The truth about adrenal fatigue.
Reviewed by Helen Kollias, PhD
What is adrenal fatigue? | Symptoms | Science | Treatment
Every month, roughly 80,000 people type “what is adrenal fatigue?” into a search bar, hoping for answers.
And the internet gives them plenty. (About 17 million, give or take.)
Click on any number of these offerings and you can read a super-convincing theory about how adrenal fatigue works.
That line of reasoning goes like this:
Prolonged stress or illness overworks your adrenal glands. Eventually, your glands fatigue, and sleep disruptions, cravings, brain fog, exhaustion, and other symptoms set in.
According to certain people on the interwebz, expensive supplements, restrictive eat-this-not-that diet lists, and essential oil blends can turn this sad state of affairs around.
If you’re desperate for help, this adrenal-fatigue theory can seem like manna from Heaven.
Except it’s not true, as we’ll explain below.
Unfortunately this misinformation prevents people from understanding what’s really going on.
In this article, we’ll help you sort the facts from the fiction. By the end, you’ll know the real cause of these symptoms—as well as evidence-based strategies that actually work.
What is adrenal fatigue?
To fully understand adrenal fatigue theory, you need a quick anatomy lesson.
At the top of each of your kidneys, you have an adrenal gland that releases an array of hormones. One of those hormones, cortisol, gets you out of bed, regulates blood pressure, and snaps you to attention during an emergency, among other things.
According to adrenal-fatigue theory, too much stress causes the adrenals to stop functioning properly.
They either don’t generate enough cortisol, or they produce it at the wrong times (like when you’re trying to sleep).
This then leads to symptoms like:
- feeling tired and lethargic
- poor healing and recovery
- aches and pains
- having salt or sugar cravings
- having trouble falling asleep or waking up
- relying on caffeine to get through the day
Those are all real problems. We’re guessing you’ve experienced one (or all) of them. Or you know someone who has. (Because why else would you be reading this story?)
Is adrenal fatigue real?
The truth: There isn’t much evidence in favor of the adrenal fatigue theory.
But there is quite a bit of evidence that refutes it.
After carefully examining 58 different studies, researchers from Brazil found that, in most people tested for adrenal fatigue, cortisol levels were… normal. In other words, their adrenal glands were anything but depleted.1
They concluded: “Adrenal fatigue does not exist.” (Pretty clear where these scientists stand!)
Sure, if you dig around PubMed long enough, you’ll find a few studies that claim to support the adrenal fatigue theory.
Those studies tend to measure fatigue levels—rather than actual adrenal function. In other words, they show that fatigue exists, but not necessarily adrenal fatigue.
So why do so many people swear that adrenal fatigue exists?
That’s probably because their so-called adrenal fatigue symptoms are very real, common—and frustrating.
Tiredness is one of the top reasons people seek medical care. It plagues a lot of folks.2
For most of those people, stress—and not adrenal fatigue—is the more likely problem. (More about this below).
Yet there’s no easy medical test for stress.
There are, however, a wide range of tests for the dozens of complex medical conditions that can also lead to fatigue, including thyroid issues, sleep apnea, and anemia.
This can leave people in a situation where they continually tell their doctors about how crummy they feel.
So their doctors order more tests that reveal nothing out of the ordinary, which can make patients feel unheard and misunderstood.
When someone’s not getting the answers they need, adrenal fatigue theory becomes super attractive.
Adrenal insufficiency
Many people confuse adrenal fatigue with adrenal insufficiency (AI).
However…
Adrenal insufficiency is a recognized medical diagnosis.3
In AI, the adrenal glands don’t produce their full roster of hormones.
This includes cortisol as well as aldosterone (which regulates salt and water balance), DHEA (a “master” hormone necessary for testosterone and estrogen production), plus others.
AI can result from Addison’s disease, a condition where the adrenal glands are physically damaged, often due to an autoimmune reaction where the body attacks its own healthy tissue.
