, chocolate, potatoes, and mushrooms.
- Chromium: Beef, pork, turkey, brewer’s yeast, grape and orange juice, and grain products.
- Fluoride: Brewed tea and coffee, shrimp, and water with added fluoride.
- Iodine: Iodized salt, seaweed, fish, eggs, cheese.
- Iron: Beef, pork, turkey, fish, fortified cereals and grains, spinach, tofu, lentils, beans, and dark chocolate.
- Manganese: Whole grains, clams, oysters, mussels, nuts, soybeans, legumes, rice, coffee, tea, and leafy green vegetables.
- Molybdenum: Legumes, whole grains, nuts, beef liver, milk, and yogurt.
- Selenium: Brazil nuts, fish, shrimp, organ meats, fortified cereals, beef, turkey, chicken, and dairy products.
- Zinc: Found in beef, oysters, blue crab, fortified cereals and grains, pumpkin seeds, turkey, cheese, and shrimp.
To meet your micronutrient needs, prioritize nutrient-dense foods while maintaining a balanced calorie intake. For optimal health, moderate your sodium, saturated fat, added sugars, and alcohol consumption.
What happens if you don’t have enough micronutrients?
Getting enough micronutrients for each stage and phase of your life is important.
How much you need of each will depend on how much you exercise, your gender-assigned-at-birth, weight, and several other factors. Not getting enough is called a deficiency.
Diets high in highly-processed foods, disordered eating, and malabsorption conditions like Crohn’s disease can contribute to deficiencies.
The impact of these deficiencies isn’t always visible; some signs of micronutrient deficiencies are more subtle, like decreased energy and mental sharpness. These often result in hindered learning, reduced work productivity, and heightened susceptibility to infections and diseases.
Some of the most common micronutrient deficiencies and their symptoms include:
- Vitamin A deficiency: Night blindness, impaired vision, stunted growth
- Biotin deficiency: Metabolic acidosis, dermatitis, seizures
- Vitamin C deficiency: Bleeding gums, petechiae, impaired wound healing
- Calcium deficiency: Cataracts, osteoporosis, dental changes
- Vitamin D deficiency: Muscle weakness, bone pain, low mood
- Vitamin E deficiency: Ataxia, myopathy, vision impairment
- Fluoride deficiency: Weakens teeth and bones, and increases tooth decay
- Folate deficiency: Weakness, difficulty concentrating, heart palpitations
- Iodine deficiency: Goiters, intellectual disabilities, feeling cold
- Iron deficiency: Fatigue, pale skin, dizziness, cold extremities
- Vitamin K deficiency: Slower blood clotting, hemorrhagic diseases
- Potassium deficiency: Irregular heartbeat, muscle weakness
- Selenium deficiency: Cardiomyopathy, deforming arthritis
- Zinc deficiency: Diarrhea, hair loss, delayed growth
To prevent deficiencies, eat a balanced diet rich in diverse sources of these vital micronutrients. Fortified foods—and supplements, with your doctor’s approval—can also bridge the gap.
What happens if you have too many micronutrients?
While less common than micronutrient deficiencies, consuming too many micronutrients is possible.
This is called toxicity. It’s much more likely to happen when taking supplements, so speak with your doctor about safe use.
Some of the most common micronutrient toxicities and their symptoms include:
- Vitamin A toxicity: Dizziness, nausea, and, in severe cases, bone pain and blurred vision
- Calcium toxicity: Kidney stones, constipation, and kidney damage
- Vitamin D toxicity: Nausea, vomiting, and weakness
- Vitamin E toxicity: Excessive bleeding
- Vitamin K toxicity: Disruption of blood clotting
- Iron toxicity: Damage to the lining of the stomach and intestines, vomiting, stomach ache, loose stools, and hypovolemia
- Selenium toxicity: Nausea, vomiting, discoloration, brittleness, and loss of nails, loss of hair, fatigue, irritability, and foul breath odor
- Zinc toxicity: Vomiting, hematemesis, nausea, muscle cramps, watery diarrhea, and abdominal pain
Build a healthy diet with Precision Nutrition
A healthy, well-balanced diet full of nutritious food is your key to overall wellness.
If you want help building an optimal nutrition plan to support your specific goals, try our 1:1 coaching program. You’ll be paired with your own expert coach, who will help you determine your ideal dietary pattern—and help you sustain it.
Whatever your health goals, Precision Nutrition is here to help you reach them.
The post The importance of micronutrients—and where they fit in your diet appeared first on Precision Nutrition.
Source: Health1
Massive industry-wide survey reveals the personality characteristics linked to phenomenal success in the health and fitness industry.
The post Caliper | Personalities and Behaviors of Successful Health and Fitness Pros [Free PDF] appeared first on Precision Nutrition.
Source: Health1