Or, it can result from hormonal signalling problems. Meaning, the hormonal signals from the pituitary or hypothalamus aren’t communicating properly with the adrenal glands.4, 5
The symptoms of AI are typically more severe than those proposed in “adrenal fatigue.”
They include:
- weight loss and loss of appetite
- significant joint pain
- stomach pain and upset
- dry skin
- disrupted electrolytes (like sodium and calcium)
- low blood pressure
- major fatigue
- hyperpigmentation (darkened areas of skin)
Adrenal insufficiency can only be diagnosed and treated by a medical doctor.
Stress: The real reason you feel so awful
Here’s what the proponents of adrenal fatigue get right: Stress is a real problem—for a lot of people.
Chronic stress doesn’t just affect the adrenal glands.
Our stress response is a whole-body experience, affecting the nervous, digestive, and immune systems, among many other parts of the body.
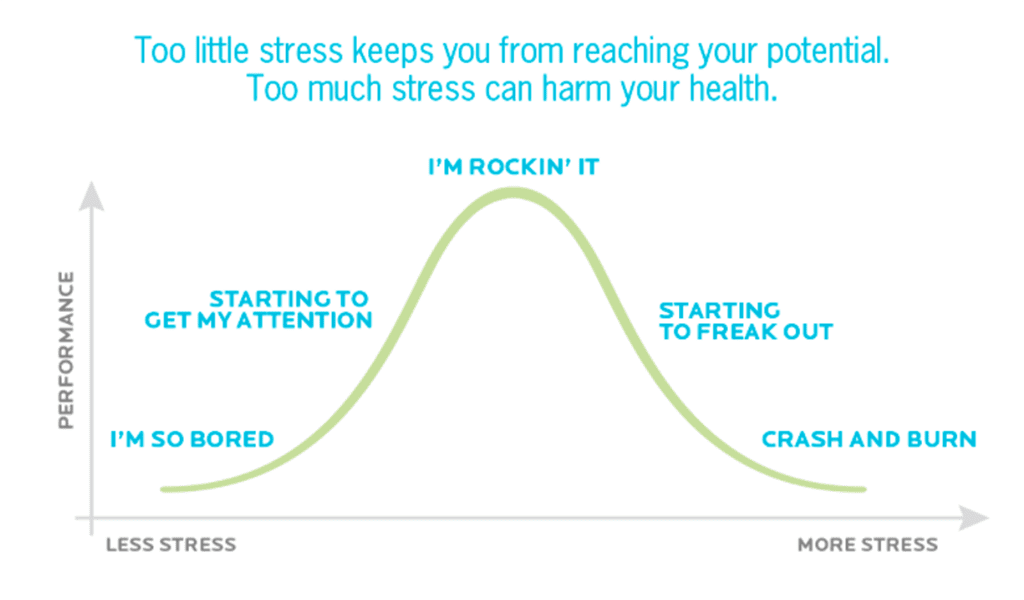
Short bouts of stress followed by adequate recovery are no big deal. In fact, that’s how we grow stronger.
If that stress is ongoing and there’s not enough recovery, however, the body starts to break down.
Consider what might happen if you hoisted heavy dumbbells… forever. You wouldn’t get stronger; you’d get weaker.
And that’s what happens when you’re under unrelenting stress, even low-level stress. Chronic stress without respite feels terrible, head-to-toe, as the graphic below shows.
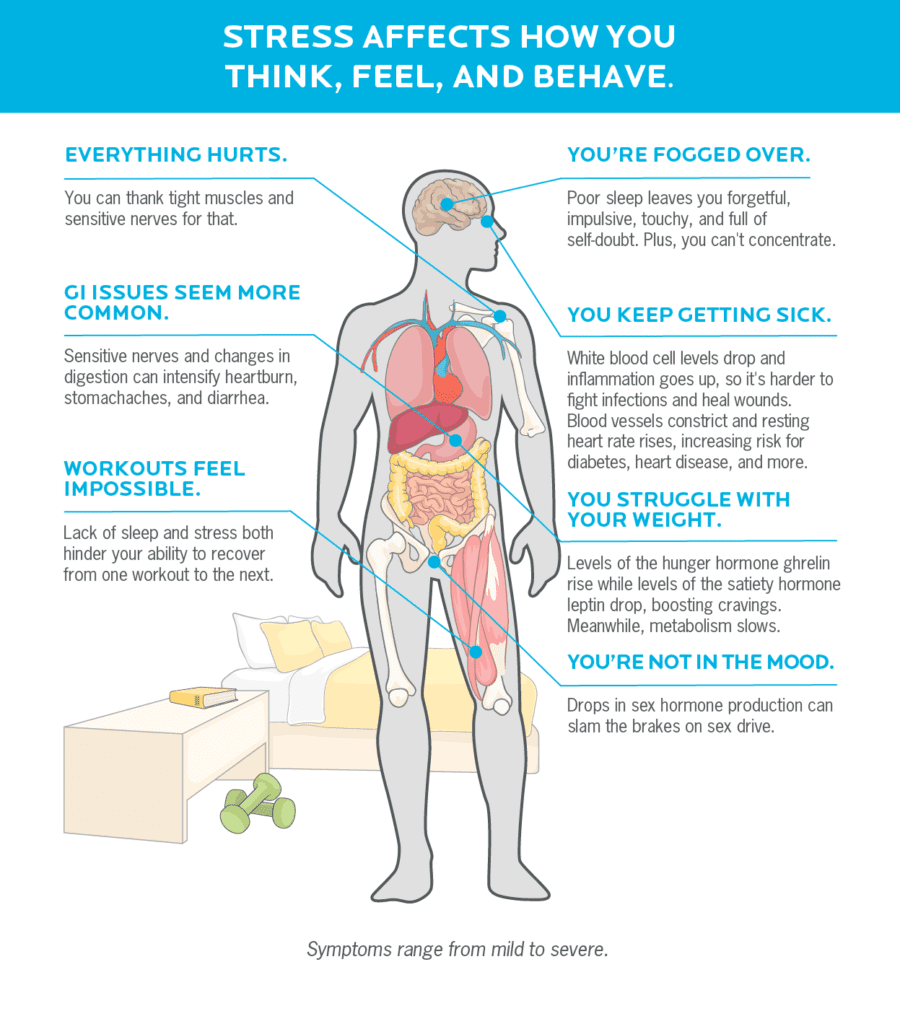
If you’re experiencing these symptoms, check with your doctor to rule out any medical conditions.
If you leave with a clean bill of health, you may be suffering from the consequences of unrelenting stress, without adequate recovery. Luckily, simple, accessible practices can help.
Reduce stress that’s within your control.
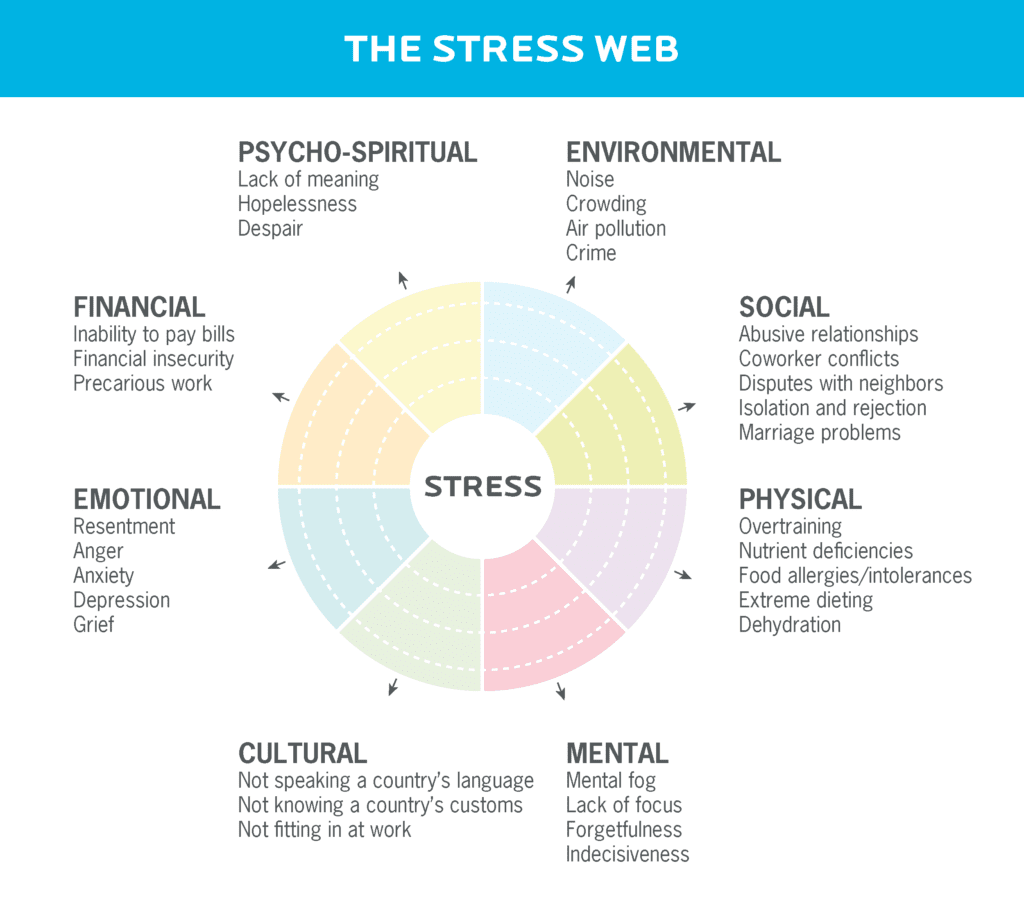
It’s not realistic (or even ideal) to obliterate all stress. But you can turn some stressors down a few notches. Your first step: Identify your areas of stress, using the Stress Web, below, as a guide.
Consider your stress level for each area of the web.
To make this easy, you might download and print out the web so you can color in the areas based on how much stress they deliver.
Let’s say you’re training hard in the gym several days a week. Then you might color in all four sections of the physical part of the circle.
On the other hand, maybe you’re not dealing with any of the financial stressors. In that case, you might not color any of those in.
Once you see which areas pose the most stress, brainstorm ways to reduce those areas of stress.
And know that it’s not always about the big things.
For example, our client, Zahra, noticed that her environmental and mental dimensions of the stress web were particularly high.
After some thought, she made a couple changes. She:
 bought noise-cancelling headphones to drown out her household
bought noise-cancelling headphones to drown out her household
 installed apps on her computer to block certain websites during periods of the day
installed apps on her computer to block certain websites during periods of the day
Those strategies allowed her to cut down on unproductive distractions and focus on her work tasks.
After a month, Zahra was feeling more clear-headed, and actually started enjoying her workday more. Plus, she had way more energy. She hadn’t realized how depleting all those competing distractions had been.
Jack up recovery, in multiple areas of your life.
The more stress we deal with, the more we need to prioritize recovery.
Think of your “mojo reserve” as a jug: Stress drains it, and recovery fills it back up.
Try to fill your jug at least as much as you drain it.
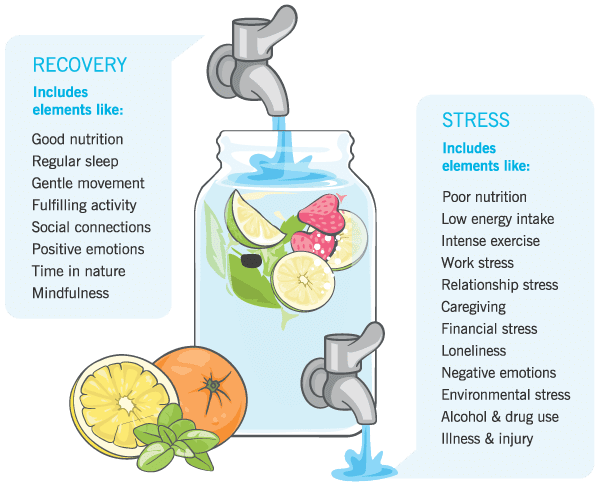
Recovery can take many forms. In working with over 100,000 clients, however, we’ve noticed that the following three practices offer an enormous impact.
Eat a nutrient-packed diet
Consume enough calories to support your body and activity levels, with a balance of macronutrients (including carbs!).
Bonus points if you can eat slowly and mindfully. (Here’s why slow eating is way better than dieting: The 30-day eating challenge that can transform your body.)
For more specific recommendations check out our Nutrition Calculator. Plug in some basic info, and it’ll give you a personalized nutrition plan based on YOUR body, lifestyle, and goals.
Get appropriate levels of exercise
If your intense spin or CrossFit sessions feel more like they’re breaking you down than building you up, lower the intensity and/or duration.
Schedule in recovery days, and consider replacing some of your more intense training sessions with gentle, restorative movement that activates the parasympathetic “calming” nervous system. Think: yoga, tai chi, walks in nature (or “forest-bathing” if you prefer!), stretching, and foam rolling.
Form good sleep habits
While we can’t force ourselves to fall asleep on cue, we do have a lot of control over our sleep hygiene—the habits and routines we engage in around sleep.
Experiment with the following strategies and see what works for you:
- Power down devices 30 minutes before bed
- Use a journal to write down thoughts, worries, and reminders before turning off the lights
- Turn down the thermostat a degree or two
- Take a hot shower or bath before bed
- Sleep alone, so you’re not disturbed by your partner or pets
Remember, “experiment” means to try it. Any individual practice may or may not be useful. But you won’t ever really know unless you make a concerted effort to give it a shot.
You can always decide to stop doing it if it doesn’t make a difference. In fact, at PN, when we make a change or try something new, we like to say, “It’s forever for now.”
Adopting this “nothing has to be permanent” mindset might help you (or your clients) be more open to experimentation.
(For a visual guide on how to engineer your life for better sleep, check out: The power of sleep).
You can build stress muscles.
When you face stressful events—with a strong mindset, relationships, and recovery practices—you grow stronger.
If you’ve been stuck in a downward spiral, small improvements can give you some much needed energy, and hope for a better future.
Eventually, stress can feel like surfing: Challenging and dynamic, without pulling you under.
jQuery(document).ready(function(){
jQuery(“#references_link”).click(function(){
jQuery(“#references_holder”).show();
jQuery(“#references_link”).parent().hide();
});
});
References
Click here to view the information sources referenced in this article.
1. Cadegiani FA, Kater CE. Adrenal fatigue does not exist: a systematic review. BMC Endocr Disord. 2016 Aug 24;16(1):48.
2. Stadje R, Dornieden K, Baum E, Becker A, Biroga T, Bösner S, et al. The differential diagnosis of tiredness: a systematic review. BMC Fam Pract. 2016 Oct 20;17(1):147.
3. Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and Treatment of Primary Adrenal Insufficiency: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016 Feb;101(2):364–89.
4. Charmandari E, Nicolaides NC, Chrousos GP. Adrenal insufficiency. Lancet. 2014 Jun 21;383(9935):2152–67.
5. Husebye ES, Allolio B, Arlt W, Badenhoop K, Bensing S, Betterle C, et al. Consensus statement on the diagnosis, treatment and follow-up of patients with primary adrenal insufficiency. J Intern Med. 2014 Feb;275(2):104–15.
If you’re a health and fitness coach…
Learning how to help clients manage stress, build resilience, and optimize sleep and recovery can be deeply transformative—for both of you.
It helps clients get “unstuck” and makes everything else easier—whether they want to eat better, move more, lose weight, or reclaim their
health.
And for coaches: It gives you a rarified skill that will set you apart as an elite change maker.
PN’s brand-new certification—announcement coming soon!—will show you how.
Want to know more?
The post The truth about adrenal fatigue. appeared first on Precision Nutrition.
Source: Health1